Abstract
Objective
To assess augmentation success after guided bone regeneration (GBR) carried out simultaneously with implant placement using bovine-derived xenograft alone and in combination with liquid platelet-rich fibrin (liquid-PRF).
Methods
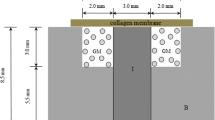
This randomized controlled clinical trial was conducted on patients with horizontal bone deficiency in the posterior regions of the mandible. After implant placement, GBR procedures were randomly performed using liquid-PRF-enriched bovine-derived xenograft (for the test group) and with bovine-derived xenograft alone (for the control group). To assess the change in augmentation thickness, the primary outcome of the study, cone beam computed tomography was carried out at the implant sites on completion and 6 months after surgery. The secondary outcomes were marginal bone level and implant survival rate at prosthetic delivery and at 6 months, 1 year, and 2 years follow-up after loading. The significance level was set at p<0.05 for all analysis.
Results
Twenty patients with 50 implants were analyzed for the test group and 20 patients with 48 implants for the control group. At 6 months postoperatively, the mean values of augmentation thickness were 1.63 ± 0.21 mm, 2.59 ± 0.34 mm, and 3.11 ± 0.36 mm for the test group and 1.34 ± 0.14 mm, 2.49 ± 0.24 mm, and 2.97 ± 0.24 mm for the control group at 2 mm, 4 mm, and 6 mm below to the implant shoulder (p < 0.001, p = 0.007, and p = 0.036, respectively). The mean marginal bone loss was found to be less than 1 mm for both study groups during the 2 years of follow-up after prosthetic loading. Implant survival rate was 100% for both study groups.
Conclusion
Bovine-derived xenograft alone and in combination with liquid-PRF are both successful in achieving bone augmentation around the implants and produce a small change in marginal bone level and a high implant survival rate after loading.
Clinical relevance
There is a lack of evidence in the literature regarding the augmentation success of liquid-PRF used in combination with bone graft substitutes. This study indicates that liquid-PRF could be used as a supportive material with bovine-derived xenograft in GBR procedures carried out simultaneously with implant placement.








Similar content being viewed by others
References
Wessing B, Urban I, Montero E, Zechner W, Hof M, Alandez Chamorro J, Alandez Martin N, Polizzi G, Meloni S, Sanz M (2017) A multicenter randomized controlled clinical trial using a new resorbable non-cross-linked collagen membrane for guided bone regeneration at dehisced single implant sites: interim results of a bone augmentation procedure. Clin Oral Implants Res 28:e218–e226. https://doi.org/10.1111/clr.12995
Khzam N, Arora H, Kim P, Fisher A, Mattheos N, Ivanovski S (2015) Systematic review of soft tissue alterations and aesthetic outcomes following immediate implant placement and restoration of single implants in the anterior maxilla. J Periodontol 86:1321–1330. https://doi.org/10.1902/jop.2015.150287
Araújo MG, Lindhe J (2005) Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol 32:21–218. https://doi.org/10.1111/j.1600-051X.2005.00642.x
Cardaropoli G, Araújo M, Lindhe J (2003) Dynamics of bone tissue formation in tooth extraction sites. An experimental study in dogs. J Clin Periodontol 30:809–818. https://doi.org/10.1034/j.1600-051x.2003.00366.x
Rocchietta I, Fontana F, Simion M (2008) Clinical outcomes of vertical bone augmentation to enable dental implant placement: a systematic review. J Clin Periodontol 35:203–215. https://doi.org/10.1111/j.1600-051X.2008.01271.x
Checchi V, Gasparro R, Pistilli R, Canullo L, Felice P (2019) Clinical classification of bone augmentation procedure failures in the atrophic anterior maxillae: esthetic consequences and treatment options. BioMed Res Int 3:1–16. https://doi.org/10.1155/2019/4386709
Cucchi A, Vignudelli E, Napolitano A, Corinaldesi G (2017) Evaluation of complication rates and vertical bone gain after guided bone regeneration with non-resorbable membranes versus titanium meshes and resorbable membranes. A randomized clinical trial. Clin Implant Dent Relat Res 19:821–832. https://doi.org/10.1111/cid.12520
Fontana F, Maschera E, Rocchietta I, Simion M (2011) Clinical classification of complications in guided bone regeneration procedures by means of a nonresorbable membrane. Int J Periodontics Restorative Dent 31:265–273
Clementini M, Morlupi A, Canullo L, Agrestini C, Barlattani A (2012) Success rate of dental implants inserted in horizontal and vertical guided bone regenerated areas: a systematic review. Int J Oral Maxillofac Surg 41:847–852. https://doi.org/10.1016/j.ijom.2012.03.016
Chiapasco M, Zaniboni M (2009) Clinical outcomes of GBR procedures to correct peri-implant dehiscences and fenestrations: a systematic review. Clin Oral Implants Res 20:113–123. https://doi.org/10.1111/j.1600-0501.2009.01781.x
Hämmerle CH, Jung RE, Feloutzis A (2002) A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. J Clin Periodontol 29:226–231. https://doi.org/10.1034/j.1600-051x.29.s3.14.x
Arunjaroensuk S, Panmekiate S, Pimkhaokham A (2018) The stability of augmented bone between two different membranes used for guided bone regeneration simultaneous with dental implant placement in the esthetic zone. Int J Oral Maxillofac Implants 33:206–216. https://doi.org/10.11607/jomi.5492
Jung RE, Herzog M, Wolleb K, Ramel CF, Thoma DS, Hammerle CHF (2017) A randomized controlled clinical trial comparing small buccal dehiscence defects around dental implants treated with guided bone regeneration or left for spontaneous healing. Clin Oral Implants Res 28:348–354. https://doi.org/10.1111/clr.12806
ArRejaie A, Al-Harbi F, Alagl A, Hassan K (2016) Platelet-rich plasma gel combined with bovine-derived xenograft for the treatment of dehiscence around immediately placed conventionally loaded dental implants in humans: cone beam computed tomography and three-dimensional image evaluation. Int J Oral Maxillofac Implants 31:431–438. https://doi.org/10.11607/jomi.3859
Temmerman A, Cortellini S, Van Dessel J, De Greef A, Jacobs R, Dhondt R (2020) Bovine-derived xenograft in combination with autogenous bone chips versus xenograft alone for the augmentation of bony dehiscences around oral implants: a randomized, controlled, split-mouth clinical trial. J Clin Periodontol 47:110–119
Papageorgiou SN, Papageorgiou PN, Deschner J, Götz W (2016) Comparative effectiveness of natural and synthetic bone grafts in oral and maxillofacial surgery prior to insertion of dental implants: systematic review and network meta-analysis of parallel and cluster randomized controlled trials. J Dent 48:1–8. https://doi.org/10.1016/j.jdent.2016.03.010
Troeltzsch M, Troeltzsch M, Kauffmann P, Gruber R, Brockmeyer P, Moser N, Rau A, Schliephake H (2016) Clinical efficacy of grafting materials in alveolar ridge augmentation: a systematic review. J Craniomaxillofac Surg 44:1618–1629. https://doi.org/10.1016/j.jcms.2016.07.028
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (prf): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e45–e50. https://doi.org/10.1016/j.tripleo.2005.07.009
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM (2006) Platelet-rich fibrin (prf): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e56–e60. https://doi.org/10.1016/j.tripleo.2005.07.011
Ghanaati S, Herrera-Vizcaino C, Al-Maawi S, Lorenz J, Miron RJ, Nelson K, Schwarz F, Choukroun J, Sader R (2018) Fifteen years of platelet rich fibrin (PRF) in dentistry and oromaxillofacial surgery: how high is the level of scientific evidence? J Oral Implantol 44:471–492. https://doi.org/10.1563/aaid-joi-D-17-00179
Strauss FJ, Nasirzade J, Kargarpoor Z, Stähli A, Gruber R (2020) Effect of platelet-rich fibrin on cell proliferation, migration, differentiation, inflammation, and osteoclastogenesis: a systematic review of in vitro studies. Clin Oral Investig 24:569–584. https://doi.org/10.1007/s00784-019-03156-9
Choukroun J, Ghanaati S (2018) Reduction of relative centrifugation force within PRF (platelet-rich-fibrin) concentrates advances patients’ own inflammatory cells and platelets: first introduction of the low speed centrifugation concept. Eur J Trauma Emerg Surg 44:87–95. https://doi.org/10.1007/s00068-017-0767-9
El-Baghdadi K, Kubesch A, Yu X, Al-Maawi S, Orlowska A, Dias A, Booms P, Dohle E, Sader R, Kirkpatrick J, Choukroun J, Ghanaati S (2019) Reduction of relative centrifugal forces increases growth factor release within solid platelet-rich-fibrin (PRF)-based matrices: a proof of concept of LSCC (low speed centrifugation concept). Eur J Trauma Emerg Surg 45:467–479. https://doi.org/10.1007/s00068-017-0785-7
Miron RJ, Fujioka-Kobayashi M, Hernandez M, Kandalam U, Zhang Y, Ghanaati S, Choukroun J (2017) Injectable platelet rich fibrin (i-prf): opportunities in regenerative dentistry? Clin Oral Investig 21:2619–2627. https://doi.org/10.1007/s00784-017-2063-9
Gülşen U, Dereci Ö (2019) Evaluation of new bone formation in sinus floor augmentation with injectable platelet-rich fibrin-soaked collagen plug: a pilot study. Implant Dent 28:220–225. https://doi.org/10.1097/ID.0000000000000883
Thanasrisuebwong P, Surarit R, Bencharit S, Ruangsawasdi N (2019) Influence of fractionation methods on physical and biological properties of injectable platelet-rich fibrin: an exploratory study. Int J Mol Sci 20:1657. https://doi.org/10.3390/ijms20071657
Valladão CAA, Monteiro MF, Joly JC (2020) Guided bone regeneration in staged vertical and horizontal bone augmentation using platelet-rich fibrin associated with bone grafts: a retrospective clinical study. Int J Implant Dent 6:72. https://doi.org/10.1186/s40729-020-00266-y
Juodzbalys G, Raustia AM (2004) Accuracy of clinical and radiological classification of the jawbone anatomy for implantation--a survey of 374 patients. J Oral Implantol 30:30–39. https://doi.org/10.1563/1548-1336(2004)030<0030:AOCARC>2.0.CO;2
Chen LC, Lundgren T, Hallström H, Cherel F (2008) Comparison of different methods of assessing alveolar ridge dimensions prior to dental implant placement. J Periodontol 79:401–405. https://doi.org/10.1902/jop.2008.070021
Urban IA, Monje A, Lozada J, Wang HL (2017) Principles for vertical ridge augmentation in the atrophic posterior mandible: a technical review. Int J Periodontics Restorative Dent 37:639–645. https://doi.org/10.11607/prd.3200
Choukroun J (2014) Advanced PRF, &i-PRF : platelet concentrates or blood concentrates? J Periodont Med Clin Pract 1:3
Miron RJ, Pinto NR, Quirynen M, Ghanaati S (2019) Standardization of relative centrifugal forces in studies related to platelet-rich fibrin. J Periodontol 90:817–820. https://doi.org/10.1002/JPER.18-0553
Miron R, Choukroun J, Ghanaati S (2018) Controversies related to scientific report describing g-forces from studies on platelet-rich fibrin: necessity for standardization of relative centrifugal force values. Int J Growth Factors Stem Cells Dent 1:80–89. https://doi.org/10.4103/GFSC.GFSC_23_18
Danesh-Sani SA, Tarnow D, Yip JK, Mojaver R (2017) The influence of cortical bone perforation on guided bone regeneration in humans. Int J Oral Maxillofac Surg 46:261–266. https://doi.org/10.1016/j.ijom.2016.10.017
Meloni SM, Jovanovic SA, Pisano M, De Riu G, Baldoni E, Tallarico M (2018) One-stage horizontal guided bone regeneration with autologous bone, anorganic bovine bone and collagen membranes: follow-up of a prospective study 30 months after loading. Eur J Oral Implantol 11:89–95. https://doi.org/10.1111/jcpe.13209
Basler T, Naenni N, Schneider D, Hämmerle CHF, Jung RE, Thoma DS (2018) Randomized controlled clinical study assessing two membranes for guided bone regeneration of peri-implant bone defects: 3-year results. Clin Oral Implants Res 29:499–507. https://doi.org/10.1111/clr.13147
Albrekttson T, Zarb G, Worthington P, Eriksson AR (1986) The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants 1:11–25
Hämmerle CH, Jung RE, Yaman D, Lang NP (2008) Ridge augmentation by applying bioresorbable membranes and deproteinized bovine bone mineral: a report of twelve consecutive cases. Clin Oral Implants Res 19:19–25. https://doi.org/10.1111/j.1600-0501.2007.01407.x
Moses O, Pitaru S, Artzi Z, Nemcovsky CE (2005) Healing of dehiscence-type defects in implants placed together with different barrier membranes: a comparative clinical study. Clin Oral Implants Res 16:210–219. https://doi.org/10.1111/j.1600-0501.2004.01100.x
Juodzbalys G, Raustia AM, Kubilius R (2007) A 5-year follow-up study on one-stage implants inserted concomitantly with localized alveolar ridge augmentation. J Oral Rehabil 34:781–789. https://doi.org/10.1111/j.1365-2842.2006.01679.x
Mordini L, Hur Y, Ogata Y, Finkelman M, Cavani F, Steffensen B (2020) Volumetric changes following lateral guided bone regeneration. Int J Oral Maxillofac Implants 35:e77–e85. https://doi.org/10.11607/jomi.7524
Khojasteh A, Motamedian SR, Sharifzadeh N, Zadeh HH (2016) The influence of initial alveolar ridge defect morphology on the outcome of implants in augmented atrophic posterior mandible: an exploratory retrospective study. Clin Oral Implants Res 28:208–217. https://doi.org/10.1111/clr.12991
Wang X, Zhang Y, Choukroun J, Ghanaati S, Miron RJ (2017) Behavior of gingival fibroblasts on titanium implant surfaces in combination with either injectable-PRF or PRP. Int J Mol Sci 18:331. https://doi.org/10.3390/ijms18020331
Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V, Fujioka-Kobayashi M, Bishara M, Zhang Y, Wang HL, Chandad F, Nacopoulos C, Simonpieri A, Aalam AA, Felice P, Sammartino G, Ghanaati S, Hernandez MA, Choukroun J (2017) Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig 21:1913–1927. https://doi.org/10.1007/s00784-017-2133-z
Castro AB, Meschi N, Temmerman A, Pinto N, Lambrechts P, Teughels W, Quirynen M (2017) Regenerative potential of leucocyte- and platelet-rich fibrin. Part B: sinus floor elevation, alveolar ridge preservation and implant therapy. a systematic review. J Clin Periodontol 44:225–234. https://doi.org/10.1111/jcpe.12658
Eskan MA, Greenwell H, Hill M, Morton D, Vidal R, Shumway B, Girouard ME (2014) Platelet-rich plasma-assisted guided bone regeneration for ridge augmentation: a randomized, controlled clinical trial. J Periodontol 85:661–668. https://doi.org/10.1902/jop.2013.130260
Miron RJ, Dham A, Dham U, Zhang Y, Pikos MA, Sculean A (2019) The effect of age, gender, and time between blood draw and start of centrifugation on the size outcomes of platelet-rich fibrin (PRF) membranes. Clin Oral Investig 23:2179–2185. https://doi.org/10.1007/s00784-018-2673-x
Lourenço ES, Mourão CFAB, Leite PEC, Granjeiro JM, Calasans-Maia MD, Alves GG (2018) The in vitro release of cytokines and growth factors from fibrin membranes produced through horizontal centrifugation. J Biomed Mater Res A 106:1373–1380. https://doi.org/10.1002/jbm.a.36346
Miron RJ, Chai J, Sculean A, Zhang Y (2019) A novel method for evaluating and quantifying cell types in platelet rich fibrin and an introduction to horizontal centrifugation. J Biomed Mater Res A 107:2257–2271. https://doi.org/10.1002/jbm.a.36734
Fujioka-Kobayashi M, Kono M, Katagiri H, Schaller B, Zhang Y, Schulean A, Miron RJ (2021) Histological comparison of platelet rich fibrin clots prepared by fixed-angle versus horizontal centrifugation. Platelets. 32:413–419. https://doi.org/10.1080/09537104.2020.1754382
Benic GI, Eisner BM, Jung RE, Basler T, Schneider D, Hämmerle CHF (2019) Hard tissue change after guided bone regeneration after peri-implant defects comparing block versus particulate bone substitutes: 6 months results of randomized controlled trial. Clin Oral Implants Res 30:1016–1026. https://doi.org/10.1111/clr.13515
Elnayef B, Porta C, Suárez-López Del Amo F, Mordini L, Gargallo-Albiol J, Hernández-Alfaro F (2018) The fate of lateral ridge augmentation: a systematic review and meta-analysis. Int J Oral Maxillofac Implants 33:622–635. https://doi.org/10.11607/jomi.6290
Nizam N, Eren G, Akçalı A, Donos N (2018) Maxillary sinus augmentation with leukocyte and platelet-rich fibrin and deproteinized bovine bone mineral: a split-mouth histological and histomorphometric study. Clin Oral Implants Res 29:67–75. https://doi.org/10.1111/clr.13044
Scarano A, Inchingolo F, Murmura G, Traini T, Piattelli A, Lorusso F (2018) Three-dimensional architecture and mechanical properties of bovine bone mixed with autologous platelet liquid, blood, or physiological water: an in vitro study. Int J Mol Sci 19:1230. https://doi.org/10.3390/ijms19041230
Koller CD, Pereira-Cenci T, Boscato N (2016) Parameters associated with marginal bone loss around implant after prosthetic loading. Braz Dent J 27:292–297. https://doi.org/10.1590/0103-6440201600874
Author information
Authors and Affiliations
Contributions
G.I. and T.G. conceived the ideas and planned the research; T.G. performed the surgeries; M.O.Y and N.K.T collected the data; G.I. led the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
All procedures carried out in the course of the studies involving human participants were in accordance with the ethical standards of the institutional research committee (No: 17-12.1/34) and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOC 220 kb)
Rights and permissions
About this article
Cite this article
Işık, G., Özden Yüce, M., Koçak-Topbaş, N. et al. Guided bone regeneration simultaneous with implant placement using bovine-derived xenograft with and without liquid platelet-rich fibrin: a randomized controlled clinical trial. Clin Oral Invest 25, 5563–5575 (2021). https://doi.org/10.1007/s00784-021-03987-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03987-5