Abstract
Objectives
This study aims to assess the potential of a mixture of three antibiotics (TreVitaMix, TVM) as an intracanal dressing to disinfect the outer root surface by applying a new in vitro model.
Materials and methods
Fifty freshly extracted bovine roots were endodontically treated. Forty samples were then thoroughly scaled, mounted to petri dishes, gas sterilized, and randomly allocated to four groups (n = 10/group) according to their intracanal medication: sterile saline (NaCl; control, A); the TVM carrier material alone, i.e., propylene glycol (PG; B); TVM (C); and calcium hydroxide (D). In an additional group (E), the cementum was not removed and TVM was placed. Petri dishes were filled with Fastidious Anaerobe Agar, inoculated with Fusobacterium nucleatum suspension and then anaerobically incubated during 48-h intervals at 37 °C up to 192 h. Inhibition zones around the roots were then measured after each incubation period (mm2).
Results
Only teeth inoculated with the TVM dressing showed inhibition at all time points, whereas the other treatments showed no peri-radicular growing inhibition. Presence of cementum had no negative effect on disinfection (p = 0.9320).
Conclusion
TVM was able to penetrate through the dentine and inhibit the bacterial growth of F. nucleatum up to 192 h.
Clinical relevance
TVM might have the potential to sustainably disinfect the outer root surface in perio-endo lesions and serve as an adjunctive antimicrobial agent.



Similar content being viewed by others
References
Trope M, Tronstad L, Rosenberg ES, Listgarten M (1988) Darkfield microscopy as a diagnostic aid in differentiating exudates from endodontic and periodontal abscesses. J Endod 14:35–38
Kobayashi T, Hayashi A, Yoshikawa R, Okuda K, Hara K (1990) The microbial flora from root canals and periodontal pockets of non-vital teeth associated with advanced periodontitis. Int Endod J 23:100–106
Trope M, Rosenberg E, Tronstad L (1992) Darkfield microscopic spirochete count in the differentiation of endodontic and periodontal abscesses. J Endod 18:82–86
Kurihara H, Kobayashi Y, Francisco IA, Isoshima O, Nagai A, Murayama Y (1995) A microbiological and immunological study of endodontic-periodontic lesions. J Endod 21:617–621
Dongari A, Lambrianidis T (1988) Periodontally derived pulpal lesions. Endod Dent Traumatol 4:49–54
Kipioti A, Nakou M, Legakis N, Mitsis F (1984) Microbiological findings of infected root canals and adjacent periodontal pockets in teeth with advanced periodontitis. Oral Surg Oral Med Oral Pathol 58:213–220
Kerekes K, Olsen I (1990) Similarities in the microfloras of root canals and deep periodontal pockets. Endod Dent Traumatol 6:1–5
Didilescu AC, Rusu D, Anghel A, Nica L, Iliescu A, Greabu M et al (2012) Investigation of six selected bacterial species in endo-periodontal lesions. Int Endod J 45:282–293
Langeland K, Rodrigues H, Dowden W (1974) Periodontal disease, bacteria, and pulpal histopathology. Oral Surg Oral Med Oral Pathol 37:257–270
Bergenholtz G, Lindhe J (1978) Effect of experimentally induced marginal periodontitis and periodontal scaling on the dental pulp. J Clin Periodontol 5:59–73
Oosterwaal PJ, Mikx FH, Renggli HH (1990) Clearance of a topically applied fluorescein gel from periodontal pockets. J Clin Periodontol 17:613–615
Mohammadi Z, Abbott PV (2009) Antimicrobial substantivity of root canal irrigants and medicaments: a review. Aust Endod J 35:131–139
Siqueira JFJ, Lopes HP (1999) Mechanisms of antimicrobial activity of calcium hydroxide: a critical review. Int Endod J 32:361–369
Orstavik D (2003) Root canal disinfection: a review of concepts and recent developments. Aust Endod J 29:70–74
Athanassiadis B, Abbott PV, Walsh LJ (2007) The use of calcium hydroxide, antibiotics and biocides as antimicrobial medicaments in endodontics. Aust Dent J 52:S64–S82
Nerwich A, Figdor D, Messer HH (1993) pH changes in root dentin over a 4-week period following root canal dressing with calcium hydroxide. J Endod 19:302–306
Hoshino E, Kurihara-Ando N, Sato I, Uematsu H, Sato M, Kota K et al (1996) In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J 29:125–130
Sato I, Ando-Kurihara N, Kota K, Iwaku M, Hoshino E (1996) Sterilization of infected root-canal dentine by topical application of a mixture of ciprofloxacin, metronidazole and minocycline in situ. Int Endod J 29:118–124
Csukas Z, Ferenczi I, Nasz I, Banoczy J (1987) Diffusion of metronidazole through the dentinal tubules of extracted teeth. Acta Microbiol Hung 34:121–124
Thibodeau B, Trope M (2007) Pulp revascularization of a necrotic infected immature permanent tooth: case report and review of the literature. Pediatr Dent 29:47–50
Kim JH, Kim Y, Shin SJ, Park JW, Jung IY (2010) Tooth discoloration of immature permanent incisor associated with triple antibiotic therapy: a case report. J Endod 36:1086–1091
Trope M (2010) Treatment of the immature tooth with a non-vital pulp and apical periodontitis. Dent Clin North Am 54:313–324
Wang X, Thibodeau B, Trope M, Lin LM, Huang GT (2010) Histologic characterization of regenerated tissues in canal space after the revitalization/revascularization procedure of immature dog teeth with apical periodontitis. J Endod 36:56–63
Bezgin T, Yilmaz AD, Celik BN, Sonmez H (2014) Concentrated platelet-rich plasma used in root canal revascularization: 2 case reports. Int Endod J 47:41–49
Chen X, Bao ZF, Liu Y, Liu M, Jin XQ, Xu XB (2013) Regenerative endodontic treatment of an immature permanent tooth at an early stage of root development: a case report. J Endod 39:719–722
Tawfik H, Abu-Seida AM, Hashem AA, Nagy MM (2013) Regenerative potential following revascularization of immature permanent teeth with necrotic pulps. Int Endod J 46:910–922
Bystrom A, Sundqvist G (1985) The antibacterial action of sodium hypochlorite and EDTA in 60 cases of endodontic therapy. Int Endod J 18:35–40
Gmur R, Guggenheim B (1983) Antigenic heterogeneity of Bacteroides intermedius as recognized by monoclonal antibodies. Infect Immun 42:459–470
Yassen GH, Platt JA, Hara AT (2011) Bovine teeth as substitute for human teeth in dental research: a review of literature. J Oral Sci 53:273–282
Titley KC, Torneck CD, Smith DC, Adibfar A (1988) Adhesion of composite resin to bleached and unbleached bovine enamel. J Dent Res 67:1523–1528
Arends J, Christoffersen J, Ruben J, Jongebloed WL (1989) Remineralization of bovine dentine in vitro. The influence of the F content in solution on mineral distribution. Caries Res 23:309–314
Retief DH, Mandras RS, Russell CM, Denys FR (1990) Extracted human versus bovine teeth in laboratory studies. Am J Dent 3:253–258
Reeves GW, Fitchie JG, Hembree JHJ, Puckett AD (1995) Microleakage of new dentin bonding systems using human and bovine teeth. Oper Dent 20:230–235
Vasiliadis L, Darling AI, Levers BG (1983) The histology of sclerotic human root dentine. Arch Oral Biol 28:693–700
Paque F, Luder HU, Sener B, Zehnder M (2006) Tubular sclerosis rather than the smear layer impedes dye penetration into the dentine of endodontically instrumented root canals. Int Endod J 39:18–25
Cruz EV, Kota K, Huque J, Iwaku M, Hoshino E (2002) Penetration of propylene glycol into dentine. Int Endod J 35:330–336
Gomes BP, Montagner F, Berber VB, Zaia AA, Ferraz CC, de Almeida JF et al (2009) Antimicrobial action of intracanal medicaments on the external root surface. J Dent 37:76–81
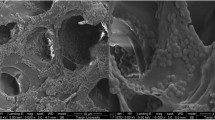
Martins Junior W, De Rossi A, Samih Georges Abi Rached R, Rossi MA (2011) A scanning electron microscopy study of diseased root surfaces conditioned with EDTA gel plus Cetavlon after scaling and root planing. J Electron Microsc (Tokyo) 60:167–175
Gamal AY, Mailhot JM (2003) The effects of EDTA gel conditioning exposure time on periodontitis-affected human root surfaces: surface topography and PDL cell adhesion. J Int Acad Periodontol 5:11–22
Prasad SS, Radharani C, Varma S, Kumar SV, Sinha S, Bijle MN (2012) Effects of citric acid and EDTA on periodontally involved root surfaces: a SEM study. J Contemp Dent Pract 13:446–451
Mittal M, Vashisth P, Chaubey KK, Dwivedi S, Arora S (2014) Comparative evaluation of root surface morphology after planing and root conditioning with tetracycline hydrochloride—an in vitro SEM study. J Tenn Dent Assoc 94:21–26, quiz 26–7
de Sanctis M, Clementini M (2014) Flap approaches in plastic periodontal and implant surgery: critical elements in design and execution. J Clin Periodontol 41(Suppl 15):S108–S122
Hattler AB, Listgarten MA (1984) Pulpal response to root planing in a rat model. J Endod 10:471–476
Kerns DG, Scheidt MJ, Pashley DH, Horner JA, Strong SL, Van Dyke TE (1991) Dentinal tubule occlusion and root hypersensitivity. J Periodontol 62:421–428
Kolenbrander PE, Palmer RJJ, Periasamy S, Jakubovics NS (2010) Oral multispecies biofilm development and the key role of cell-cell distance. Nat Rev Microbiol 8:471–480
Rams TE, Degener JE, van Winkelhoff AJ (2014) Antibiotic resistance in human chronic periodontitis microbiota. J Periodontol 85:160–169
Rams TE, Feik D, Mortensen JE, Degener JE, van Winkelhoff AJ (2013) Antibiotic susceptibility of periodontal Enterococcus faecalis. J Periodontol 84:1026–1033
Veloo AC, Seme K, Raangs E, Rurenga P, Singadji Z, Wekema-Mulder G et al (2012) Antibiotic susceptibility profiles of oral pathogens. Int J Antimicrob Agents 40:450–454
Al-Ahmad A, Ameen H, Pelz K, Karygianni L, Wittmer A, Anderson AC et al (2014) Antibiotic resistance and capacity for biofilm formation of different bacteria isolated from endodontic infections associated with root-filled teeth. J Endod 40:223–230
Olsen I (2015) Biofilm-specific antibiotic tolerance and resistance. Eur J Clin Microbiol Infect Dis 34:877–886
Herrera D, Alonso B, Leon R, Roldan S, Sanz M (2008) Antimicrobial therapy in periodontitis: the use of systemic antimicrobials against the subgingival biofilm. J Clin Periodontol 35:45–66
Jhajharia K, Parolia A, Shetty KV, Mehta LK (2015) Biofilm in endodontics: a review. J Int Soc Prev Community Dent 5:1–12
Rabbani GM, Ash MMJ, Caffesse RG (1981) The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol 52:119–123
Windley W, Teixeira F, Levin L, Sigurdsson A, Trope M (2005) Disinfection of immature teeth with a triple antibiotic paste. J Endod 31:439–443
Ahmed HM, Abbott PV (2012) Discolouration potential of endodontic procedures and materials: a review. Int Endod J 45:883–897
Acknowledgments
We would like to thank Beatrice Sener and Andreas Meier for their help in the microbiology laboratory.
Conflict of interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Zaruba, M., Rechenberg, DK., Thurnheer, T. et al. Endodontic drug delivery for root surface disinfection: a laboratory feasibility evaluation. Clin Oral Invest 20, 607–613 (2016). https://doi.org/10.1007/s00784-015-1538-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1538-9