Abstract
Objective
This prospective clinical study compares postoperative pain after single-visit, non-surgical root canal treatment of teeth with irreversible pulpitis using two different root canal filling techniques.
Material and methods
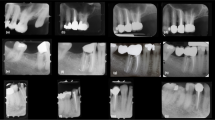
All cases were treated by endodontic residents with a standardized protocol (minimum apical size 35) and filled with one of the two techniques: warm vertical compaction technique (WVT) with gutta percha and epoxy resin-based sealer (AH Plus Jet Root Canal Sealer, Dentsply Maillefer, York, PA, USA) or sealer-based filling technique (SBT) with single cone gutta percha and calcium silicate-based sealer (EndoSequence BC Sealer, Brasseler, Savannah, GA, USA). Surveys were given to participating patients to record pain intensity on a numeric rating scale (NRS, 0–10) at 4, 24, and 48 h postoperatively. Statistical significance was set at 0.05 level.
Results
One hundred ninety-four surveys were distributed over eighteen months. Ninety-two patients returned the survey (41 WVT and 51 SBT), of which 38% were asymptomatic irreversible pulpitis cases. The NRS values reduced over time for both techniques. No statistical difference was found between the two groups at the three time points assessed (p > 0.05). Postoperative pain was related to age, gender, presence of preoperative pain, and sealer extrusion (p < 0.05), however not related to preoperative periapical symptoms (percussion/palpation), dental arch, root type, and experience of the provider (p > 0.05).
Conclusions
The intensity of postoperative pain for the two obturation techniques was equivalent at evaluated time points.
Clinical relevance
The obturation technique does not influence postoperative pain. After endodontic treatment of symptomatic irreversible pulpitis teeth, the pain subsides in 48 h regardless of the technique.
Trial registration
ClinicalTrials.gov ID: NCT04462731





Similar content being viewed by others
References
Harrison JW, Baumgartner JC, Svec TA (1983) Incidence of pain associated with clinical factors during and after root canal therapy. Part 2. Postobturation pain. J Endod 9:434–438. https://doi.org/10.1016/S0099-2399(83)80259-3
Nixdorf DR, Moana-Filho EJ, Law AS et al (2010) Frequency of persistent tooth pain after root canal therapy: a systematic review and meta-analysis. J Endod 36:224–230. https://doi.org/10.1016/j.joen.2009.11.007
Pak JG, White SN (2011) Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J Endod 37:429–438. https://doi.org/10.1016/j.joen.2010.12.016
Arslan H, Güven Y, Karataş E, Doğanay E (2017) Effect of the simultaneous working length control during root canal preparation on postoperative pain. J Endod 43:1422–1427. https://doi.org/10.1016/j.joen.2017.04.028
Gondim E, Setzer FC, Dos Carmo CB, Kim S (2010) Postoperative pain after the application of two different irrigation devices in a prospective randomized clinical trial. J Endod 36:1295–1301. https://doi.org/10.1016/j.joen.2010.04.012
Nekoofar MH, Sheykhrezae MS, Meraji N et al (2015) Comparison of the effect of root canal preparation by using waveone and protaper on postoperative pain: a randomized clinical trial. J Endod 41:575–578. https://doi.org/10.1016/j.joen.2014.12.026
Topçuoğlu HS, Topçuoğlu G, Arslan H (2018) The effect of different irrigation agitation techniques on postoperative pain in mandibular molar teeth with symptomatic irreversible pulpitis: a randomized clinical trial. J Endod 44:1451–1456. https://doi.org/10.1016/j.joen.2018.06.008
Farzaneh S, Parirokh M, Nakhaee N, Abbott PV (2018) Effect of two different concentrations of sodium hypochlorite on postoperative pain following single-visit root canal treatment: a triple-blind randomized clinical trial. Int Endod J 51:e2–e11. https://doi.org/10.1111/iej.12749
DiRenzo A, Gresla T, Johnson BR et al (2002) Postoperative pain after 1- and 2-visit root canal therapy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93:605–610. https://doi.org/10.1067/moe.2002.121900
Ehrmann EH, Messer HH, Adams GG (2003) The relationship of intracanal medicaments to postoperative pain in endodontics. Int Endod J 36:868–875. https://doi.org/10.1111/j.1365-2591.2003.00735.x
Alonso-Ezpeleta LOL, Gasco-Garcia C, Castellanos-Cosano L et al (2012) Postoperative pain after one-visit root-canal treatment on teeth with vital pulps: comparison of three different obturation techniques. Med Oral Patol Oral Cir Bucal 17:e721–e727. https://doi.org/10.4317/medoral.17898
Sahito N, Dal AQ, Qureshi A (2014) A clinical study of the post operative pain after root canal obturation with Obtura-Ii & System-B, warm gutta-percha techniques. J Am Sci 10:11–14
Rosenberg PA, Babick PJ, Schertzer L, Leung A (1998) The effect of occlusal reduction on pain after endodontic instrumentation. J Endod 24:492–496. https://doi.org/10.1016/S0099-2399(98)80054-X
Alaçam T (1985) Incidence of postoperative pain following the use of different sealers in immediate root canal filling. J Endod 11:135–137. https://doi.org/10.1016/S0099-2399(85)80233-8
Atav Ates A, Dumani A, Yoldas O, Unal I (2019) Post-obturation pain following the use of carrier-based system with AH Plus or iRoot SP sealers: a randomized controlled clinical trial. Clin Oral Investig 23:3053–3061. https://doi.org/10.1007/s00784-018-2721-6
Nabi S, Farooq R, Purra A, Ahmed F (2019) Comparison of various sealers on postoperative pain in single-visit endodontics: a randomized clinical study. Indian J Dent Sci 11:99–102. https://doi.org/10.4103/IJDS.IJDS_81_18
Loushine BA, Bryan TE, Looney SW et al (2011) Setting properties and cytotoxicity evaluation of a premixed bioceramic root canal sealer. J Endod. https://doi.org/10.1016/j.joen.2011.01.003
Silva Almeida LH, Moraes RR, Morgental RD, Pappen FG (2017) Are premixed calcium silicate-based endodontic sealers comparable to conventional materials? A systematic review of in vitro studies. J Endod 43:527–535. https://doi.org/10.1016/j.joen.2016.11.019
Chybowski EA, Glickman GN, Patel Y et al (2018) Clinical outcome of non-surgical root canal treatment using a single-cone technique with endosequence bioceramic sealer: a retrospective analysis. J Endod 44:941–945. https://doi.org/10.1016/j.joen.2018.02.019
Graunaite I, Skucaite N, Lodiene G et al (2018) Effect of resin-based and bioceramic root canal sealers on postoperative pain: a split-mouth randomized controlled trial. J Endod 44:689–693. https://doi.org/10.1016/j.joen.2018.02.010
Tan HSG, Lim KC, Lui JN et al (2020) Postobturation pain associated with tricalcium silicate and resin-based sealer techniques: a randomized clinical trial. J Endod. https://doi.org/10.1016/j.joen.2020.10.013
Liang K-Y, Zeger SL (1986) Longitudinal data analysis using generalized linear models. Biometrika 73:13. https://doi.org/10.2307/2336267
Alí A, Olivieri JG, Duran-Sindreu F et al (2016) Influence of preoperative pain intensity on postoperative pain after root canal treatment: a prospective clinical study. J Dent 45:39–42. https://doi.org/10.1016/j.jdent.2015.12.002
Michaelson PL, Holland GR (2002) Is pulpitis painful? Int Endod J 35:829–832. https://doi.org/10.1046/j.1365-2591.2002.00579.x
Robinson ME, Riley JL, Myers CD et al (2001) Gender role expectations of pain: relationship to sex differences in pain. J Pain 2:251–257. https://doi.org/10.1054/jpai.2001.24551
Bartley EJ, Fillingim RB (2013) Sex differences in pain: a brief review of clinical and experimental findings. Br J Anaesth 111:52–58. https://doi.org/10.1093/bja/aet127
Paulson PE, Minoshima S, Morrow TJ, Casey KL (1998) Gender differences in pain perception and patterns of cerebral activation during noxious heat stimulation in humans. Pain 76:223–229. https://doi.org/10.1016/s0304-3959(98)00048-7
Liddell A, Locker D (1997) Gender and age differences in attitudes to dental pain and dental control. Community Dent Oral Epidemiol 25:314–318. https://doi.org/10.1111/j.1600-0528.1997.tb00945.x
Trope M, Bunes A, Debelian G (2015) Root filling materials and techniques: bioceramics a new hope? Endod Top 32:86–96. https://doi.org/10.1111/etp.12074
Ørstavik D, Nordahl I, Tibballs JE (2001) Dimensional change following setting of root canal sealer materials. Dent Mater 17:512–519. https://doi.org/10.1016/S0109-5641(01)00011-2
Zhou H, Shen Y, Zheng W et al (2013) Physical properties of 5 root canal sealers. J Endod 39:1281–1286. https://doi.org/10.1016/j.joen.2013.06.012
Ricucci D, Rôças IN, Alves FRF et al (2016) Apically extruded sealers: fate and influence on treatment outcome. J Endod 42:243–249. https://doi.org/10.1016/j.joen.2015.11.020
Sari Ş, Durutűrk L (2007) Radiographic evaluation of periapical healing of permanent teeth with periapical lesions after extrusion of AH Plus sealer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104:e54–e59. https://doi.org/10.1016/j.tripleo.2007.03.024
Augsburger RA, Peters DD (1990) Radiographic evaluation of extruded obturation materials. J Endod 16:492–497. https://doi.org/10.1016/S0099-2399(07)80179-8
Nair PNR, Sjögren U, Krey G, Sundqvist G (1990) Therapy-resistant foreign body giant cell granuloma at the periapex of a root-filled human tooth. J Endod 16:589–595. https://doi.org/10.1016/S0099-2399(07)80202-0
Scarparo RK, Grecca FS, Fachin EVF (2009) Analysis of tissue reactions to methacrylate resin-based, epoxy resin-based, and zinc oxide–eugenol endodontic sealers. J Endod 35:229–232. https://doi.org/10.1016/j.joen.2008.10.025
Ricucci D, Grande NM, Plotino G, Tay FR (2020) Histologic response of human pulp and periapical tissues to tricalcium silicate–based materials: a series of successfully treated cases. J Endod 46:307–317. https://doi.org/10.1016/j.joen.2019.10.032
Zhang W, Peng B (2015) Tissue reactions after subcutaneous and intraosseous implantation of iRoot SP, MTA and AH Plus. Dent Mater J 34:774–780. https://doi.org/10.4012/dmj.2014-271
Laux M, Abbott PV, Pajarola G, Nair PNR (2000) Apical inflammatory root resorption: a correlative radiographic and histological assessment. Int Endod J 33:483–493. https://doi.org/10.1046/j.1365-2591.2000.00338.x
Ruparel NB, Ruparel SB, Chen PB et al (2014) Direct effect of endodontic sealers on trigeminal neuronal activity. J Endod 40:683–687. https://doi.org/10.1016/j.joen.2014.01.030
Myles PS, Myles DB, Galagher W et al (2017) Measuring acute postoperative pain using the visual analog scale: the minimal clinically important difference and patient acceptable symptom state. Br J Anaesth 118:424–429. https://doi.org/10.1093/bja/aew466
Johnsen DC, Harshbarger J, Rymer HD (1983) Quantitative assessment of neural development in human premolars. Anat Rec 205:421–429. https://doi.org/10.1002/ar.1092050407
Bernick S, Nedelman C (1975) Effect of aging on the human pulp. J Endod 1:88–94. https://doi.org/10.1016/S0099-2399(75)80024-0
Gomes MS, Böttcher DE, Scarparo RK et al (2017) Predicting pre- and postoperative pain of endodontic origin in a southern Brazilian subpopulation: an electronic database study. Int Endod J 50:729–739. https://doi.org/10.1111/iej.12684
Axelrod DA, Hayward R (2007) Nonrandomized interventional study designs (quasi-experimental designs). In: Clinical research methods for surgeons. Humana Press, Totowa, pp 63–76
Cobanoglu C, Moreo PJ, Warde B (2001) A comparison of mail, fax and web-based survey methods. Int J Mark Res 43:1–15. https://doi.org/10.1177/147078530104300401
Converse PD, Wolfe EW, Huang X, Oswald FL (2008) Response rates for mixed-mode surveys using mail and e-mail/web. Am J Eval 29:99–107. https://doi.org/10.1177/1098214007313228
Fowler FJ, Cosenza C, Cripps LA et al (2019) The effect of administration mode on CAHPS survey response rates and results: a comparison of mail and web-based approaches. Health Serv Res 54:714–721. https://doi.org/10.1111/1475-6773.13109
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yu, YH., Kushnir, L., Kohli, M. et al. Comparing the incidence of postoperative pain after root canal filling with warm vertical obturation with resin-based sealer and sealer-based obturation with calcium silicate-based sealer: a prospective clinical trial. Clin Oral Invest 25, 5033–5042 (2021). https://doi.org/10.1007/s00784-021-03814-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-021-03814-x