Abstract
Introduction
This study evaluated the reproducibility of electronic color determination system evaluations of the marginal gingiva, which could be important for adhesive cervical fillings or prosthetic restorations that imitate the gingiva.
Material and methods
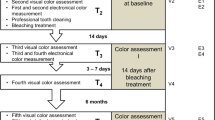
In 50 subjects, the L*, a*, and b* color coordinates were evaluated five times at a point in the marginal area of a central incisor using different electronic color determination systems: (SP) Shadepilot, (ES) Easyshade, (CE) Crystaleye, and (SV) X-Rite. The mean color difference (ΔE) and its standard deviation between the five measurements from each participant were calculated separately for each device. Further ICC for interdevice reliability was determined.
Results
The L*, a*, and b* color coordinates and ΔE values differed significantly among the systems (p < 0.001). Within each patient and measurement system, ΔE ranged from 1.4 to 3.2 (SD 1.1–2.5), L* from 2.6 to 5.7 (SD 2.6–5.7), a* from 11.9 to 21.3 (SD 3.6–3.9), and b* from 15.1 to 28.9 (SD 1.7–4.3). Interdevice reliability ranged between 0.675 and 0.807.
Conclusions
Color determination of the marginal gingiva using the electronic tooth color determination systems tested herein showed limited reproducibility. The results obtained with the different measurement systems differed enormously.
Clinical relevance
These results show that the electronic color measurement devices tested allow no high reproducible determination of color coordinates of the marginal gingiva.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As society ages and more people retain their natural teeth, the incidence of anterior restorations continues to increase, particularly cervical fillings; thus, Class V restorations are increasingly necessary for oral rehabilitation [1, 2]. Class V restorations are applied in areas of occlusal dysfunction and abrasive processes, where the fillings must withstand shrinkage of the resin material and bonding and deformation during static and dynamic occlusal dysfunction [3, 4]. Composite restorations created in this context often require esthetic color adjustment [5]. Typically, color matching refers to the color of the affected tooth. However, in certain situations, to avoid surgical treatment [6], it may be beneficial to use gingiva-colored composites or ceramic materials to achieve better esthetic results and the ideal proportions of red and white [7, 8]. Consequently, color matching of the marginal gingiva is necessary and it is a challenge to achieve color harmonization for natural-looking teeth.
Traditionally, to match tooth or gingival color, the dentist referred to color keys to identify the target color [9]. In the last decade, however, color-measuring devices have been used to overcome the disadvantages of visual color matching, which include observer factors like color blindness, fatigue, light conditions, and health impairments. These color-measurement devices have the potential to detect colors more precisely and reproducibly, by determining the color coordinates and dental color shades and calculating the color differences (ΔE) between objects [10,11,12,13,14,15,16,17,18]. The ΔE values are calculated using formulas that enable quantitative evaluation of ΔE. The most frequently used formula is derived from the CIE L*a*b* system. Several studies have reported ΔE thresholds that are clinical acceptable and result in perceptible ΔE [19]. Indeed, 50% of examiners are able to perceive a ΔE value < 1 when observing opal monochromatic samples under controlled conditions. Therefore, the minimum ΔE for discriminating a mismatch between the composite and tooth color in the oral cavity varies from study to study [20]. Although electronic shade-measuring systems are used for color determination, few studies have evaluated the reproducibility of electronic gingival color determination, particularly in the context of adhesive restorations of Class V defects [2, 21, 22].
Therefore, this study evaluated the reproducibility of electronic color-determination system evaluations of the marginal gingiva (Figs. 1).
Materials and methods
Color-measuring devices
This study examined four commercial dental color-measuring devices (Table 1) with different operating modes: Shadepilot (SP) (Figs. 2a, Hanau, Germany) the Easyshade Advance (ES) (Fig. 4; VITA Zahnfabrik H. Rauter GmbH & Co. KG, Bad Säckingen, Germany); (Figs. 2c, (CE) (Fig. 5) Olympus America, Center Valley, PA, USA); and X-Rite ShadeVision (SV) ((Figs. 2d) X-Rite, Grand Rapids, MI, USA) [13, 15]. Table 1 summarizes the specifications of the devices. Each device was used according to the manufacturer’s instructions and this investigation was performed in terms of quality assurance. Of the four devices, the SP, ES, and CE are spectrophotometric devices and the SV is a colorimetric device; all have different operating modes.
All measurements were performed under the same standardized test conditions by one trained operator (five measurements per tooth) during restorative and prosthetic restorations (Fig. 3a, b)
The electronic device SP was calibrated using the white and green calibration tiles provided by the manufacturer before obtaining images of teeth. The optical hand piece was held at 90° to the target tooth and flush against the gingival matrix. The SP device measured the CIE L*a*b* values for each tooth and automatically selected the closed shade tab from the internal database of the manufacturer. Tooth analysis mode was chosen and the color coordinates of the marginal area of the tooth 11 were recorded by manual selection. The ES system was calibrated using the white calibration standard as per the manufacturer’s instructions, with the hand piece in its stand. Tooth area analysis mode was used and only the color information of a point of the marginal area of the tooth 11 were analyzed. The CE system was calibrated using the calibration plate on the docking station before measurements and the device was positioned to capture the tooth image. Spectral data for the cervical, central, and incisal thirds of the tooth were analyzed. The best shade match obtained with the VC-system, and CIE L*a*b* values, was calculated for a point of the marginal gingiva of the tooth 11. The SV device, calibrated on the docking station before and between tooth measurements, measured the selected point of the marginal gingiva of the tooth 11.
Patients
This study enrolled 50 patients (34 females, 16 males, age 22-29 years (mean age: 24.8 years), which received. During measurements, they were instructed to place their heads against the headrest of a dental chair and relax. The color measurement devices were used and calibrated according to the manufacturers’ instructions. The CIE L*a*b* values were recorded five times for each patient without removal of the instruments. The region of interest was a point of the gingiva with a distance of 2 mm to the gingival margin considering the tooth axis of the tooth 11. Patients with abnormal discoloration were excluded. All patients underwent a professional tooth cleaning before the examination.
Test conditions
All measurements were made by a single trained operator under standardized test conditions to avoid external influences. The operator was trained to keep the measuring points during the measurements. A repositioning jig was not used. The illumination source (Just Normlicht, Weilheim an der Teck, Germany) was set at 6,500 K and 1,000 Lux. Natural daylight was excluded using an opaque optical louver. The shade of slightly moistened gingiva was examined and the patient’s clothing was covered with a cloth to minimize visual interference.
Statistical analyses
The data were imported into SPSS ver. 19.0 (SPSS, Chicago, IL, USA) or SAS ver. 9.2 (SAS Institute, Cary, NC, USA). Reproducibility was assessed by calculating the mean and standard deviation (SD) of the color coordinates (L*, a*, and b*) with each color measuring system. The color distances (ΔE) among the measurements were calculated for each patient and each device using the following equation:
where i and ii are two different measurements [18]. The color coordinates of the color-measuring devices were compared using analysis of variance (ANOVA) with the Bonferroni adjustment to control for multiple testing. P values < 0.016 were deemed to indicate significance. Further intraclass correlation coefficients (ICC) for the color coordinates (L*, a*, and b*) and for the color distances (ΔE) were calculated to determine interdevice reliability.
Results
It was shown both in the L*, a*, and b* color coordinates and in the calculated color differences ΔE different results with wide ranges, so L* color coordinates ranged from 49 to 78.7, a* coordinates from 3.6 to 31.2, b* coordinates from 8.6 to 45.6, and the calculated color differences ΔE for each device from 0.1 to 19.1. Table 2 shows the mean, standard deviations, minimum, and maximum values of L*, a*, and b* coordinates and calculated color differences ΔE for each color measurement device.
Only the L* coordinates and the ΔE values between the system A and C systems differed not significantly (p > 0.016)
Table 3 shows the intraclass correlation coefficients (ICC) for interdevice reliability for the L*, a*, and b* color coordinates and color distances ΔE for the devices tested. These ICC ranged from 0.675 to 0.807.
Discussion
Pink composite or ceramic restorations are a viable option for restoring Class V defects or perform optimal red esthetics with prosthetic restorations [8]. Even with challenging restorations, such as massive recession defects (Miller class II or above) or pigmentation of the marginal gingiva, composite restorations are an esthetic alternative to invasive surgical procedures for treating recession [6, 23]. However, visual evaluation of the shade of the gingiva has disadvantages because it is affected by light conditions (i.e., metamerism) or dyschromatopsia. Shade guides and electronic measurement systems are available for evaluating the shade of natural teeth. Several shade guides have been developed for different requirements, such as color matching in prosthetic restorations or detecting color changes during a bleaching process. However, only a few shade guide systems are available for evaluating the shade of gingival regions, and these are subject to coverage errors [9]. Ghinea et al. declared that there is no optimal gingival shade guide [24].
Therefore, a more objective and reproducible method for evaluating gingival color would be helpful. While electronic shade-taking systems are generally used for reproducible determination of tooth color [10, 13, 15, 16], these systems may also have the potential to evaluate gingival color reproducibly. The color coordinates of the gingiva vary widely and differ between females and males [25]. It is not clear whether tooth color measurement systems can record the strongly scattered color information of the marginal gingiva, especially because one of the systems tested (device ES) generates color information from reflected light. It is also not clear to what extent the thickness and type of gingiva, the region within the oral cavity [26], and the contact mode of the ES device affect color measurements. In fact and a strength of this study is that it was shown that the color measurement systems tested generated different color coordinates of gingival tissue that is shown by the low ICCs. In contrast to this, a limitation of this study is that no repositioning jig was used. Although such a jig was not used, which could have caused an extra variance of the results, this is not surprising because although dental color measuring systems have high reproducibility, they are not CIE-compliant. It was first demonstrated a difference between these systems and a CIE-compliant system in 2010 [15]. The SDs of the L*, a*, and b* color coordinates ranged from 1.6 to 5.7, and the calculated ΔE for each proband and measuring system also differed, as expected but first shown in this study. Several formulas are available for calculating ΔE [27] and the ΔE of each system has a SD visible to humans [19]. Therefore, the small differences in color of the gingival regions detected could also result from the measurement uncertainty of the systems. This is not surprising given that the instruments were designed for determining the shade of natural teeth, which have different color coordinates. Particularly, contact measurement systems, such as the ES system, could affect tissue perfusion during gingival color measurements, resulting in color changes that is a further limitation when interpreting the results. Therefore, soft tissue colors should be measured with non-contact systems. Considering the inherent uncertainties of gingiva measurements, the SP and CE systems showed the highest reliability for gingival color measurements of the devices tested. However, all these devices allow no high reproducible determination of color coordinates of the marginal gingiva.
Conclusion
The electronic tooth color determination systems evaluated herein are limited in terms of the reproducibility of evaluations of marginal gingival color. Furthermore, the results of the different measurement systems differ enormously; this should be considered in future clinical studies, whereas the systems SP and CE showed a higher reproducibility compared with the other two systems tested in this study. However, all systems tested in this study are not suitable for high reproducible determination of color coordinates of the marginal gingiva.
References
Khurana PR, Thomas PV, Rao SV, Balamuragan R, Singh MP (2009) A clinical study to correlate maxillary anterior natural teeth with that of the commercially available acrylic and porcelain shade guides. J Contemp Dent Pract 14(3):427–433
Tagtekin D, Yanikoglu F, Ozyoney G, Noyan N, Hayran O (2011) Clinical evaluation of a gingiva-coloured material, Comp Natur: a 3-year longitudinal study. Chin J Dent Res 14(1):59–66
Gallo JR, Burgess JO, Ripps AH, Walker RS, Ireland EJ, Mercante DE, Davidson JM (2005) Three-year clinical evaluation of a compomer and a resin composite as Class V filling materials. Oper Dent 30(3):275–281
Balkenhol M, Huang J, Wostmann B, Hannig M (2007) Influence of solvent type in experimental dentin primer on the marginal adaptation of Class V restorations. J Dent 35(11):836–844
Paravina RD, Westland S, Johnston WM, Powers JM (2008) Color adjustment potential of resin composites. J Dent Res 87(5):499–503
Pradeep K, Rajababu P, Satyanarayana D, Sagar V (2012) Gingival recession: review and strategies in treatment of recession. Case Rep Dent 2012:563421
Paryag A, Lowe J, Rafeek R (2017) Colored gingiva composite used for the rehabilitation of gingiva recessions and non-carious cervical lesions. Dentistry journal 5(4)
Paryag AA, Rafeek RN, Mankee MS, Lowe J (2016) Exploring the versatility of gingiva-colored composite. Clin Cosmet Investig Dent 8:63–69
Amer RS, Chandrasekaran I, Johnston WM (2016) Illuminant effect on the coverage error of a gingiva-colored composite resin shade guide. J Prosthet Dent 116(5):770–776
Khurana R, Tredwin CJ, Weisbloom M, Moles DR (2007) A clinical evaluation of the individual repeatability of three commercially available colour measuring devices. Br Dent J 203(12):675–680
Igiel C, Lehmann KM, Ghinea R, Weyhrauch M, Hangx Y, Scheller H, Paravina RD (2017) Reliability of visual and instrumental color matching. J Esthet Restor Dent 29(5):303–308
Igiel C, Weyhrauch M, Wentaschek S, Scheller H, Lehmann KM (2016) Dental color matching: a comparison between visual and instrumental methods. Dent Mater J 35(1):63–69
Lehmann KM, Devigus A, Igiel C, Wentaschek S, Azar MS, Scheller H (2011) Repeatability of color-measuring devices. Eur J Esthet Dent 6(4):428–435
Lehmann KM, Devigus A, Igiel C, Weyhrauch M, Schmidtmann I, Wentaschek S, Scheller H (2012) Are dental color measuring devices CIE compliant? Eur J Esthet Dent 7(3):324–333
Lehmann KM, Igiel C, Schmidtmann I, Scheller H (2010) Four color-measuring devices compared with a spectrophotometric reference system. J Dent 38(Suppl 2):e65–e70
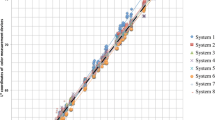
Weyhrauch M, Igiel C, Pabst AM, Wentaschek S, Scheller H, Lehmann KM (2015) Interdevice agreement of eight equivalent dental color measurement devices. Clin Oral Investig 19(9):2309–2318
Zenthofer A, Cabrera T, Corcodel N, Rammelsberg P, Hassel AJ (2014) Comparison of the easyshade compact and advance in vitro and in vivo. Clin Oral Investig 18(5):1473–1479
Hu X, Johnston WM, Seghi RR (2010) Measuring the color of maxillofacial prosthetic material. J Dent Res 89(12):1522–1527
Paravina RD, Ghinea R, Herrera LJ et al (2015) Color difference thresholds in dentistry. J Esthet Restor Dent 27(Suppl 1):1–9
Ragain JC Jr, Johnston WM (2001) Minimum color differences for discriminating mismatch between composite and tooth color. J Esthet Restor Dent 13(1):41–48
Happe A, Schulte-Mattler V, Fickl S, Naumann M, Zoller JE, Rothamel D (2013) Spectrophotometric assessment of peri-implant mucosa after restoration with zirconia abutments veneered with fluorescent ceramic: a controlled, retrospective clinical study. Clin Oral Implants Res 24(Suppl A100):28–33
Valente NA, Sailer I, Fehmer V, Thoma DS (2018) Color differences between pink veneering ceramics and the human gingiva. Int J Periodontics Restorative Dent 38(Suppl):s59–s65
Janiani P, Bhat PR, Trasad VA, Acharya AB, Thakur SL (2018) Evaluation of the intensity of gingival melanin pigmentation at different age groups in the Indian population: an observational study. J Indian Soc Pedod Prev Dent 36(4):329–333
Ghinea R, Herrera LJ, Perez MM, Ionescu AM, Paravina RD (2018) Gingival shade guides: colorimetric and spectral modeling. J Esthet Restor Dent 30(2):E31–E38
Gomez-Polo C, Montero J, Gomez-Polo M, Martin Casado AM (2018) Clinical study on natural gingival color. Odontology 107(1):80–89
Ganji KK, Alswilem RO, Abouonq AO, Alruwaili AA, Alam MK (2018) Noninvasive evaluation of the correlation between thickness of the buccal bone and attached gingiva of maxillary premolars. J Esthet Restor Dent 31(3):240–245
Gomez Polo C, Montero J, Martin Casado AM (2019) Comparison of two color-difference formulas using the Bland-Altman approach based on gingiva color space. Odontology 107(1):72–79
Funding
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author Henning Staedt declares that he has no conflict of interest. Author Eva Mally declares that she has no conflict of interest. Author Herbert Scheller declares that he has no conflict of interest. Author Peer W. Kämmerer declares that he has no conflict of interest. Author Adrian Kasaj declares that he has no conflict of interest. The author Alessandro Devigus declares that he has no conflict of interest. The author Karl Martin Lehmann declares that he has no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Human participants take part in this study during the preparation of restorative or prosthetic restorations.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Staedt, H., Mally, E., Scheller, H. et al. The reproducibility of electronic color measurements of the marginal gingiva. Clin Oral Invest 25, 145–150 (2021). https://doi.org/10.1007/s00784-020-03345-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-020-03345-x