Abstract
Objectives
The present study evaluated the degradation of collagen matrix (CM) immersed in tetracycline (TTC) or phosphate-buffered saline (PBS) in diabetic and normoglycemic rats.
Materials and methods
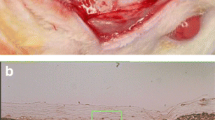
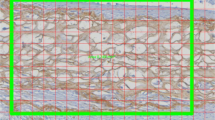
Diabetes was induced in 15 rats by systemic streptozotocin (STZ) (experimental); 15 healthy rats served as controls. One day before implantation 60 CM disks, 5 mm in diameter, were labeled with biotin: 30 were immersed in tetracycline (TTC) and 30 in PBS. One disk of each type was implanted subdermally in each rat. Animals were euthanized after 3 weeks, and tissue specimens containing the disks were prepared for histologic analysis. Horseradish peroxidase (HRP)-conjugated streptavidin was used to detect the remaining biotinylated collagen. Residual collagen area within the CM disks was analyzed and compared to baseline.
Results
Diabetes significantly increased the CM degradation. Immersion of the CM disks in a 50-mg/mL TTC solution before implantation decreased its degradation both in diabetic and normoglycemic rats.
Conclusions
Diabetes significantly increases collagen matrix degradation; immersion of collagen matrix in TTC before implantation decreases its degradation in both diabetic and normoglycemic conditions.
Clinical relevance
Immersion of medical collagen devices in TTC may be an effective means to decrease their resorption rate and increase their effectiveness, especially in situations with increased degradation such as diabetes.




Similar content being viewed by others
References
Chiapasco M, Zaniboni M, Boisco M (2006) Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res 17(Suppl 2):136–159
Pfeifer J, Van Swol RL, Ellinger R (1989) Epithelial exclusion and tissue regeneration using a collagen membrane barrier in chronic periodontal defects: a histologic study. Int J Periodontics Restorative Dent 9:262–273
Tal H, Kozlovsky A, Artzi Z, Nemcovsky CE, Moses O (2008) Cross-linked and non-cross-linked collagen barrier membranes disintegrate following surgical exposure to the oral environment: a histological study in the cat. Clin Oral Implants Res 19:760–766
Tal H, Kozlovsky A, Artzi Z, Nemcovsky CE, Moses O (2008) Long-term bio-degradation of cross-linked and noncross-linked collagen barriers in human guided bone regeneration. Clin Oral Implants Res 19:295–302
Singh MP, Stefko J, Lumpkin JA, Rosemblatt J (1995) The effect of electrostatic charge interactions on release rates of gentamicin from collagen matrices. Pharmacol Res 12:1205–1210
Freiss W (1998) Collagen—biomaterial for drug delivery. Eur J Pharm Biopharm 45:113–136
Goissis G, Marcantônio E Jr, Marcantônio RA, Lia RC, Cancian DC, de Carvalho WM (1999) Biocompatibility studies of anionic collagen membranes with different degree of glutaraldehyde cross-linking. Biomaterials 20:27–34
Tanaka S, Avigad G, Eikenberry EF, Brodsky B (1988) Isolation and partial characterization of collagen chains dimerized by sugar-derived cross-links. J Biol Chem 263:17650–17657
Hämmerle CH, Jung RE, Feloutzis A (2002) A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. J Clin Periodontol 29(Suppl 3):226–231
Wallace SS, Froum SJ (2003) Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol 8:328–343
McGuire MK, Scheyer ET (2010) Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence-type recession defects. J Periodontol 81:1108–1117
Nevins M, Nevins ML, Kim SW, Schupbach P, Kim DM (2011) The use of mucograft collagen matrix to augment the zone of keratinized tissue around teeth: a pilot study. Int J Periodontics Restorative Dent 31:367–367
Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M (2009) Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 36:868–876
Lorenzo R, Garcia V, Orsini M, Martin C, Sanz M (2012) Clinical efficacy of a xenogeneic collagen matrix in augmenting keratinized mucosa around implants: a randomized controlled prospective clinical trial. Clin Oral Implants Res 23:316–324
Camelo M, Nevins M, Nevins ML, Schupbach P, Kim DM (2012) Treatment of gingival recession defects with xenogenic collagen matrix: a histologic report. Int J Periodontics Restorative Dent 32:167–173
Herford AS, Akin L, Cicciu M, Maiorana C, Boyne PJ (2010) Use of a porcine collagen matrix as an alternative to autogenous tissue for grafting oral soft tissue defects. J Oral Maxillofac Surg 68:1463–1470
Abraham LC, Dice JF, Lee K, Kaplan DL (2007) Phagocytosis and remodeling of collagen matrices. Exp Cell Res 313:1045–1055
Reynolds JJ, Hembry RM, Meikle MC (1994) Connective tissue degradation in health and periodontal disease and the roles of matrix metalloproteinases and their natural inhibitors. Adv Dent Res 8:312–319
Armstrong DG, Jude EB (2002) The role of matrix metalloproteinases in wound healing. J Am Podiatr Med Assoc 92:12–18
Minabe M, Kodama T, Kogou T et al (1989) Different cross-linked types of collagen implanted in rat palatal gingiva. J Periodontol 60:35–43
DeLustro F, Condell RA, Nguyen MA, McPherson JM (1986) A comparative study of the biologic and immunologic response to medical devices derived from dermal collagen. J Biomed Mater Res 20:109–120
Hämmerle CH, Jung RE (2003) Bone augmentation by means of barrier membranes. Periodontol 33:36–53, 2000
Moses O, Nemcovsky CE, Tal H, Zohar R (2001) Tetracycline modulates collagen membrane degradation in vitro. J Periodontol 72:1588–1593
Zohar R, Nemcovsky CE, Kebudi E, Artzi Z, Tal H, Moses O (2004) Tetracycline impregnation delays collagen membrane degradation in vivo. J Periodontol 75:1096–1101
Moses O, Vitiral D, Aboody G et al (2008) Bio-degradation of three different collagen membranes in the rat calvaria: a comparative study. J Periodontol 79:905–911
Moses O, Shemesh A, Aboody G, Tal H, Weinreb M, Nemcovsky CE (2009) Systemic TTC delays degradation of three different collagen membranes in rat calvaria. Clin Oral Implants Res 20:189–195
Pacios S, Kang J, Galicia J et al (2012) Diabetes aggravates periodontitis by limiting repair through enhanced inflammation. FASEB J 26:1423–1430
Graves DT, Kayal RA (2008) Diabetic complications and dysregulated innate immunity. Front Biosci 13:1227–1239
Xu F, Zhang C, Graves DT (2013) Abnormal cell responses and role of TNF-α in impaired diabetic wound healing. Biomed Res Int 2013, 754802. doi:10.1155/2013/754802
Thrailkill KM, Clay Bunn R, Fowlkes JL (2009) Matrix metalloproteinases: their potential role in the pathogenesis of diabetic nephropathy. Endocrine 35:1–10
Eliezer M, Nemcovsky CE, Romanos G et al (2013) Opposing effects of diabetes and tetracycline on the degradation of collagen membranes in rats. J Periodontol 84:529–534
Hartner A, Veelken R, Wittmann M, Cordasic N, Hilgers KF (2005) Effects of diabetes and hypertension on macrophage infiltration and matrix expansion in the rat kidney. BMC Nephrol 27(6):6
Fornoni A, Ijaz A, Tejada T, Lenz O (2008) Role of inflammation in diabetic nephropathy. Curr Diabetes Rev 4:10–17, Review
Acknowledgments
This study was supported by the Gerald A Niznick Chair of Implantology at Tel Aviv University, Israel. Mucograft® was donated by Geistlich Pharma AG Wolhusen, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by Institutional Animal Care and Use Committee of the Tel Aviv University.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
In partial fulfillment for the degree of D.M.D. of Asaf Shely from the Maurice and Gabriela Goldschleger School of Dental Medicine, Tel Aviv University, Tel Aviv, Israel.
Rights and permissions
About this article
Cite this article
Tal, H., Weinreb, M., Shely, A. et al. Tetracycline impregnation affects degradation of porcine collagen matrix in healthy and diabetic rats. Clin Oral Invest 20, 1237–1242 (2016). https://doi.org/10.1007/s00784-015-1615-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1615-0