Abstract
Background
Smear layer removal has been shown to reduce bacterial penetration through root canal obturations when resin-based endodontic sealer is used. The purpose of this in vitro study was to test this effect when a non-resin-based sealer is used.
Material and methods
Thirty root segments were assigned to the following groups: Smear layer removed (n = 8); smear layer retained (n = 8); negative controls (n = 10; 5 with smear layer, 5 without); and positive controls (n = 4; 2 with smear layer, 2 without). After rotary instrumentation, smear layers were removed in the treatment group and half of controls using 17% ethylenediamenetetraacetic acid (EDTA) prior to obturation. Each obturated root was affixed into a dual-chamber leakage model employing Streptococcus mutans. Roots were incubated at 37 °C for 120 d. Days until lower chamber turbidity occurred was recorded for each sample, and data were analyzed using Kaplan-Meier survival curve analysis (p = 0.05).
Results
No negative controls leaked, while all positive controls were turbid within 1 day. Mean days to leakage for roots with smear layer intact was 82.75 (+/− 33.29, 95% CI), although three never leaked. Mean days to leakage through roots with smear layer removed was 46.25 (+/− 26.67, 95% CI), and all leaked. Treatment survival curves were significantly different (p = 0.048).
Conclusions
Under the conditions and limitations of this study, retaining the smear layer reduced the rate of bacterial penetration through canals which had been obturated using zinc oxide eugenol (ZOE) -based sealer.
Similar content being viewed by others
Background
During endodontic instrumentation, dentin is cut which leaves behind a layer of microscopic debris on its surface. This is known as the smear layer, and it has been characterized as a collection of micro-particles of mineralized collagen matrix. Whether this layer should be removed prior to endodontic obturation has been controversial [1].
Studies in support of smear layer removal suggest that it may contribute to better disinfection [2] and enhanced sealability [3, 4] of the canal system. It is thought that, since the smear layer can contain bacteria, and because it might potentially slough later, it should be removed. Thus, the clinical consensus has been to remove it prior to endodontic obturation.
Alternatively, it has been suggested that an intact smear layer may block bacterial penetration into the dentinal tubules. Smear layer plugs in dentinal tubules are thought to reduce the permeability of dentin, enhancing the overall sealability of the canal system by obturation [5]. These plugs have also been observed to delay the effects of intracanal medicaments [6]. Moreover, recent clinical outcome (i.e. success rate of endodontic treatment) data have not fully supported the practice of smear layer removal [7]. As a result, some clinicians continue to question whether the smear layer should be removed or left intact.
The effect of the smear layer upon treatment success may be dependent upon the type of endodontic sealer that is used. Leaving the smear layer intact resulted in reduced bacterial penetration in vitro when calcium hydroxide-based sealer was used [8]. In a similar study, the opposite was observed [9], but only polymeric resin-based sealer AH 26™ (Dentsply Caulk, Milford, DE., U.S.A.) was used. Contemporary clinical endodontic practice has long employed ZOE-based sealers with success. In terms of biocompatibility and clinical outcomes, the efficacy of ZOE-based sealers has been well demonstrated [10, 11]. Because the effect of the smear layer may be dependent upon sealer type, and ZOE-based sealers are still widely used, our purpose herein was to examine the significance of the smear layer specifically when ZOE-based sealers are used. The null hypothesis for this in vitro study was that smear layer removal, prior to endodontic obturation using ZOE-based sealer, does not affect bacterial leakage through and beside coronally-exposed gutta-percha obturations.
Methods
Thirty caries- and restoration-free single-rooted human teeth that had been extracted for unrelated reasons, usually orthodontic, were collected from a private oral surgery clinic. All clinical protocol, including the use of discarded teeth without individual patient consent, was approved by the Institutional Review Board of Saint Leo University, Saint Leo, FL., according to regulations instituted by the U.S. Department of Health and Human Services [12]. Teeth were decoronated to standardize length of root segments to 17 mm, with apices intact and unaltered. No roots with severe apical curvatures or dilacerations were included. Individual root segments were prepared and obturated using conventional endodontic protocol consistent with that described by Monticelli et al. [13], except that apical foramina were trephinated to three file sizes higher than that which initially gave resistance at the apical constriction. This resulted in different master apical file sizes for different samples, with the aim of reducing experimental variability due to varying apical anatomy. ZOE-based Tubli-Seal™ (Sybron Endo Inc., manufactured by Kerr Italia, Scafati, Italy) was used as sealer in all samples. After canal instrumentation, and prior to obturation, smear layers of 16 teeth were removed by rinsing the prepared canal systems with 10 ml of 17% EDTA (Inter-Med, Racine, WI., U.S.A.) according to Pashley et al. [5]. Obturated root segments were stored in humid conditions at 37 °C for 7 d to allow the sealer to set.
Obturated root segments were randomly and blindly assigned into the following groups:
8 with smear layer removed
8 with smear layer intact
5 negative controls with smear layer removed
5 negative controls with smear layer intact
2 positive controls with smear layer removed
2 positive controls with smear layer intact
Coronal orifices of negative control teeth were filled with a depth of at least 2 mm of Intermediate Restorative Material (IRM®, Dentsply Sirona Inc., manufactured by Dentsply Caulk Inc., Milford, DE., U.S.A.), and their apical foramina were covered by two layers of nail enamel (Revlon®, New York, NY., U.S.A.). Positive control teeth were instrumented and prepared for obturation, one with smear layer removed, but left unobturated and unfilled.
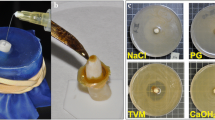
A split, or dual, chamber leakage model system for each root segment (Fig. 1) was similar to the design from previous studies [4, 5, 13], with the following minor adaptations: Two layers of nail enamel were used instead of sticky wax; and the upper chamber was achieved using a modified, disposable plastic 3 mL graduated transfer pipette (Karter Scientific, Lake Charles, LA., U.S.A.). The upper chamber was formed by stretching the cut plastic pipette tightly over the coronal end of the root segment. The junction between pipette plastic and the outer surface of the root was covered with two layers of nail enamel to within 3 mm of the apical foramen. This upper chamber apparatus was disinfected by soaking in 3.0% NaOCl (Kerr Inc., Orange, CA., U.S.A.) for 10 min followed by thorough flush with sterile de-ionized water, based upon evidence that NaOCl effectively removes endodontic biofilms [14]. For each sample, the upper chamber apparatus was then lowered into a 100 mL glass test tube (Karter Scientific, Lake Charles, LA., U.S.A.) containing clear bovine brain heart infusion (BD Bacto™, BD Biosciences, San Jose, CA., U.S.A.) to a level that inundated the peripex and the outer, varnish-coated surface of the root. The upper chamber apparati were affixed in place, and the lower chambers sealed from the environment, using Parafilm M® (Bemis, Neenah, WI., U.S.A.). The opening at the top of the upper chamber, through which weekly bacterial re-inoculations were made, was also covered with Parafilm M. All dual-chamber leakage models were assembled, as above, under a fume hood.
All bacteriologic methods were carried out as described by Monticelli et al. [13] employing Streptococcus mutans, a gram-positive facultative anaerobe. On day 0 of the experiment, the upper chambers of each sample were half-filled with Strep. mutans suspensions and sealed with Parafilm over the opening. Model systems were incubated at 37 °C and were re-inoculated weekly for the duration of the experiment. Lower chambers were examined daily for turbidity. Number of days until lower chamber turbidity occurred was recorded for each sample. Turbidity of a lower chamber was taken to indicate leakage of Strep. mutans through or around the obturation in a root segment (Fig. 2). 95% confidence intervals were calculated for mean number of days to leakage for each treatment; and survival curves for each treatment were generated and analyzed using the Kaplan-Meier Log Rank test (p = 0.05) on SigmaPlot 14.0 (Systat Software, San Jose, CA., U.S.A.). Since the data was nonparametric, medians were included as well.
Results
All results are listed in Table 1. All positive controls showed turbidity in the lower chambers within 1 day. None of the negative controls leaked for the entire 120 d experimental period. Mean number of days to leakage through roots with smear layer intact was 82.75, with 95% CI (49.47, 116.04) for a sample size of 8. Median number of days to leakage, with smear layer intact, was 78.0. Mean number of days to leakage through roots with smear layer removed was 46.25, with 95% CI (19.59, 72.92) for a sample size of 8. Median number of days to leakage, with smear layer removed, was 24.0. Based upon Kaplan-Meier Log Rank analysis, the survival curve for roots with smear layer intact was significantly longer than for roots with smear layer removed (p = 0.048; Fig. 3). Three of the 8 roots with smear layer intact did not leak for the entire experimental period, while all roots with smear layer removed leaked during the experimental period.
Discussion
The results of this in vitro study support rejection of our null hypothesis that removal of the smear layer, prior to endodontic obturation using ZOE-based sealer, would not affect bacterial leakage through or beside coronally-exposed root canal obturations. Under the conditions and limitations of this study, retaining the smear layer appeared to weakly reduce bacterial leakage. This contrasts with the findings of Clark-Holke et al. [9], who used resin-based sealer and observed significantly reduced bacterial leakage with smear layer removal. Our findings and those of Clark-Holke et al. add to a growing body of evidence that the significance of the smear layer varies depending upon the type of sealer used [8, 9, 14, 15].
Drawing inference based upon in vitro bacterial leakage results is somewhat tenuous as varying experimental designs and protocols have produced conflicting results [16]. Isotope and dye penetration, glucose and fluid infiltration have all been used to assess coronal microleakage. The dual chamber bacterial method, as employed herein, is thought to best simulate clinical conditions [15, 17]. In order to minimize systematic error in dual chamber bacterial leakage studies, Rechenberg et al. [15] recommended the inclusion of better negative controls. We employed more negative controls than any previous dual chamber study. Our inherent assumption that turbidity of the lower chamber could not occur as a result of persistent biofilms on a root surface, or alternate pathways for leakage, was tested by the inclusion of five negative controls for each treatment group. Increased replication of controls allowed validation of our study design, but at the cost of reducing treatment sample size. Because treatment sample sizes were limited, 95% confidence intervals were included to qualify the data for proper interpretation.
Another limitation of the current study was the use of single strain planktonic bacteria. As was used in nearly all previous dual chamber bacterial leakage studies, this was not representative of nature. Endodontic infections are understood to be biofilm infections, the ecology and morphology of which can vary between cases [18, 19]. The resistance of biofilms to antimicrobials, and virulence of individual species within them, has been increasingly shown to vary largely from that of planktonic bacteria [20, 21].
With regard to the specific strain of bacteria used, Clark-Holke et al. employed Enterococcus faecalis, because it had been commonly observed in studies of failing endodontic cases [9]. Studies which were culture-based had implied a causative role for E. faecalis in failing endodontic cases [22,23,24]. However, using novel and more accurate DNA-based bacterial identification, Fouad et al. has now questioned whether E.Faecalis has any causative role in periradicular pathosis [25]. Moreover, specific strains of E. faecalis have been shown to differ in their ability to coexist in biofilms with other species [26]. Strep. mutans was selected for the current study because of its potential role in re-infecting obturated root canals, and because of its successful use in similar studies of in vitro bacterial leakage [13, 15].
Under the conditions and limitations of the current study, our data suggest that the removal of the smear layer (i.e. the use of EDTA) may be an unnecessary clinical step prior to endodontic obturation when ZOE-based sealer is used. Other studies have suggested that it may even be a deleterious clinical step. In their review, Prado et al [27] found that mixing EDTA with NaOCl, depending upon the local pH, may result in the loss of free available chlorine significantly reducing the ability of NaOCl to dissolve organic tissue. Based upon these and additional findings in their recent review, Wright et al. [28] corroborate these in vitro findings with a case report attributing a subcutaneous emphysema to gas formation, resulting from the interaction of EDTA with NaOCl. It was recommended that these irrigants not be mixed with one another. The conventional use of NaOCl as an effective irrigant during root canal therapy has been well established for several decades. EDTA has been added to common clinical protocol more recently, for the purpose of smear layer removal alone. In the intent of overall tooth survival, as mentioned earlier, the prospective study by Ng et al. [7] found the use of EDTA to be insignificant. When other than resin-based sealers are used, the EDTA flush may be an extraneous step that can be eliminated.
Many novel types of endodontic sealer are currently being introduced. These include methacrylate-, mineral trioxide aggregate (MTA)-, and bioceramic-based sealers. Bacterial leakage data for these sealers are sparse, and to date only Andriukaitiene et al. [14] has studied the effect of the smear layer. They observed that methacrylate-based sealers resisted leakage longer when the smear layer was intact, while leakage through MTA-based samples was unaffected. As new types of endodontic sealers are developed and tested, the significance of the smear layer should be considered, because of this established interaction between smear layer effect and sealer type.
Conclusions
Under the conditions and limitations of this in vitro study, retaining the smear layer appeared to slow the rate of bacterial leakage through coronally-exposed root canal obturations, when ZOE-based endodontic sealer was used. This finding adds to the growing body of evidence suggesting that the overall significance of the smear layer appears to vary depending upon the type of sealer used.
Abbreviations
- EDTA:
-
Ethylenediamenetetraacetic acid
- NaOCl:
-
Sodium hypochlorite
- MTA:
-
Mineral trioxide aggregate
- ZOE:
-
Zinc oxide eugenol
References
Violich DR, Chandler NP. The smear layer in endodontics - a review. Int Endod J. 2010;43:2–15.
Morago A, Ordinola-Zapata R, Ferrer-Luque CM, Baca P, Ruiz-Linares M, Arias-Moliz MT. Influence of smear layer on the antimicrobial activity of a sodium hypochlorite/Etidronic acid irrigating solution in infected dentin. J Endod. 2016;42:1647–50.
Behrend GD, Cutler CW, Gutmann JL. An in-vitro study of smear layer removal and microbial leakage along root-canal fillings. Int Endod J. 1996;29:99–107.
Shahravan A, Haghdoost A-A, Adl A, Rahimi H, Shadifar F. Effect of smear layer on sealing ability of canal obturation: a systematic review and meta-analysis. J Endod. 2007;33:96–105.
Pashley DH, Michelich V, Kehl T. Dentin permeability: effects of smear layer removal. J Prosthet Dent. 1981;46:531–7.
Ørstavik D, Haapasalo M. Disinfection by endodontic irrigants and dressings of experimentally infected dentinal tubules. Endod Dent Traumatol. 1990;6:142–9.
Ng Y-L, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J. 2011;44:610–25.
Saleh IM, Ruyter IE, Haapasalo M, Ørstavik D. Bacterial penetration along different root canal filling materials in the presence or absence of smear layer. Int Endod J. 2008;1:32–40.
Clark-Holke D, Drake D, Walton R, Rivera E, Guthmiller JM. Bacterial penetration through canals of endodontically treated teeth in the presence or absence of the smear layer. J Dent. 2003;31:275–81.
Ricucci D, Rocas IN, Alves FR, Loghin S, Siquiera JF Jr. Apically extruded sealers: fate and influence on treatment outcome. J Endod. 2016;42:243–9.
Augsburger RA, Peters DD. Radiographic evaluation of extruded obturation material. J Endod. 1990;16:492–7.
U.S. Department of Health and Human Services. Code of Federal Regulations Title 45 Part 46 Protection of Human Subjects. Washington D.C. (2009). http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.102. Accessed 8 Nov 2010.
Monticelli F, Sadek FT, Schuster GS, et al. Efficacy of two contemporary single-cone filling techniques in preventing bacterial leakage. J Endod. 2007;33:310–3.
Andriukaitiene L, Song X, Yang N, Lassila LVJ, Vallittu PK, Kerosuo E. The effect of smear layer removal on E. faecalis leakage and bond strength of four resin-based root canal sealers. BMC Oral Health. 2018;18:213.
Shipper G, Trope M. In vitro microbial leakage of endodontically treated teeth using new and standard obturation techniques. J Endod. 2004;30:154–8.
Rechenberg D-K, De-Deus G, Zehnder M. Potential systematic error in laboratory experiments on microbial leakage through filled root canals: review of published articles. Int Endod J. 2011;44:183–94.
De-Deus G. New directions in old leakage methods. Int Endod J. 2008;41:720–3.
Svensäter G, Bergenholz G. Biofilms in endodontic infections. Endod Top. 2005;9:27–36.
Ricucci D, Siquiera JF. Biofilms and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod. 2010;36:1277–88.
Chavez de Paz LE, Bergenholz G, Svensäter G. The effects of antimicrobials on endodontic biofilm infections. J Endod. 2010;36:70–7.
Sedgley CM, Lee EH, Martin MJ, Flannagan SE. Antibiotic resistance gene transfer between Streptococcus gordoni and E. faecalis in root canals of teeth ex vivo. J Endod. 2008;34:57–64.
Sundqvist G, Figdor D, Persson S, Sjögren U. Microbiologic analysis of teeth with failed endodontic treatment and the outcome of conservative treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:86–93.
Siquiera JF Jr, Rocas IN. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod. 2008;34:1291–301.
Hancock HH III, Sigurdsson A, Trope M, Moiseiwitsch J. Bacteria isolated after unsuccessful endodontic treatment in a north American population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:579–86.
Fouad AF, Zerelia J, Barry J, Spǻngberg LS. Molecular detection of Enterococcus species in root canals of therapy-resistant endodontic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:112–8.
Chavez de Paz LE, Davies JR, Bergenholz G, Svensäter G. Strains of Enterococcus faecalis differ in their ability to coexist in biofilms with other root canal bacteria. Int Endod J. 2015;48:916–25.
Prado M, Santos Junior HM, Rezende CM, Pinto AC, Faria RB, Simão RA, et al. Interactions between irrigants commonly used in endodontic practice: a chemical analysis. J Endod. 2013;39:505–10.
Wright PP, Kahler B, Walsh LJ. Alkaline sodium hypochorite irrigant and its chemical interactions. Materials (Basel). 2017;10:1–8.
Acknowledgements
The authors thank West Michigan Oral and Maxillofacial Surgery, Holland, Michigan U.S.A. for providing teeth for this study. For proof reading the manuscript, the authors thank Dr. Laura Altfeld and Dr. Howard Carey, Saint Leo University, Mathematics & Sciences Department, 33701 State Road 52, Saint Leo, FL, USA 33574. The authors further thank personnel of the Mathematics & Sciences Department, St. Leo University for use of their laboratory facilities and for provision of culture media and bacterial strains.
Funding
The authors declare that, besides that mentioned under Acknowledgements, the current study was entirely self-funded.
Author information
Authors and Affiliations
Contributions
HAB performed 100% of all bacteriologic procedures and the running of the entire experiment. HAB contributed 50% to manuscript preparation. HAB also presented the study before peers at Saint Leo University. BJB performed 100% of processing, cleaning and shaping, and obturating of root samples. BJB contributed 50% to manuscript preparation. Both authors equally participated in initial setting up of the experiment. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All clinical protocol, including the use of discarded teeth without individual patient consent, was approved by the Institutional Review Board of Saint Leo University, Saint Leo, FL. (CITI Record ID 26213030), according to regulations instituted by the U.S. Department of Health and Human Services [12].
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Buurma, H.A., Buurma, B.J. The effect of smear layer on bacterial penetration through roots obturated using zinc oxide eugenol-based sealer. BMC Oral Health 20, 88 (2020). https://doi.org/10.1186/s12903-020-01069-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-020-01069-8