Abstract
Background and objective
The resorption of alveolar ridge bone and maxillary sinus pneumatization are challenges to implant-supported prosthetic rehabilitation. Bone regeneration using bone substitutes and growth factors are alternatives for maxillary sinus augmentation (MSA). Therefore, we sought to evaluate the effects of the association between leukocyte and platelet–rich fibrin (L-PRF) and deproteinized bovine bone mineral (DBBM) in MSA procedures.
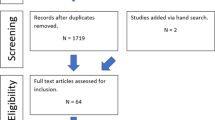
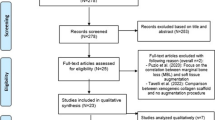
Materials and methods
Thirty-six maxillary sinuses from 24 individuals were included in this randomized clinical trial. The maxillary sinuses were randomly grafted with LPRF and DBBM (test group) or grafted only with DBBM (positive control). Dental implants were installed in the test group following two periods of evaluation: after 4 (DBBM+LPRF4) and 8 (DBBM+LPFR8) months of sinus graft healing, while the control group received implants only after 8 months. Cone beam computed tomography (CBCT) was taken 1 week after surgery (T1) and before implant placement (T2). Bone samples were collected during implant placement for histomorphometric and immunohistochemical (IHC) analysis. The primary implant stability was assessed by resonance frequency analysis.
Results
CBCT analysis demonstrated a significant decrease in bone volume from T1 to T2 in all groups without differences among them. Histologically, the test group showed significantly increase in bone neoformation in both periods of evaluation (LPRF+DBBM4: 44.70±14.01%; LPRF+DBBM8: 46.56±12.25%) compared to the control group (32.34±9.49%). The control group showed the highest percentage of residual graft. IHC analysis showed increased staining intensity of osteocalcin (OCN), vascular endothelial growth factor (VEGF), and runt related transcription factor 2 (RUNX-2) in LPRF+DBBM4 group, and osteopontin (OPN) in the L-PRF+DBBM8. Primary implant stability was successfully achieved (above 60 in implant stability quotient) in all the evaluated groups.
Conclusion
Combination of L-PRF and DBBM increased and accelerated new bone formation allowing early implant placement probably due to the higher protein expression of RUNX2, VEGF, OCN, and OPN. These data suggest that the use of L-PRF might be an interesting alternative to use in combination with DBBM for augment the maxillary sinuses allowing the installation of appropriate length implants in shorter period of time.
Clinical relevance
This study showed improvement in bone neoformation and accelerated healing when associating L-PRF and DBBM for maxillary sinus augmentation procedures.
Trial registration
This study was registered before participant recruitment in Brazilian Registry of Clinical Trials (ReBEC - RBR-95m73t).







Similar content being viewed by others
Data availability
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
References
Boyne PJ, James RA (1980) Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 38:613–616
Tatum H Jr (1986) Maxillary and sinus implant reconstructions. Dent Clin North Am 30:207–229
Ocak H, Kutuk N, Demetoglu U, Balcioglu E, Ozdamar S, Alkan A (2017) Comparison of bovine bone-autogenic bone mixture versus platelet-rich fibrin for maxillary sinus grafting: histologic and histomorphologic study. J Oral Implantol 43:194–201. https://doi.org/10.1563/aaid-joi-D-16-00104
Palma VC, Magro-Filho O, de Oliveria JA, Lundgren S, Salata LA, Sennerby L (2006) Bone reformation and implant integration following maxillary sinus membrane elevation: an experimental study in primates. Clin Implant Dent Relat Res 8:11–24. https://doi.org/10.2310/j.6480.2005.00026.x
Srouji S, Ben-David D, Lotan R, Riminucci M, Livne E, Bianco P (2010) The innate osteogenic potential of the maxillary sinus (Schneiderian) membrane: an ectopic tissue transplant model simulating sinus lifting. Int J Oral Maxillofac Surg 39:793–801. https://doi.org/10.1016/j.ijom.2010.03.009
Srouji S, Kizhner T, Ben David D, Riminucci M, Bianco P, Livne E (2009) The Schneiderian membrane contains osteoprogenitor cells: in vivo and in vitro study. Calcif Tissue Int 84:138–145. https://doi.org/10.1007/s00223-008-9202-x
Sul SH, Choi BH, Li J, Jeong SM, Xuan F (2008) Effects of sinus membrane elevation on bone formation around implants placed in the maxillary sinus cavity: an experimental study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:684–687. https://doi.org/10.1016/j.tripleo.2007.09.024
de Molon RS, Magalhaes-Tunes FS, Semedo CV, Furlan RG, de Souza LGL, de Souza Faloni AP, Marcantonio E Jr, Faeda RS (2019) A randomized clinical trial evaluating maxillary sinus augmentation with different particle sizes of demineralized bovine bone mineral: histological and immunohistochemical analysis. Int J Oral Maxillofac Surg 48:810–823. https://doi.org/10.1016/j.ijom.2018.09.003
Dos Anjos TL, de Molon RS, Paim PR, Marcantonio E, Marcantonio E Jr, Faeda RS (2016) Implant stability after sinus floor augmentation with deproteinized bovine bone mineral particles of different sizes: a prospective, randomized and controlled split-mouth clinical trial. Int J Oral Maxillofac Surg 45:1556–1563. https://doi.org/10.1016/j.ijom.2016.09.004
Pichotano EC, de Molon RS, Freitas de Paula LG, de Souza RV, Marcantonio E Jr, Zandim-Barcelos DL (2018) Early placement of dental implants in maxillary sinus grafted with leukocyte and platelet-rich fibrin and deproteinized bovine bone mineral. J Oral Implantol 44:199–206. https://doi.org/10.1563/aaid-joi-D-17-00220
Dos Santos PL, de Molon RS, Queiroz TP, Okamoto R, de Souza Faloni AP, Gulinelli JL, Luvizuto ER, Garcia IR Jr (2016) Evaluation of bone substitutes for treatment of peri-implant bone defects: biomechanical, histological, and immunohistochemical analyses in the rabbit tibia. J Periodontal Implant Sci 46:176–196. https://doi.org/10.5051/jpis.2016.46.3.176
Kim YJ, de Molon RS, Horiguti FR, Contador GP, Coelho MA, Mascarenhas VI, de Souza Faloni AP, Cirelli JA, Sendyk WR (2018) Vertical bone augmentation using deproteinized bovine bone mineral, absorbable collagen sponge, and recombinant human bone morphogenetic protein-2: an in vivo study in rabbits. Int J Oral Maxillofac Implants 33:512–522. https://doi.org/10.11607/jomi.5959
Jensen T, Schou S, Stavropoulos A, Terheyden H, Holmstrup P (2012) Maxillary sinus floor augmentation with Bio-Oss or Bio-Oss mixed with autogenous bone as graft in animals: a systematic review. Int J Oral Maxillofac Surg 41:114–120. https://doi.org/10.1016/j.ijom.2011.08.010
Simonpieri A, Choukroun J, Del Corso M, Sammartino G, Dohan Ehrenfest DM (2011) Simultaneous sinus-lift and implantation using microthreaded implants and leukocyte- and platelet-rich fibrin as sole grafting material: a six-year experience. Implant Dent 20:2–12. https://doi.org/10.1097/ID.0b013e3181faa8af
Tajima N, Ohba S, Sawase T, Asahina I (2013) Evaluation of sinus floor augmentation with simultaneous implant placement using platelet-rich fibrin as sole grafting material. Int J Oral Maxillofac Implants 28:77–83. https://doi.org/10.11607/jomi.2613
Browaeys H, Bouvry P, De Bruyn H (2007) A literature review on biomaterials in sinus augmentation procedures. Clin Implant Dent Relat Res 9:166–177. https://doi.org/10.1111/j.1708-8208.2007.00050.x
Zerbo IR, de Lange GL, Joldersma M, Bronckers AL, Burger EH (2003) Fate of monocortical bone blocks grafted in the human maxilla: a histological and histomorphometric study. Clin Oral Implants Res 14:759–766. https://doi.org/10.1046/j.0905-7161.2003.00967.x
Pinchasov G, Juodzbalys G (2014) Graft-free sinus augmentation procedure: a literature review. J Oral Maxillofac Res 5:e1. https://doi.org/10.5037/jomr.2014.5101
Choukroun J, Diss A, Simonpieri A, Girard MO, Schoeffler C, Dohan SL, Dohan AJ, Mouhyi J, Dohan DM (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part V: histologic evaluations of PRF effects on bone allograft maturation in sinus lift. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:299–303. https://doi.org/10.1016/j.tripleo.2005.07.012
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part I: technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e37–e44. https://doi.org/10.1016/j.tripleo.2005.07.008
Nizam N, Eren G, Akcali A, Donos N (2018) Maxillary sinus augmentation with leukocyte and platelet-rich fibrin and deproteinized bovine bone mineral: a split-mouth histological and histomorphometric study. Clin Oral Implants Res 29:67–75. https://doi.org/10.1111/clr.13044
Pichotano EC, de Molon RS, de Souza RV, Austin RS, Marcantonio E, Zandim-Barcelos DL (2019) Evaluation of L-PRF combined with deproteinized bovine bone mineral for early implant placement after maxillary sinus augmentation: a randomized clinical trial. Clin Implant Dent Relat Res 21:253–262. https://doi.org/10.1111/cid.12713
Tadjoedin ES, de Lange GL, Bronckers AL, Lyaruu DM, Burger EH (2003) Deproteinized cancellous bovine bone (Bio-Oss) as bone substitute for sinus floor elevation. A retrospective, histomorphometrical study of five cases. J Clin Periodontol 30:261–270. https://doi.org/10.1034/j.1600-051x.2003.01099.x
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part III: leucocyte activation: a new feature for platelet concentrates? Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e51–e55. https://doi.org/10.1016/j.tripleo.2005.07.010
Liu R, Yan M, Chen S, Huang W, Wu D, Chen J (2019) Effectiveness of platelet-rich fibrin as an adjunctive material to bone graft in maxillary sinus augmentation: a meta-analysis of randomized controlled trails. Biomed Res Int 2019:7267062. https://doi.org/10.1155/2019/7267062
Strauss FJ, Stahli A, Gruber R (2018) The use of platelet-rich fibrin to enhance the outcomes of implant therapy: a systematic review. Clin Oral Implants Res 29(Suppl 18):6–19. https://doi.org/10.1111/clr.13275
Zhang Y, Tangl S, Huber CD, Lin Y, Qiu L, Rausch-Fan X (2012) Effects of Choukroun's platelet-rich fibrin on bone regeneration in combination with deproteinized bovine bone mineral in maxillary sinus augmentation: a histological and histomorphometric study. J Craniomaxillofac Surg 40:321–328. https://doi.org/10.1016/j.jcms.2011.04.020
Shiezadeh F, Taher M, Shooshtari Z, Arab H, Shafieian R (2023) Using platelet-rich fibrin in combination with allograft bone particles can induce bone formation in maxillary sinus augmentation. J Oral Maxillofac Surg. https://doi.org/10.1016/j.joms.2023.03.015
Powell CA, Casarez-Quintana A, Zellner J, Al-Bayati O, Font K (2022) The application of leukocyte- and platelet-rich fibrin (L-PRF) in maxillary sinus augmentation. Clin Adv Periodontics 12:277–286. https://doi.org/10.1002/cap.10216
de Molon RS, de Paula WN, Spin-Neto R, Verzola MH, Tosoni GM, Lia RC, Scaf G, Marcantonio E Jr (2015) Correlation of fractal dimension with histomorphometry in maxillary sinus lifting using autogenous bone graft. Braz Dent J 26:11–18. https://doi.org/10.1590/0103-6440201300290
Guastaldi FPS, Queiroz TP, Marques DO, Santos ABS, Molon RS, Margonar R, Guastaldi AC (2021) Comparative evaluation of implants with different surface treatments placed in human edentulous mandibles: a 1-year prospective study. J Maxillofac Oral Su. https://doi.org/10.1007/s12663-021-01600-6
do Lago ES, Ferreira S, Garcia IR Jr, Okamoto R, Mariano RC (2020) Improvement of bone repair with l-PRF and bovine bone in calvaria of rats. histometric and immunohistochemical study. Clin Oral Investig 24:1637–1650. https://doi.org/10.1007/s00784-019-03018-4
Pereira RS, Gorla LF, Boos F, Okamoto R, Garcia Junior IR, Hochuli-Vieira E (2017) Use of autogenous bone and beta-tricalcium phosphate in maxillary sinus lifting: histomorphometric study and immunohistochemical assessment of RUNX2 and VEGF. Int J Oral Maxillofac Surg 46:503–510. https://doi.org/10.1016/j.ijom.2017.01.002
Pedrosa WF Jr, Okamoto R, Faria PE, Arnez MF, Xavier SP, Salata LA (2009) Immunohistochemical, tomographic and histological study on onlay bone graft remodeling. Part II: calvarial bone. Clin Oral Implants Res 20:1254–1264. https://doi.org/10.1111/j.1600-0501.2009.01747.x
Anitua E (1999) Plasma rich in growth factors: preliminary results of use in the preparation of future sites for implants. Int J Oral Maxillofac Implants 14:529–535
Dohan Ehrenfest DM, Rasmusson L, Albrektsson T (2009) Classification of platelet concentrates: from pure platelet-rich plasma (P-PRP) to leucocyte- and platelet-rich fibrin (L-PRF). Trends Biotechnol 27:158–167. https://doi.org/10.1016/j.tibtech.2008.11.009
van Hinsbergh VW, Collen A, Koolwijk P (2001) Role of fibrin matrix in angiogenesis. Ann N Y Acad Sci 936:426–437. https://doi.org/10.1111/j.1749-6632.2001.tb03526.x
Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Gogly B (2006) Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part II: platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101:e45–e50. https://doi.org/10.1016/j.tripleo.2005.07.009
Everts PA, van Zundert A, Schonberger JP, Devilee RJ, Knape JT (2008) What do we use: platelet-rich plasma or platelet-leukocyte gel? J Biomed Mater Res A 85:1135–1136. https://doi.org/10.1002/jbm.a.31570
Tatullo M, Marrelli M, Cassetta M, Pacifici A, Stefanelli LV, Scacco S, Dipalma G, Pacifici L, Inchingolo F (2012) Platelet rich fibrin (P.R.F.) in reconstructive surgery of atrophied maxillary bones: clinical and histological evaluations. Int J Med Sci 9:872–880. https://doi.org/10.7150/ijms.5119
Castro AB, Meschi N, Temmerman A, Pinto N, Lambrechts P, Teughels W, Quirynen M (2017) Regenerative potential of leucocyte- and platelet-rich fibrin. Part A: intra-bony defects, furcation defects and periodontal plastic surgery. A systematic review and meta-analysis. J Clin Periodontol 44:67–82. https://doi.org/10.1111/jcpe.12643
Degidi M, Daprile G, Piattelli A (2012) Primary stability determination by means of insertion torque and RFA in a sample of 4,135 implants. Clin Implant Dent Relat Res 14:501–507. https://doi.org/10.1111/j.1708-8208.2010.00302.x
Meredith N (1998) Assessment of implant stability as a prognostic determinant. Int J Prosthodont 11:491–501
Sennerby L, Meredith N (2000) (2008) Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 47:51–66. https://doi.org/10.1111/j.1600-0757.2008.00267.x
Nedir R, Bischof M, Szmukler-Moncler S, Bernard JP, Samson J (2004) Predicting osseointegration by means of implant primary stability. Clin Oral Implants Res 15:520–528. https://doi.org/10.1111/j.1600-0501.2004.01059.x
Shanbhag S, Shanbhag V, Stavropoulos A (2014) Volume changes of maxillary sinus augmentations over time: a systematic review. Int J Oral Maxillofac Implants 29:881–892. https://doi.org/10.11607/jomi.3472
Acknowledgements
The authors would like to thank Geistlich Pharma AG® (Wolhusen, Switzerland) for the free donation of Bio-Oss® and BioGide® membranes, and Neodent® (Curitiba, PR, Brazil) for the donation of the implants.
Funding
Carolina M. de Almeida Malzoni and Elton Carlos Pichotano were supported by grant provided by CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior).
Author information
Authors and Affiliations
Contributions
Carolina Mendonca de Almeida Malzoni: methodology, conceptualization, formal analysis, writing — original draft, writing — review and editing, visualization, final approval of the submitted version; Elton Carlos Pichotano: methodology, formal analysis, writing — review and editing, visualization, final approval of the submitted version; Luis Guilherme Freitas de Paula: methodology, conceptualization, supervision, formal analysis, writing — review and editing, visualization, final approval of the submitted version; Ricardo Violante de Souza: methodology, formal analysis, writing — review and editing, visualization, final approval of the submitted version; Roberta Okamoto: methodology, formal analysis, writing — review and editing, visualization, final approval of the submitted version; Elcio Marcantonio Jr: methodology, conceptualization, supervision, formal analysis, writing — review and editing, visualization, final approval of the submitted version; Rupert S. Austin: methodology, formal analysis, writing — review and editing, visualization, final approval of the submitted version; Rafael Scaf de Molon: methodology, formal analysis, writing — original draft, writing — review and editing, visualization, final approval of the submitted version; Daniela Leal Zandim-Barcelos: methodology, formal analysis, conceptualization, supervision, writing — review and editing, visualization, final approval of the submitted version
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
This study was approved by the Human Research Ethics Committee of the School of Dentistry at Araraquara (CAAE #41357514.5.0000.5416) and was performed in accordance with the principles stated in the Declaration of Helsinki in 1964. Furthermore, this clinical trial was registered before participant recruitment in Brazilian Registry of Clinical Trials (ReBEC - RBR-95m73t).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Almeida Malzoni, C.M., Pichotano, E.C., Freitas de Paula, L.G. et al. Combination of leukocyte and platelet–rich fibrin and demineralized bovine bone graft enhanced bone formation and healing after maxillary sinus augmentation: a randomized clinical trial. Clin Oral Invest 27, 5485–5498 (2023). https://doi.org/10.1007/s00784-023-05167-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-023-05167-z