Abstract
Objectives
This systematic review was undertaken to determine the oral health–related quality of life (OHRQoL) before and after endodontic treatment.
Materials and Methods
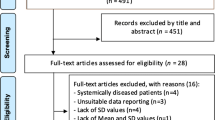
Based on the PRISMA guidelines, electronic databases (n = 7) were searched and from 1038 citations, 16 papers were included in this review. Information on study design, sample size, intervention/treatment modality, methods of assessing OHRQoL, and the key findings were extracted and analyzed.
Results
Among the 16 studies, 3 were cross-sectional surveys, 9 were longitudinal studies, and 4 were randomized clinical trials. The cross-sectional studies reported improvements in OHRQoL following root canal treatment. Comparative longitudinal studies did not identify a significant association between improvements in OHRQoL and the method of root canal instrumentation or number of instruments used. Clinical trials found that improvements in OHRQoL were significantly associated with instrumentation technique, surgical-incision approach, and the application of platelet-concentrate during surgery. Several methods of assessing OHRQoL were employed with the most common being the Oral Health Impact Profile (OHIP), albeit using different versions.
Conclusions
The results of this systematic review indicate that the QoL of patients improved after endodontic treatment. Nevertheless, these results are limited to patients who seek endodontic treatment and cannot be generalized. The lack of well-designed observational studies with standardized assessment approaches, coupled with heterogeneity of study design and interventions, precluded quantitative synthesis.
Clinical relevance
Pragmatic clinical trials are more meaningful to understand patient-centered outcomes of treatment. This review shows that endodontic treatment does improve the QoL. However, future studies should use standardized tools and data reporting, which are critical to make meta-analyses possible.

Similar content being viewed by others
References
Montero J, Lorenzo B, Barrios R, Albaladejo A, Miron Canelo JA, Lopez-Valverde A (2015) Patient-centered outcomes of root canal treatment: a cohort follow-up study. J Endod 41:1456–1461
Pak JG, White SN (2011) Pain prevalence and severity before, during, and after root canal treatment: a systematic review. J Endod 37:429–438
Dugas NN, Lawrence HP, Teplitsky P, Friedman S (2002) Quality of life and satisfaction outcomes of endodontic treatment. J Endod 28:819–827
Gatten DL, Riedy CA, Hong SK, Johnson JD, Cohenca N (2011) Quality of life of endodontically treated versus implant treated patients: a university-based qualitative research study. J Endod 37:903–909
Liu P, McGrath C, Cheung G (2014) Improvement in oral health-related quality of life after endodontic treatment: a prospective longitudinal study. J Endod 40:805–810
Haag DG, Peres KG, Balasubramanian M, Brennan DS (2017) Oral conditions and health-related quality of life: a systematic review. J Dent Res 96:864–874
Thalji G, McGraw K, Cooper LF (2016) Maxillary complete denture outcomes: a systematic review of patient-based outcomes. Int J Oral Maxillofac Implants 31(Suppl):s169–s181
Thomason JM, Kelly SA, Bendkowski A, Ellis JS (2012) Two implant retained overdentures--a review of the literature supporting the McGill and York consensus statements. J Dent 40:22–34
McGrath C, Lam O, Lang N (2012) An evidence-based review of patient-reported outcome measures in dental implant research among dentate subjects. J Clin Periodontol 39(Suppl 12):193–201
Shanbhag S, Dahiya M, Croucher R (2012) The impact of periodontal therapy on oral health-related quality of life in adults: a systematic review. J Clin Periodontol 39:725–735
Sox HC, Greenfield S (2009) Comparative effectiveness research: a report from the Institute of Medicine. Ann Intern Med 151:203–205
Hargreaves KM (2018) It is all in the eye of the beholder - what is the ideal clinical outcome study? AAE Annual Session 2018
Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K (2007) Outcome of primary root canal treatment: systematic review of the literature - part 1. Effects of study characteristics on probability of success. Int Endod J 40:921–939
Ng YL, Mann V, Rahbaran S, Lewsey J, Gulabivala K (2008) Outcome of primary root canal treatment: systematic review of the literature -- part 2. Influence of clinical factors. Int Endod J 41:6–31
Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S (2010) Outcome of endodontic surgery: a meta-analysis of the literature--part 1: comparison of traditional root-end surgery and endodontic microsurgery. J Endod 36:1757–1765
Tsesis I, Rosen E, Taschieri S, Telishevsky Strauss Y, Ceresoli V, Del Fabbro M (2013) Outcomes of surgical endodontic treatment performed by a modern technique: an updated meta-analysis of the literature. J Endod 39:332–339
Fleming PS, Koletsi D, O’Brien K, Tsichlaki A, Pandis N (2016) Are dental researchers asking patient-important questions? A scoping review. J Dent 49:9–13
Reisine ST, Fertig J, Weber J, Leder S (1989) Impact of dental conditions on patients’ quality of life. Community Dent Oral Epidemiol 17:7–10
Allen PF (2003) Assessment of oral health related quality of life. Health Qual Life Outcomes 1:40
Vena DA, Collie D, Wu H, Gibbs JL, Broder HL, Curro FA et al (2014) Prevalence of persistent pain 3 to 5 years post primary root canal therapy and its impact on oral health-related quality of life: PEARL Network findings. J Endod 40:1917–1921
Hamasha AA, Hatiwsh A (2013) Quality of life and satisfaction of patients after nonsurgical primary root canal treatment provided by undergraduate students, graduate students and endodontic specialists. Int Endod J 46:1131–1139
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S (2014) PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14:579
Del Fabbro M, Taschieri S, Testori T, Francetti L, Weinstein RL (2007) Surgical versus non-surgical endodontic re-treatment for periradicular lesions. Cochrane Database Syst Rev CD005511
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62:1006–1012
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al (2011) The Newcastle–Ottawa Scale (NOS) for assessing the quality of non-randomized studies in meta-analysis. Available from http://www.ohri.Ca/programs/clinical_epidemiology/oxford.asp
Yu VS, Messer HH, Yee R, Shen L (2012) Incidence and impact of painful exacerbations in a cohort with post-treatment persistent endodontic lesions. J Endod 38:41–46
Liu P, McGrath C, Cheung G (2014) What are the key endodontic factors associated with oral health-related quality of life? Int Endod J 47:238–245
Jordan RA, Markovic L, Holzner AL, Richter B, Gaengler P (2009) Development of a basic root canal treatment (BRT) for primary oral health care--evaluation after one year. Int Dent J 59:141–147
Wright WG, Jones JA, Spiro A 3rd, Rich SE, Kressin NR (2009) Use of patient self-report oral health outcome measures in assessment of dental treatment outcomes. J Public Health Dent 69:95–103
Bartols A, Reutter CA, Robra BP, Walther W (2016) Reciproc vs. hand instrumentation in dental practice: a study in routine care. PeerJ 4:e2182
Bartols A, Laux G, Walther W (2016) Multiple-file vs. single-file endodontics in dental practice: a study in routine care. PeerJ 4:e2765
Pasqualini D, Corbella S, Alovisi M, Taschieri S, Del Fabbro M, Migliaretti G et al (2016) Postoperative quality of life following single-visit root canal treatment performed by rotary or reciprocating instrumentation: a randomized clinical trial. Int Endod J 49:1030–1039
Yaylali IE, Teke A, Tunca YM (2017) The effect of foraminal enlargement of necrotic teeth with a continuous rotary system on postoperative pain: a randomized controlled trial. J Endod 43:359–363
He J, White RK, White CA, Schweitzer JL, Woodmansey KF (2017) Clinical and patient-centered outcomes of nonsurgical root canal retreatment in first molars using contemporary techniques. J Endod 43:231–237
Tsesis I, Shoshani Y, Givol N, Yahalom R, Fuss Z, Taicheri S (2005) Comparison of quality of life after surgical endodontic treatment using two techniques: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99:367–371
Del Fabbro M, Taschieri S, Weinstein R (2009) Quality of life after microscopic periradicular surgery using two different incision techniques: a randomized clinical study. Int Endod J 42:360–367
Del Fabbro M, Ceresoli V, Lolato A, Taschieri S (2012) Effect of platelet concentrate on quality of life after periradicular surgery: a randomized clinical study. J Endod 38:733–739
Duncan HF, Galler KM, Tomson PL, Simon S, El-Karim I, Kundzina R, Krastl G, Dammaschke T, Fransson H, Markvart M, Zehnder M, Bjørndal L (2019) European Society of Endodontology position statement: management of deep caries and the exposed pulp. Int Endod J 52:923–934
Bjørndal L, Simon S, Tomson PL, Duncan HF (2019) Management of deep caries and the exposed pulp. Int Endod J 52:949–973
Antunes LS, Souza CR, Salles AG, Gomes CC, Antunes LA (2018) Does conventional endodontic treatment impact oral health-related quality of life? A systematic review. Eur Endod J 3:2–8
Masood M, Masood Y, Saub R, Newton JT (2014) Need of minimal important difference for oral health-related quality of life measures. J Public Health Dent 74:13–20
Hollister MC, Weintraub JA (1993) The association of oral status with systemic health, quality of life, and economic productivity. J Dent Educ 57:901–912
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41:582–592
Iqbal MK, Kratchman SI, Guess GM, Karabucak B, Kim S (2007) Microscopic periradicular surgery: perioperative predictors for postoperative clinical outcomes and quality of life assessment. J Endod 33:239–244
Liu P, McGrath C, Cheung GS (2012) Quality of life and psychological well-being among endodontic patients: a case-control study. Aust Endod J 57:493–497
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, ethical approval is not required.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary data 1
PRISMA checklist for selection process of articles (DOC 59 kb)
Appendix 1
Appendix 1
Assessment of risk of bias for cross-sectional and longitudinal studies included in this review
The following criteria (Newcastle-Ottawa scale) was used to score each study that was included in this review.
A maximum of two stars (**) is awarded for item 1.
A maximum of one star (*) is awarded for items 2 and 3.
A maximum of five stars (*****) is awarded for the items “Outcomes measurement.”
-
1.
Representativeness of sample (max. 2*)
Evaluated by the sample generation methods and sample origin (e.g., community, specific population)
-
a)
Random sample of specific population groups*
-
b)
Random sample of individuals of a population (or community)**
-
c)
Non-random sample of specific population groups
-
d)
Non-random sample of individuals of a population (or community)
-
e)
No description of whether sample was random or not
-
a)
-
2.
Comparability (max. 1*)
Evaluated by the presence of control group
-
a)
Presence of control group (without endodontic treatment)
-
b)
Absence of control group
-
a)
-
3.
Calibration for exposure (max. 1*)
-
a)
Calibrated examiner: *Description of training/calibration procedure
-
b)
Non-calibrated examiner: report of absence of calibration; report of calibration, but with no description of procedure; no report of whether calibration was performed
-
a)
-
4.
Outcome measurement (max. 5*) including outcome assessment tool; concealment; adjustment of confounding factors; and non-response rate
Assessment tool for outcome (In this review, the outcome was impact of endodontic treatment on quality of life).
-
a)
Use of validated assessment tool*
-
b)
Use of non-validated assessment tool or databank records (secondary data)
-
a)
Concealment for evaluation of outcome (In this review, the examiner was considered to be blinded to exposure (received or not received endo-treatment) when evaluating the outcome (quality of life)).
-
5.
Adjustments for confounding factors
-
a)
Adjustment for confounder of outcome*
-
b)
Adjustment for second confounder of outcome**
-
a)
-
6.
Non-response rate
-
a)
Description of non-response rate*
-
b)
No description of non-response rate
-
a)
Although references [32, 33, 36, 37] were performed with control groups for comparison of two treatments, we evaluated them using this risk of bias tool due to the absence of a negative control group (no endodontic treatment). Albeit this being an issue of ethical concern, this strategy was adopted to fit to the research question in this paper.
Rights and permissions
About this article
Cite this article
Neelakantan, P., Liu, P., Dummer, P.M.H. et al. Oral health–related quality of life (OHRQoL) before and after endodontic treatment: a systematic review. Clin Oral Invest 24, 25–36 (2020). https://doi.org/10.1007/s00784-019-03076-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-03076-8