Abstract
Objectives
The aim of this review is to highlight recent progress in the field of biomaterials-mediated dental pulp tissue engineering. Specifically, we aim to underscore the critical design criteria of biomaterial platforms that are advantageous for pulp tissue engineering, discuss models for preclinical evaluation, and present new and innovative multifunctional strategies that hold promise for clinical translation.
Materials and methods
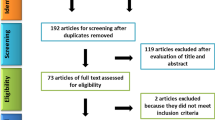
The current article is a comprehensive overview of recent progress over the last 5 years. In detail, we surveyed the literature in regenerative pulp biology, including novel biologic and biomaterials approaches, and those that combined multiple strategies, towards more clinically relevant models. PubMed searches were performed using the keywords: “regenerative dentistry,” “dental pulp regeneration,” “regenerative endodontics,” and “dental pulp therapy.”
Results
Significant contributions to the field of regenerative dentistry have been made in the last 5 years, as evidenced by a significant body of publications. We chose exemplary studies that we believe are progressive towards clinically translatable solutions. We close this review with an outlook towards the future of pulp regeneration strategies and their clinical translation.
Conclusions
Current clinical treatments lack functional and predictable pulp regeneration and are more focused on the treatment of the consequences of pulp exposure, rather than the restoration of healthy dental pulp.
Clinical relevance
Clinically, there is great demand for bioinspired biomaterial strategies that are safe, efficacious, and easy to use, and clinicians are eager for their clinical translation. In particular, we place emphasis on strategies that combine favorable angiogenesis, mineralization, and functional tissue formation, while limiting immune reaction, risk of microbial infection, and pulp necrosis.















Similar content being viewed by others
References
Schmalz G, Smith AJ (2014) Pulp development, repair, and regeneration: challenges of the transition from traditional dentistry to biologically based therapies. J Endod 40(4 Suppl):S2-5. https://doi.org/10.1016/j.joen.2014.01.018
Orti V, Collart-Dutilleul PY, Piglionico S, Pall O, Cuisinier F, Panayotov I (2018) pulp regeneration concepts for nonvital teeth: from tissue engineering to clinical approaches. Tissue Eng Part B Rev 24(6):419–442. https://doi.org/10.1089/ten.TEB.2018.0073
Adnan S, Ullah R (2018) Top-cited articles in regenerative endodontics: a bibliometric analysis. J Endod 44(11):1650–1664. https://doi.org/10.1016/j.joen.2018.07.015
Morotomi T, Washio A, Kitamura C (2019) Current and future options for dental pulp therapy. Jpn Dent Sci Rev 55(1):5–11. https://doi.org/10.1016/j.jdsr.2018.09.001
Organization WH (2017) Oral health. https://www.who.int/publications/i/item/WHO-NMH-NHD-17.12. Accessed 19 November 2020
Organization WH (2003) Dental diseases and oral health. https://www.who.int/oral_health/publications/en/orh_fact_sheet.pdf. Accessed 19 November 2020
Li X, Kolltveit KM, Tronstad L, Olsen I (2000) Systemic diseases caused by oral infection. Clin Microbiol Rev 13(4):547–558. https://doi.org/10.1128/cmr.13.4.547-558.2000
Albuquerque MT, Valera MC, Nakashima M, Nor JE, Bottino MC (2014) Tissue-engineering-based strategies for regenerative endodontics. J Dent Res 93(12):1222–1231. https://doi.org/10.1177/0022034514549809
Itoh Y, Sasaki JI, Hashimoto M, Katata C, Hayashi M, Imazato S (2018) Pulp regeneration by 3-dimensional dental pulp stem cell constructs. J Dent Res 97(10):1137–1143. https://doi.org/10.1177/0022034518772260
Bottino MC, Pankajakshan D, Nor JE (2017) Advanced scaffolds for dental pulp and periodontal regeneration. Dent Clin North Am 61(4):689–711. https://doi.org/10.1016/j.cden.2017.06.009
Yildirim S, Fu SY, Kim K, Zhou H, Lee CH, Li A, Kim SG, Wang S, Mao JJ (2011) Tooth regeneration: a revolution in stomatology and evolution in regenerative medicine. Int J Oral Sci 3(3):107–116. https://doi.org/10.4248/IJOS11042
Bansal R, Jain A (2015) Current overview on dental stem cells applications in regenerative dentistry. J Nat Sci Biol Med 6(1):29–34. https://doi.org/10.4103/0976-9668.149074
Fischer NG, Munchow EA, Tamerler C, Bottino MC, Aparicio C (2020) Harnessing biomolecules for bioinspired dental biomaterials. J Mater Chem B 8(38):8713–8747. https://doi.org/10.1039/d0tb01456g
Bjorndal L, Simon S, Tomson PL, Duncan HF (2019) Management of deep caries and the exposed pulp. Int Endod J 52(7):949–973. https://doi.org/10.1111/iej.13128
de Souza Costa CA, Hebling J, Scheffel DL, Soares DG, Basso FG, Ribeiro AP (2014) Methods to evaluate and strategies to improve the biocompatibility of dental materials and operative techniques. Dent Mater 30(7):769–784. https://doi.org/10.1016/j.dental.2014.04.010
Hanna SN, Perez Alfayate R, Prichard J (2020) Vital pulp therapy an insight over the available literature and future expectations. Eur Endod J 5(1):46–53. https://doi.org/10.14744/eej.2019.44154
Medina-Fernandez I, Celiz AD (2019) Acellular biomaterial strategies for endodontic regeneration. Biomater Sci 7(2):506–519. https://doi.org/10.1039/c8bm01296b
Ricucci D, Loghin S, Lin LM, Spangberg LS, Tay FR (2014) Is hard tissue formation in the dental pulp after the death of the primary odontoblasts a regenerative or a reparative process? J Dent 42(9):1156–1170. https://doi.org/10.1016/j.jdent.2014.06.012
Altaii M, Richards L, Rossi-Fedele G (2017) Histological assessment of regenerative endodontic treatment in animal studies with different scaffolds: a systematic review. Dent Traumatol 33(4):235–244. https://doi.org/10.1111/edt.12338
Nosrat A, Kolahdouzan A, Khatibi AH, Verma P, Jamshidi D, Nevins AJ, Torabinejad M (2019) Clinical, radiographic, and histologic outcome of regenerative endodontic treatment in human teeth using a novel collagen-hydroxyapatite scaffold. J Endod 45(2):136–143. https://doi.org/10.1016/j.joen.2018.10.012
Yoo C, Vines JB, Alexander G, Murdock K, Hwang P, Jun HW (2014) Adult stem cells and tissue engineering strategies for salivary gland regeneration: a review. Biomater Res 18:9. https://doi.org/10.1186/2055-7124-18-9
Saoud TM, Zaazou A, Nabil A, Moussa S, Aly HM, Okazaki K, Rosenberg PA, Lin LM (2015) Histological observations of pulpal replacement tissue in immature dog teeth after revascularization of infected pulps. Dent Traumatol 31(3):243–249. https://doi.org/10.1111/edt.12169
Huang GT, Garcia-Godoy F (2014) Missing concepts in de novo pulp regeneration. J Dent Res 93(8):717–724. https://doi.org/10.1177/0022034514537829
Langer R, Vacanti JP (1993) Tissue engineering. Science 260(5110):920–926. https://doi.org/10.1126/science.8493529
Ma PX (2008) Biomimetic materials for tissue engineering. Adv Drug Deliv Rev 60(2):184–198. https://doi.org/10.1016/j.addr.2007.08.041
Swanson WB, Ma PX (2020) 1.4.7 - Textured and porous biomaterials. In: Wagner WR, Sakiyama-Elbert SE, Zhang G, Yaszemski MJ (eds) Biomaterials Science (Fourth Edition). Academic Press, pp 601-622. https://doi.org/https://doi.org/10.1016/B978-0-12-816137-1.00039-8
Gupte MJ, Swanson WB, Hu J, Jin X, Ma H, Zhang Z, Liu Z, Feng K, Feng G, Xiao G, Hatch N, Mishina Y, Ma PX (2018) Pore size directs bone marrow stromal cell fate and tissue regeneration in nanofibrous macroporous scaffolds by mediating vascularization. Acta Biomater 82:1–11. https://doi.org/10.1016/j.actbio.2018.10.016
Mousa M, Evans ND, Oreffo ROC, Dawson JI (2018) Clay nanoparticles for regenerative medicine and biomaterial design: A review of clay bioactivity. Biomaterials 159:204–214. https://doi.org/10.1016/j.biomaterials.2017.12.024
Galler KM, Widbiller M (2017) Perspectives for cell-homing approaches to engineer dental pulp. J Endod 43(9S):S40–S45. https://doi.org/10.1016/j.joen.2017.06.008
Yelick PC, Sharpe PT (2019) Tooth bioengineering and regenerative dentistry. J Dent Res 98(11):1173–1182. https://doi.org/10.1177/0022034519861903
Soares DG, Rosseto HL, Scheffel DS, Basso FG, Huck C, Hebling J, de Souza Costa CA (2017) Odontogenic differentiation potential of human dental pulp cells cultured on a calcium-aluminate enriched chitosan-collagen scaffold. Clin Oral Investig 21(9):2827–2839. https://doi.org/10.1007/s00784-017-2085-3
Soares DG, Anovazzi G, Bordini EAF, Zuta UO, Silva Leite MLA, Basso FG, Hebling J, de Souza Costa CA (2018) Biological analysis of simvastatin-releasing chitosan scaffold as a cell free system for pulp dentin regeneration. J Endod 44(6):971-976-e971. https://doi.org/10.1016/j.joen.2018.02.014
Soares DG, Zhang Z, Mohamed F, Eyster TW, de Souza Costa CA, Ma PX (2018) Simvastatin and nanofibrous poly(l-lactic acid) scaffolds to promote the odontogenic potential of dental pulp cells in an inflammatory environment. Acta Biomater 68:190–203. https://doi.org/10.1016/j.actbio.2017.12.037
Soares DG, Bordini EAF, Cassiano FB, Bronze-Uhle ES, Pacheco LE, Zabeo G, Hebling J, Lisboa-Filho PN, Bottino MC, de Souza Costa CA (2020) Characterization of novel calcium hydroxide-mediated highly porous chitosan-calcium scaffolds for potential application in dentin tissue engineering. J Biomed Mater Res B Appl Biomater 108(6):2546–2559. https://doi.org/10.1002/jbm.b.34586
Sakai VT, Cordeiro MM, Dong Z, Zhang Z, Zeitlin BD, Nor JE (2011) Tooth slice/scaffold model of dental pulp tissue engineering. Adv Dent Res 23(3):325–332. https://doi.org/10.1177/0022034511405325
da Fonseca Roberti Garcia L, Pontes EC, Basso FG, Hebling J, de Souza Costa CA, Soares DG, (2016) Transdentinal cytotoxicity of resin-based luting cements to pulp cells. Clin Oral Investig 20(7):1559–1566. https://doi.org/10.1007/s00784-015-1630-1
Leite M, Costa CAS, Duarte RM, Andrade AKM, Soares DG (2018) Bond strength and cytotoxicity of a universal adhesive according to the hybridization strategies to dentin. Braz Dent J 29(1):68–75. https://doi.org/10.1590/0103-6440201801698
Leite ML, Soares DG, de Oliveira Duque CC, Bordini EAF, Anovazzi G, Basso FG, Spolidorio DMP, Hebling J, de Souza Costa CA (2019) Positive influence of simvastatin used as adjuvant agent for cavity lining. Clin Oral Investig 23(9):3457–3469. https://doi.org/10.1007/s00784-018-2757-7
Murray PE, Lumley PJ, Ross HF, Smith AJ (2000) Tooth slice organ culture for cytotoxicity assessment of dental materials. Biomaterials 21(16):1711–1721. https://doi.org/10.1016/s0142-9612(00)00056-9
Laurent P, Camps J, About I (2012) Biodentine(TM) induces TGF-beta1 release from human pulp cells and early dental pulp mineralization. Int Endod J 45(5):439–448. https://doi.org/10.1111/j.1365-2591.2011.01995.x
Pedano MS, Li X, Jeanneau C, Ghosh M, Yoshihara K, Van Landuyt K, About I, Van Meerbeek B (2019) Survival of human dental pulp cells after 4-week culture in human tooth model. J Dent 86:33–40. https://doi.org/10.1016/j.jdent.2019.05.023
Li J, Rao Z, Zhao Y, Xu Y, Chen L, Shen Z, Bai Y, Lin Z, Huang Q (2020) A decellularized matrix hydrogel derived from human dental pulp promotes dental pulp stem cell proliferation, migration, and induced multidirectional differentiation in vitro. J Endod 46(10):1438-1447.e1435. https://doi.org/10.1016/j.joen.2020.07.008
Tecles O, Laurent P, Aubut V, About I (2008) Human tooth culture: a study model for reparative dentinogenesis and direct pulp capping materials biocompatibility. J Biomed Mater Res B Appl Biomater 85(1):180–187. https://doi.org/10.1002/jbm.b.30933
Li X, Pedano MS, Camargo B, Hauben E, De Vleeschauwer S, Chen Z, De Munck J, Vandamme K, Van Landuyt K, Van Meerbeek B (2018) Experimental tricalcium silicate cement induces reparative dentinogenesis. Dent Mater 34(9):1410–1423. https://doi.org/10.1016/j.dental.2018.06.016
Swanson WB, Gong T, Zhang Z, Eberle M, Niemann D, Dong R, Rambhia KJ, Ma PX (2020) Controlled release of odontogenic exosomes from a biodegradable vehicle mediates dentinogenesis as a novel biomimetic pulp capping therapy. J Control Release 324:679–694. https://doi.org/10.1016/j.jconrel.2020.06.006
Huang GT, Yamaza T, Shea LD, Djouad F, Kuhn NZ, Tuan RS, Shi S (2010) Stem/progenitor cell-mediated de novo regeneration of dental pulp with newly deposited continuous layer of dentin in an in vivo model. Tissue Eng Part A 16(2):605–615. https://doi.org/10.1089/ten.TEA.2009.0518
Iohara K, Imabayashi K, Ishizaka R, Watanabe A, Nabekura J, Ito M, Matsushita K, Nakamura H, Nakashima M (2011) Complete pulp regeneration after pulpectomy by transplantation of CD105+ stem cells with stromal cell-derived factor-1. Tissue Eng Part A 17(15–16):1911–1920. https://doi.org/10.1089/ten.TEA.2010.0615
Rosa V, Zhang Z, Grande RH, Nor JE (2013) Dental pulp tissue engineering in full-length human root canals. J Dent Res 92(11):970–975. https://doi.org/10.1177/0022034513505772
Nakashima M, Iohara K, Bottino MC, Fouad AF, Nor JE, Huang GT (2019) Animal models for stem cell-based pulp regeneration: foundation for human clinical applications. Tissue Eng Part B Rev 25(2):100–113. https://doi.org/10.1089/ten.TEB.2018.0194
Cordeiro MM, Dong Z, Kaneko T, Zhang Z, Miyazawa M, Shi S, Smith AJ, Nor JE (2008) Dental pulp tissue engineering with stem cells from exfoliated deciduous teeth. J Endod 34(8):962–969. https://doi.org/10.1016/j.joen.2008.04.009
Galler KM, Hartgerink JD, Cavender AC, Schmalz G, D’Souza RN (2012) A customized self-assembling peptide hydrogel for dental pulp tissue engineering. Tissue Eng Part A 18(1–2):176–184. https://doi.org/10.1089/ten.TEA.2011.0222
Dissanayaka WL, Hargreaves KM, Jin L, Samaranayake LP, Zhang C (2015) The interplay of dental pulp stem cells and endothelial cells in an injectable peptide hydrogel on angiogenesis and pulp regeneration in vivo. Tissue Eng Part A 21(3–4):550–563. https://doi.org/10.1089/ten.TEA.2014.0154
Silva CR, Babo PS, Gulino M, Costa L, Oliveira JM, Silva-Correia J, Domingues RMA, Reis RL, Gomes ME (2018) Injectable and tunable hyaluronic acid hydrogels releasing chemotactic and angiogenic growth factors for endodontic regeneration. Acta Biomater 77:155–171. https://doi.org/10.1016/j.actbio.2018.07.035
Mu X, Shi L, Pan S, He L, Niu Y, Wang X (2020) A customized self-assembling peptide hydrogel-wrapped stem cell factor targeting pulp regeneration rich in vascular-like structures. ACS Omega 5(27):16568–16574. https://doi.org/10.1021/acsomega.0c01266
Xiao S, Zhao T, Wang J, Wang C, Du J, Ying L, Lin J, Zhang C, Hu W, Wang L, Xu K (2019) Gelatin methacrylate (GelMA)-based hydrogels for cell transplantation: an effective strategy for tissue engineering. Stem Cell Rev Rep 15(5):664–679. https://doi.org/10.1007/s12015-019-09893-4
Monteiro N, Thrivikraman G, Athirasala A, Tahayeri A, França CM, Ferracane JL, Bertassoni LE (2018) Photopolymerization of cell-laden gelatin methacryloyl hydrogels using a dental curing light for regenerative dentistry. Dent Mater 34(3):389–399. https://doi.org/10.1016/j.dental.2017.11.020
Khayat A, Monteiro N, Smith EE, Pagni S, Zhang W, Khademhosseini A, Yelick PC (2017) GelMA-encapsulated hDPSCs and HUVECs for dental pulp regeneration. J Dent Res 96(2):192–199. https://doi.org/10.1177/0022034516682005
Athirasala A, Lins F, Tahayeri A, Hinds M, Smith AJ, Sedgley C, Ferracane J, Bertassoni LE (2017) A novel strategy to engineer pre-vascularized full-length dental pulp-like tissue constructs. Sci Rep 7(1):3323. https://doi.org/10.1038/s41598-017-02532-3
Zhang R, Xie L, Wu H, Yang T, Zhang Q, Tian Y, Liu Y, Han X, Guo W, He M, Liu S, Tian W (2020) Alginate/laponite hydrogel microspheres co-encapsulating dental pulp stem cells and VEGF for endodontic regeneration. Acta Biomater 113:305–316. https://doi.org/10.1016/j.actbio.2020.07.012
Zhang Z, Marson RL, Ge Z, Glotzer SC, Ma PX (2015) Simultaneous nano- and microscale control of nanofibrous microspheres self-assembled from star-shaped polymers. Adv Mater 27(26):3947–3952. https://doi.org/10.1002/adma.201501329
Li X, Ma C, Xie X, Sun H, Liu X (2016) Pulp regeneration in a full-length human tooth root using a hierarchical nanofibrous microsphere system. Acta Biomater 35:57–67. https://doi.org/10.1016/j.actbio.2016.02.040
Ma PX, Zhang R (1999) Synthetic nano-scale fibrous extracellular matrix. J Biomed Mater Res 46(1):60–72. https://doi.org/10.1002/(sici)1097-4636(199907)46:1%3c60::aid-jbm7%3e3.0.co;2-h
Wang X, Song G, Lou T (2010) Fabrication and characterization of nano composite scaffold of poly(L-lactic acid)/hydroxyapatite. J Mater Sci Mater Med 21(1):183–188. https://doi.org/10.1007/s10856-009-3855-5
Kuang R, Zhang Z, Jin X, Hu J, Gupte MJ, Ni L, Ma PX (2015) Nanofibrous spongy microspheres enhance odontogenic differentiation of human dental pulp stem cells. Adv Healthc Mater 4(13):1993–2000. https://doi.org/10.1002/adhm.201500308
Wang W, Dang M, Zhang Z, Hu J, Eyster TW, Ni L, Ma PX (2016) Dentin regeneration by stem cells of apical papilla on injectable nanofibrous microspheres and stimulated by controlled BMP-2 release. Acta Biomater 36:63–72. https://doi.org/10.1016/j.actbio.2016.03.015
Kuang R, Zhang Z, Jin X, Hu J, Shi S, Ni L, Ma PX (2016) Nanofibrous spongy microspheres for the delivery of hypoxia-primed human dental pulp stem cells to regenerate vascularized dental pulp. Acta Biomater 33:225–234. https://doi.org/10.1016/j.actbio.2016.01.032
Sabrah AH, Yassen GH, Liu WC, Goebel WS, Gregory RL, Platt JA (2015) The effect of diluted triple and double antibiotic pastes on dental pulp stem cells and established Enterococcus faecalis biofilm. Clin Oral Investig 19(8):2059–2066. https://doi.org/10.1007/s00784-015-1423-6
Sotomil JM, Munchow EA, Pankajakshan D, Spolnik KJ, Ferreira JA, Gregory RL, Bottino MC (2019) Curcumin-a natural medicament for root canal disinfection: effects of irrigation, drug release, and photoactivation. J Endod 45(11):1371–1377. https://doi.org/10.1016/j.joen.2019.08.004
Kamocki K, Nor JE, Bottino MC (2015) Dental pulp stem cell responses to novel antibiotic-containing scaffolds for regenerative endodontics. Int Endod J 48(12):1147–1156. https://doi.org/10.1111/iej.12414
Albuquerque MT, Evans JD, Gregory RL, Valera MC, Bottino MC (2016) Antibacterial TAP-mimic electrospun polymer scaffold: effects on P. gingivalis-infected dentin biofilm. Clin Oral Investig 20:2387–393. https://doi.org/10.1007/s00784-015-1577-2
Pankajakshan D, Albuquerque MT, Evans JD, Kamocka MM, Gregory RL, Bottino MC (2016) Triple antibiotic polymer nanofibers for intracanal drug delivery: effects on dual species biofilm and cell function. J Endod 42(10):1490–1495. https://doi.org/10.1016/j.joen.2016.07.019
Karczewski A, Feitosa SA, Hamer EI, Pankajakshan D, Gregory RL, Spolnik KJ, Bottino MC (2018) Clindamycin-modified triple antibiotic nanofibers: a stain-free antimicrobial intracanal drug delivery system. J Endod 44(1):155–162. https://doi.org/10.1016/j.joen.2017.08.024
Bottino MC, Albuquerque MTP, Azabi A, Munchow EA, Spolnik KJ, Nor JE, Edwards PC (2019) A novel patient-specific three-dimensional drug delivery construct for regenerative endodontics. J Biomed Mater Res B Appl Biomater 107(5):1576–1586. https://doi.org/10.1002/jbm.b.34250
Ribeiro JS, Daghrery A, Dubey N, Li C, Mei L, Fenno JC, Schwendeman A, Aytac Z, Bottino MC (2020) Hybrid antimicrobial hydrogel as injectable therapeutics for oral infection ablation. Biomacromolecules 21(9):3945–3956. https://doi.org/10.1021/acs.biomac.0c01131
Ribeiro JS, Bordini EAF, Ferreira JA, Mei L, Dubey N, Fenno JC, Piva E, Lund RG, Schwendeman A, Bottino MC (2020) Injectable MMP-responsive nanotube-modified gelatin hydrogel for dental infection ablation. ACS Appl Mater Interfaces 12(14):16006–16017. https://doi.org/10.1021/acsami.9b22964
Wang YY, Chatzistavrou X, Faulk D, Badylak S, Zheng L, Papagerakis S, Ge L, Liu H, Papagerakis P (2015) Biological and bactericidal properties of Ag-doped bioactive glass in a natural extracellular matrix hydrogel with potential application in dentistry. Eur Cell Mater 29:342-355. https://doi.org/10.22203/ecm.v029a26
Qu T, Jing J, Jiang Y, Taylor RJ, Feng JQ, Geiger B, Liu X (2014) Magnesium-containing nanostructured hybrid scaffolds for enhanced dentin regeneration. Tissue Eng Part A 20(17–18):2422–2433. https://doi.org/10.1089/ten.TEA.2013.0741
Okamoto M, Matsumoto S, Sugiyama A, Kanie K, Watanabe M, Huang H, Ali M, Ito Y, Miura J, Hirose Y, Uto K, Ebara M, Kato R, Yamawaki-Ogata A, Narita Y, Kawabata S, Takahashi Y, Hayashi M (2020) Performance of a biodegradable composite with hydroxyapatite as a scaffold in pulp tissue repair. Polymers (Basel) 12 (4). https://doi.org/10.3390/polym12040937
Soares DG, Rosseto HL, Basso FG, Scheffel DS, Hebling J, Costa CA (2016) Chitosan-collagen biomembrane embedded with calcium-aluminate enhances dentinogenic potential of pulp cells. Braz Oral Res 30(1):e54. https://doi.org/10.1590/1807-3107BOR-2016.vol30.0054
Bordini EAF, Cassiano FB, Silva ISP, Usberti FR, Anovazzi G, Pacheco LE, Pansani TN, Leite ML, Hebling J, de Souza Costa CA, Soares DG (2017) Synergistic potential of 1alpha,25-dihydroxyvitamin D3 and calcium-aluminate-chitosan scaffolds with dental pulp cells. Clin Oral Investig 24(2):663–674. https://doi.org/10.1007/s00784-019-02906-z
Cassiano FB, Soares DG, Bordini EAF, Anovazzi G, Hebling J, Costa CAS (2020) Simvastatin-enriched macro-porous chitosan-calcium-aluminate scaffold for mineralized tissue regeneration. Braz Dent J 31(4):385–391. https://doi.org/10.1590/0103-6440202003252
Dubey N, Ferreira JA, Malda J, Bhaduri SB, Bottino MC (2020) Extracellular matrix/amorphous magnesium phosphate bioink for 3D Bioprinting of craniomaxillofacial bone tissue. ACS Appl Mater Interfaces 12(21):23752–23763. https://doi.org/10.1021/acsami.0c05311
Li F, Liu X, Zhao S, Wu H, Xu HH (2014) Porous chitosan bilayer membrane containing TGF-beta1 loaded microspheres for pulp capping and reparative dentin formation in a dog model. Dent Mater 30(2):172–181. https://doi.org/10.1016/j.dental.2013.11.005
Daghrery A, Aytac Z, Dubey N, Mei L, Schwendeman A, Bottino MC (2020) Electrospinning of dexamethasone/cyclodextrin inclusion complex polymer fibers for dental pulp therapy. Colloids Surf B Biointerfaces 191:111011. https://doi.org/10.1016/j.colsurfb.2020.111011
Niu X, Liu Z, Hu J, Rambhia KJ, Fan Y, Ma PX (2016) Microspheres assembled from chitosan-graft-poly(lactic acid) micelle-like core-shell nanospheres for distinctly controlled release of hydrophobic and hydrophilic biomolecules. Macromol Biosci 16(7):1039–1047. https://doi.org/10.1002/mabi.201600020
Ha M, Athirasala A, Tahayeri A, Menezes PP, Bertassoni LE (2020) Micropatterned hydrogels and cell alignment enhance the odontogenic potential of stem cells from apical papilla in-vitro. Dent Mater 36(1):88–96. https://doi.org/10.1016/j.dental.2019.10.013
Pankajakshan D, Voytik-Harbin SL, Nor JE, Bottino MC (2020) Injectable highly tunable oligomeric collagen matrices for dental tissue regeneration. ACS Appl Bio Mater 3(2):859–868. https://doi.org/10.1021/acsabm.9b00944
Dubey N, Ferreira JA, Daghrery A, Aytac Z, Malda J, Bhaduri SB, Bottino MC (2020) Highly tunable bioactive fiber-reinforced hydrogel for guided bone regeneration. Acta Biomater 113:164–176. https://doi.org/10.1016/j.actbio.2020.06.011
Cooper LF, Ravindran S, Huang CC, Kang M (2019) A role for exosomes in craniofacial tissue engineering and regeneration. Front Physiol 10:1569. https://doi.org/10.3389/fphys.2019.01569
Huang CC, Narayanan R, Alapati S, Ravindran S (2016) Exosomes as biomimetic tools for stem cell differentiation: applications in dental pulp tissue regeneration. Biomaterials 111:103–115. https://doi.org/10.1016/j.biomaterials.2016.09.029
Xian X, Gong Q, Li C, Guo B, Jiang H (2018) Exosomes with highly angiogenic potential for possible use in pulp regeneration. J Endod 44(5):751–758. https://doi.org/10.1016/j.joen.2017.12.024
Zhang S, Yang Y, Jia S, Chen H, Duan Y, Li X, Wang S, Wang T, Lyu Y, Chen G, Tian W (2020) Exosome-like vesicles derived from Hertwig’s epithelial root sheath cells promote the regeneration of dentin-pulp tissue. Theranostics 10(13):5914–5931. https://doi.org/10.7150/thno.43156
Chen J, Cui C, Qiao X, Yang B, Yu M, Guo W, Tian W (2017) Treated dentin matrix paste as a novel pulp capping agent for dentin regeneration. J Tissue Eng Regen Med 11(12):3428–3436. https://doi.org/10.1002/term.2256
Holiel AA, Mahmoud EM, Abdel-Fattah WM, Kawana KY (2020) Histological evaluation of the regenerative potential of a novel treated dentin matrix hydrogel in direct pulp capping. Clin Oral Investig. https://doi.org/10.1007/s00784-020-03521-z
Salehi S, Cooper P, Smith A, Ferracane J (2016) Dentin matrix components extracted with phosphoric acid enhance cell proliferation and mineralization. Dent Mater 32(3):334–342. https://doi.org/10.1016/j.dental.2015.11.004
Zhang R, Cooper PR, Smith G, Nor JE, Smith AJ (2011) Angiogenic activity of dentin matrix components. J Endod 37(1):26–30. https://doi.org/10.1016/j.joen.2010.08.042
Smith JG, Smith AJ, Shelton RM, Cooper PR (2015) Dental pulp cell behavior in biomimetic environments. J Dent Res 94(11):1552–1559. https://doi.org/10.1177/0022034515599767
Galler KM, Widbiller M, Buchalla W, Eidt A, Hiller KA, Hoffer PC, Schmalz G (2016) EDTA conditioning of dentine promotes adhesion, migration and differentiation of dental pulp stem cells. Int Endod J 49(6):581–590. https://doi.org/10.1111/iej.12492
Widbiller M, Eidt A, Hiller KA, Buchalla W, Schmalz G, Galler KM (2017) Ultrasonic activation of irrigants increases growth factor release from human dentine. Clin Oral Investig 21(3):879–888. https://doi.org/10.1007/s00784-016-1824-1
Widbiller M, Driesen RB, Eidt A, Lambrichts I, Hiller KA, Buchalla W, Schmalz G, Galler KM (2018) Cell homing for pulp tissue engineering with endogenous dentin matrix proteins. J Endod 44(6):956-962-e952. https://doi.org/10.1016/j.joen.2018.02.011
Huang KH, Chen YW, Wang CY, Lin YH, Wu YA, Shie MY, Lin CP (2018) Enhanced capability of bone morphogenetic protein 2-loaded mesoporous calcium silicate scaffolds to induce odontogenic differentiation of human dental pulp cells. J Endod 44(11):1677–1685. https://doi.org/10.1016/j.joen.2018.08.008
Athirasala A, Tahayeri A, Thrivikraman G, Franca CM, Monteiro N, Tran V, Ferracane J, Bertassoni LE (2018) A dentin-derived hydrogel bioink for 3D bioprinting of cell laden scaffolds for regenerative dentistry. Biofabrication 10(2):024101. https://doi.org/10.1088/1758-5090/aa9b4e
Yang JW, Shen YC, Lin KC, Cheng SJ, Chen SL, Chen CY, Kumar PV, Lin SF, Lu HE, Chen GY (2020) Organ-on-a-chip: opportunities for assessing the toxicity of particulate matter. front bioeng biotechnol 8:519. https://doi.org/10.3389/fbioe.2020.00519
França CM, Tahayeri A, Rodrigues NS, Ferdosian S, Puppin Rontani RM, Sereda G, Ferracane JL, Bertassoni LE (2020) The tooth on-a-chip: a microphysiologic model system mimicking the biologic interface of the tooth with biomaterials. Lab Chip 20(2):405–413. https://doi.org/10.1039/c9lc00915a
Duarte Campos DF, Zhang S, Kreimendahl F, Kopf M, Fischer H, Vogt M, Blaeser A, Apel C, Esteves-Oliveira M (2020) Hand-held bioprinting for de novo vascular formation applicable to dental pulp regeneration. Connect Tissue Res 61(2):205–215. https://doi.org/10.1080/03008207.2019.1640217
Funding
The work was supported by the National Institutes of Health/National Institute for Dental and Craniofacial Research (NIH/NIDCR, grants F30-DE029359 to WBS and R01DE026578 to MCB), the São Paulo Research Foundation – FAPESP (grant 2016/15674-5), and by the Coordination for the Improvement of Higher Education Personnel – CAPES (Finance Code 001). The content of this review is solely the responsibility of the authors and does not necessarily represent the official view of the funding sources. We apologize to colleagues whose work we could not discuss due to space limitations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Soares, D.G., Bordini, E.A.F., Swanson, W.B. et al. Platform technologies for regenerative endodontics from multifunctional biomaterials to tooth-on-a-chip strategies. Clin Oral Invest 25, 4749–4779 (2021). https://doi.org/10.1007/s00784-021-04013-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-04013-4