Abstract
Introduction
Denosumab, a fully human anti-RANKL monoclonal antibody, is a widely used osteoporosis treatment that is increasingly being used in patients undergoing dialysis; however, its long-term efficacy and safety in these patients remain unknown.
Materials and methods
This observational study comprised individuals aged ≥ 20 years undergoing hemodialysis and receiving denosumab. After denosumab administration, we analyzed the long-term changes in bone mineral density (BMD) and levels of bone turnover markers (BTMs) and calcium.
Results
The study included 45 patients who have been receiving denosumab for a median duration of 3.8 (interquartile range, 2.5–6.7) years. Tartrate-resistant acid phosphatase 5b (TRACP-5b) levels decreased from a median of 595 (434–778) mU/dL at baseline to 200 (141–430) mU/dL after 6 months of denosumab administration (P < 0.001) and remained low thereafter. Similarly, bone-specific alkaline phosphatase (BAP) levels decreased from a median of 18.2 (15.9–25.8) μg/L at baseline to 12.4 (9.9–15.6) μg/L after 6 months (P < 0.001) and remained low thereafter. Meanwhile, BMD, as assessed with dual energy X-ray absorptiometry and measured at the distal 1/3 of the radius, did not decrease (0.465 ± 0.112 g/cm2 at baseline vs. 0.464 ± 0.112 g/cm2 after administration; P = 0.616). Regarding hypocalcemia, corrected calcium levels reached were the lowest at 7 days after administration and normalized within 30 days.
Conclusion
The study showed long-term suppression of TRACP-5b and BAP levels and sustaining BMD after denosumab administration over an extended period in patients undergoing hemodialysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients undergoing dialysis have a five-fold higher risk of experiencing fractures compared with the general population [1]; once a fracture occurs, their risk of death increases [2, 3]. Consequently, preventing fractures in patients undergoing dialysis not only improves their quality of life but also their prognosis. The pathogenesis of osteoporosis in patients on dialysis is more complex than that in the general population as impaired renal function leads to various pathologies, including anemia and chronic kidney disease-mineral and bone disorder (CKD-MBD), that also affect bone metabolism [4]. Exhaustive systematic reviews focusing on osteoporosis therapeutics in the chronic kidney disease (CKD) subset have yielded insufficient evidence of the effectiveness of each therapeutic agent within this group, and paradigms for fracture deterrence in patients undergoing dialysis are still in the early stages [5].
Denosumab, a human anti-RANKL monoclonal antibody, decreases bone resorption and is used to treat osteoporosis [6]. Several studies have indicated that denosumab restores bone mineral density (BMD) and prevents bone fractures, with a relative risk reduction of 40%–68% in the general population [4, 7,8,9,10,11,12,13,14]. The effect of denosumab is even more significant in patients with CKD, including those on dialysis, as it eliminates the need for volume regulation of renal function [10, 15]. Although several observational studies have been conducted on patients with CKD [14, 16,17,18], there is a lack of research investigating the long-term effects of denosumab on bone turnover markers (BTMs) and BMD within this group.
Currently, long-term efficacy and safety of denosumab in patients undergoing hemodialysis remain unknown, and the same is true for its long-term effects on BMD and bone mineral metabolism. A more comprehensive repository of information is warranted to establish denosumab as a preventive drug against fractures in patients undergoing hemodialysis. Therefore, we designed an observational study involving patients on hemodialysis receiving denosumab to determine changes in BMD and levels of BTMs and calcium (Ca).
Materials and Methods
Study design
In this observational retrospective study, we investigated changes in BMD and levels of BTMs and Ca in patients undergoing hemodialysis and receiving denosumab.
Ethics approval
All procedures involving human participants were approved by the institutional review board of our hospital (approval number: 34–387 [11544]) and conducted in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments. Due to the retrospective nature of this study, the need to obtain informed consent from patients was waived by the institutional review board.
Data source and patient selection
Our investigation involved individuals aged ≥ 20 years who were undergoing hemodialysis in Keijin Hospital, a maintenance hemodialysis center in Tokyo, Japan. The attending physician made the decision for denosumab administration based on the Japanese guidelines for osteoporosis [19]. The chronological term for this research extended from December 2013 through December 2022, during which time data were gathered retrospectively over a median duration of 3.8 (interquartile range [IQR]: 2.5–6.7) years for each patient.
Clinical parameters
Blood tests were performed at the beginning of the week before the start of hemodialysis. Levels of hemoglobin (g/dL), urea nitrogen (mg/dL), creatinine (mg/dL), albumin (Alb) (g/dL), Ca (mg/dL), phosphate (mg/dL), magnesium (mg/dL), alkaline phosphatase (U/L), intact parathyroid hormone (PTH) (pg/mL), tartrate-resistant acid phosphatase 5b (TRACP-5b) (mU/dL), and bone-specific alkaline phosphatase (BAP) (μg/L) were measured using standard commercial assays. For serum Ca levels, the corrected Ca (cCa) level was calculated as follows if the serum albumin level was < 4.0 mg/dL: cCa = Ca + 4.0—Alb. BMD was assessed by dual-energy X-ray absorptiometry (DXA; Dichroma Scan, DCS-600 EXV, Hitachi Aloka Medical, Tokyo, Japan) and measured at the distal 1/3 of the radius. Patients in this study underwent BMD measurements once a year, and measurements before denosumab administration and at the end of the observation period were evaluated. We also reviewed medications and comorbidities based on medical records.
Statistical analyses
Data are presented as means ± standard deviations or medians with IQR. First, we showed changes in BMD and levels of BTMs, cCa, phosphate, and intact PTH using box-beard diagrams (point: median; box, IQR; beard, 95% confidence interval [CI]), and each change was tested using the paired-sample t test. Thereafter, associations between TRACP-5b, BAP, and intact PTH levels and decrease of cCa levels were evaluated by determining the correlation coefficient and illustrating scatter plots and regression lines. All tests performed during this study were two-sided, with a P value < 0.05 indicating statistical significance. A complete case analysis was performed when data were missing. All statistical analyses were performed using Stata version 15.1 (StataCorp LLC, College Station, TX, USA).
Results
Patient characteristics
The study included 45 patients who had available data on BMD and levels of BTMs and cCa after denosumab administration. Table 1 presents the characteristics of all patients in this study. The median (25–75%) patient age was 75 (range 70–80) years. Patients had been undergoing dialysis for a median of 55 (24–113) months. All patients received denosumab every 6 months during the observation period.
Changes in BTM levels following denosumab administration
Figure 1 shows the changes in TRACP5-b and BAP levels over time. TRACp-5b levels decreased from a median of 595 (434–778) mU/dL at baseline to 200 (141–430) mU/dL after 6 months of denosumab administration and remained low thereafter. Similarly, BAP levels decreased from a median of 18.2 (15.9–25.8) μg/L at baseline to 12.4 (9.9–15.6) μg/L after 6 months of administration and remained low thereafter. All post-administration TRACP5-b and BAP levels were significantly lower than the baseline levels (P < 0.001).
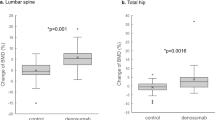
Changes in BMD following denosumab administration
BMD did not significantly change before and after denosumab administration, from a mean BMD of 0.465 (± 0.112) g/cm2 at baseline to a mean BMD of 0.464 (± 0.112) g/cm2 after administration (P = 0.616) (Fig. 2).
Changes in cCa levels following denosumab administration
CCa levels were the lowest at a median of 8.3 (7.7–9.3) mg/dL on the seventh day after administration and subsequently increased to a median of 9.2 mg/dL, similar to the baseline levels (Fig. 3).
Correlation between BTMs and cCa decreased
Figure 4 and Supplementary Fig. 1 show the correlation between intact PTH, BAP, and TRACP5-b levels and the cCa decrease at 7 days of administration, as well as the maximum decrease in cCa until 30 days of administration, respectively. The correlation coefficient between the decrease in cCa levels at day 7 and intact PTH is − 0.17, while it is 0.22 with BAP, and 0.17 with TRACP5-b. These coefficients change to − 0.22 for PTH, 0.19 for BAP, and 0.14 for TRACP5-b at 30 days. Hence, BTMs were not significantly correlated with lower cCa levels.
Changes in phosphate and intact PTH levels
Supplementary Figs. 2 and 3 show the changes in phosphate and intact PTH levels. Phosphate levels were the lowest at a median of 3.5 (2.8–4.3) mg/dL on the seventh day after administration and subsequently increased to a median of 4.1 mg/dL, similar to baseline levels (Supplementary Fig. 2). Intact PTH levels did not change significantly after denosumab administration and generally remained less than 200 pg/mL (Supplementary Fig. 3).
Discussion
In the present study, continuous denosumab administration rapidly reduced TRACP5-b and BAP levels, which remained low throughout the extended observation period. Meanwhile, BMD was maintained during the observation period. Regarding hypocalcemia, cCa levels reached their lowest at 7 days after denosumab administration and normalized within 30 days. Previous studies reporting changes in BTMs in patients undergoing hemodialysis after denosumab administration had a short follow-up period of 1 or 2 years [4, 16, 17], and they emphasized the need to determine the long-term trends in bone metabolism markers. Additionally, it was unknown whether suppression of bone turnover following denosumab administration was sustained over time. Thus, this study is the first to report that denosumab causes long-term suppression of BTMs.
Bone biopsy is the gold standard for assessing bone metabolism. However, it is invasive and complex to perform routinely in clinical practice. In contrast, measuring BTM levels is noninvasive and amenable to recurrent testing, facilitating longitudinal assessments of shifts in bone metabolism. Elevated TRACP5-b levels in the general population suggest increased bone resorption, making TRACP a widely used quantitative BTM [20]. Moreover, TRACP5-b is not influenced by renal function; hence, it is suitable for evaluating bone resorption in patients undergoing hemodialysis [20]. Notably, previous studies on denosumab in patients undergoing hemodialysis have reported a rapid decrease in TRACP5-b levels after administration [4, 16, 17].
BAP, which constitutes approximately half of the alkaline phosphatase derived from diverse tissues, is a crucial biomarker for bone formation assessment. BAP reportedly helps determine if bone formation is downregulated in the general population [21], and it is a beneficial marker in patients undergoing hemodialysis because it is not affected by renal function. Furthermore, BAP levels are significant predictors of fracture risk in patients undergoing hemodialysis [22]. Previous studies on denosumab in patients undergoing hemodialysis have also shown a rapid decrease in BAP levels after administration [4, 16, 17] similar to the present study, suggesting that the inhibition of bone resorption by denosumab concurrently leads to a reduction in bone formation.
Earlier reports in the general population have indicated that extended use of denosumab leads to the continuous suppression of TRACP5-b and BAP [23]. However, the long-term trends of these BTMs in patients on hemodialysis have yet to be explored. In this study, we showed for the first time that long-term administration of denosumab continuously suppressed TRACP5-b and BAP in patients undergoing hemodialysis.
The DXA technique employs two distinct X-rays and is widely used to estimate fracture risk in the general population [24]. Although it remains inconclusive whether BMD measured by DXA effectively estimates fracture risk in patients undergoing hemodialysis [24], several observational studies have shown that BMD measured by the DXA method correlated with fracture risk in these patients [22, 25], suggesting that the DXA method, which can be easily performed in clinical settings, may help assess fracture risk in patients undergoing hemodialysis [26, 27]. Several clinical studies have reported that denosumab treatment is associated with maintaining or improving BMD at the femoral neck, lumbar spine, and distal radius [11]. Consistent with these findings, this study demonstrated long-term maintenance of BMD after denosumab administration, albeit specifically at the distal radius. However, measuring BMD at the distal radius is reportedly unsuitable for assessing the effects of denosumab [17], which is one of the limitations of this study. Although this study assessed BMD at the distal radius due to the facility and instrumentation, measuring BMD at the lumbar spine and femoral neck may have been ideal in terms of evaluating the effect of denosumab on BMD.
Hypocalcemia is a serious adverse effect denosumab and also occurs in patients with CKD, with an incidence rate of 15% [28]. The postulated mechanism parallels the dynamics of hungry bone syndrome observed after parathyroidectomy wherein the suppression of bone resorption induced by denosumab leads to an augmented Ca flux from the blood into the bone, culminating in acute hypocalcemia [29]. Prior studies have indicated that high baseline BAP and TRACP-5b levels are risk factors for hypocalcemia in patients undergoing hemodialysis based on the hypothesis that high bone turnover is associated with enhanced denosumab efficacy [16,17,18].
In this study, no significant associations were observed between hypocalcemia and BAP or TRACP-5b levels. Within the healthcare institution that facilitated this retrospective study, patients with a high risk of hypocalcemia attributable to denosumab were administered with prophylactic oral calcium supplementation. Such treatment might have confused the relationship between Ca and BTMs in this investigation. Hence, the findings of this study cannot conclusively rule out the potential link between baseline BTMs and hypocalcemia.
Although phosphate levels were the lowest on the seventh day after administration, they returned to baseline levels after 60 days and thereafter remained within the 3.5–6 mg/dL range, which is the recommended range by the Japanese CKD-MBD guidelines. [30] As in a previous report, [4] denosumab administration did not significantly change PTH levels, and there were no signs of changes in parathyroid function in the present study.
This study had several limitations. First, this study only included patients treated with denosumab, and a comparative reference group was lacking. Therefore, this study could not evaluate whether denosumab has therapeutic effects. Second, the difficulty in collecting longitudinal data on Ca supplementation and drugs that affect calcium, phosphate, and PTH levels, such as vitamin D analogs, prevented us from examining the effects of these changes on cCa levels after denosumab administration. Third, we could not analyze the occurrence of fractures due to the small number of patients and the inability to include a comparison group that did not receive denosumab. Fourth, only two points were used to assess BMD, and the possibility of measurement errors cannot be ruled out. Finally, the limited number of cases hindered the use of multivariate linear regression models to examine the association between BTMs and hypocalcemia, which led to analysis using scatter plots and regression lines. Future prospective and large-scale studies with whole-body BMD assessments are essential to elucidate the long-term effects of denosumab on the bone of patients undergoing hemodialysis.
In conclusion, the study showed long-term suppression of TRACP-5b and BAP levels and sustaining BMD after denosumab administration over an extended period in patients undergoing hemodialysis.
References
Wakasugi M, Kazama JJ, Taniguchi M, Wada A, Iseki K, Tsubakihara Y, Narita I (2013) Increased risk of hip fracture among Japanese hemodialysis patients. J Bone Miner Metab 31:315–321
Mittalhenkle A, Gillen DL, Stehman-Breen CO (2004) Increased risk of mortality associated with hip fracture in the dialysis population. Am J Kidney Dis 44:672–679
Tentori F, McCullough K, Kilpatrick RD, Bradbury BD, Robinson BM, Kerr PG, Pisoni RL (2014) High rates of death and hospitalization follow bone fracture among hemodialysis patients. Kidney Int 85:166–173
Iseri K, Watanabe M, Yoshikawa H, Mitsui H, Endo T, Yamamoto Y, Iyoda M, Ryu K, Inaba T, Shibata T (2019) Effects of denosumab and alendronate on bone health and vascular function in hemodialysis patients: a randomized, controlled trial. J Bone Miner Res 34:1014–1024
Wilson LM, Rebholz CM, Jirru E, Liu MC, Zhang A, Gayleard J, Chu Y, Robinson KA (2017) Benefits and harms of osteoporosis medications in patients with chronic kidney disease: a systematic review and meta-analysis. Ann Intern Med 166:649–658
Delmas PD (2008) Clinical potential of RANKL inhibition for the management of postmenopausal osteoporosis and other metabolic bone diseases. J Clin Densitom 11:325–338
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C, Trial FREEDOM (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Nakamura T, Matsumoto T, Sugimoto T, Hosoi T, Miki T, Gorai I, Yoshikawa H, Tanaka Y, Tanaka S, Sone T, Nakano T, Ito M, Matsui S, Yoneda T, Takami H, Watanabe K, Osakabe T, Shiraki M, Fukunaga M (2014) Clinical trials express: fracture risk reduction with denosumab in Japanese postmenopausal women and men with osteoporosis: denosumab fracture intervention randomized placebo controlled trial (DIRECT). J Clin Endocrinol Metab 99:2599–2607
Lin T, Wang C, Cai XZ, Zhao X, Shi MM, Ying ZM, Yuan FZ, Guo C, Yan SG (2012) Comparison of clinical efficacy and safety between denosumab and alendronate in postmenopausal women with osteoporosis: a meta-analysis. Int J Clin Pract 66:399–408
Jamal SA, Ljunggren O, Stehman-Breen C, Cummings SR, McClung MR, Goemaere S, Ebeling PR, Franek E, Yang YC, Egbuna OI, Boonen S, Miller PD (2011) Effects of denosumab on fracture and bone mineral density by level of kidney function. J Bone Miner Res 26:1829–1835
Thongprayoon C, Acharya P, Acharya C, Chenbhanich J, Bathini T, Boonpheng B, Sharma K, Wijarnpreecha K, Ungprasert P, Gonzalez Suarez ML, Cheungpasitporn W (2018) Hypocalcemia and bone mineral density changes following denosumab treatment in end-stage renal disease patients: a meta-analysis of observational studies. Osteoporos Int 29:1737–1745
Chen CL, Chen NC, Hsu CY, Chou KJ, Lee PT, Fang HC, Renn JH (2014) An open-label, prospective pilot clinical study of denosumab for severe hyperparathyroidism in patients with low bone mass undergoing dialysis. J Clin Endocrinol Metab 99:2426–2432
Hiramatsu R, Ubara Y, Sawa N, Hoshino J, Hasegawa E, Kawada M, Imafuku A, Sumida K, Mise K, Hayami N, Suwabe T, Takaichi K (2015) Denosumab for low bone mass in hemodialysis patients: a noncontrolled trial. Am J Kidney Dis 66:175–177
Iseri K, Mizobuchi M, Winzenrieth R, Humbert L, Saitou T, Kato T, Nakajima Y, Wakasa M, Shishido K, Honda H (2023) Long-term effect of Denosumab on bone disease in patients with CKD. Clin J Am Soc Nephrol 18:1195–1203
Block GA, Bone HG, Fang L, Lee E, Padhi D (2012) A single-dose study of denosumab in patients with various degrees of renal impairment. J Bone Miner Res 27:1471–1479
Hiramatsu R, Ubara Y, Sawa N, Sakai A (2021) Hypocalcemia and bone mineral changes in hemodialysis patients with low bone mass treated with denosumab: a 2-year observational study. Nephrol Dial Transplant 36:1900–1907
Kunizawa K, Hiramatsu R, Hoshino J, Mizuno H, Ozawa Y, Sekine A, Kawada M, Sumida K, Hasegawa E, Yamanouchi M, Hayami N, Suwabe T, Sawa N, Ubara Y, Takaichi K (2020) Denosumab for dialysis patients with osteoporosis: a cohort study. Sci Rep 10:2496
Hori M, Yasuda K, Takahashi H, Kondo C, Shirasawa Y, Ishimaru Y, Sekiya Y, Morozumi K (2022) Maruyama S (2022) effects of bone turnover status on the efficacy and safety of Denosumab among haemodialysis patients. Sci Rep 12:7781
Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, Ohta H, Shiraki M, Sugimoto T, Suzuki T, Soen S, Nishizawa Y, Hagino H, Fukunaga M, Fujiwara S (2012) Japanese 2011 guidelines for prevention and treatment of osteoporosis—executive summary. Arch Osteoporos 7:3–20
Nishizawa Y, Inaba M, Ishii M, Yamashita H, Miki T, Goto H, Yamada S, Chaki O, Kurasawa K, Mochizuki Y (2008) Reference intervals of serum tartrate-resistant acid phosphatase type 5b activity measured with a novel assay in Japanese subjects. J Bone Miner Metab 26:265–270
Kress BC, Mizrahi IA, Armour KW, Marcus R, Emkey RD, Santora AC 2nd (1999) Use of bone alkaline phosphatase to monitor alendronate therapy in individual postmenopausal osteoporotic women. Clin Chem 45:1009–1017
Iimori S, Mori Y, Akita W, Kuyama T, Takada S, Asai T, Kuwahara M, Sasaki S, Tsukamoto Y (2012) Diagnostic usefulness of bone mineral density and biochemical markers of bone turnover in predicting fracture in CKD stage 5D patients—a single-center cohort study. Nephrol Dial Transplant 27:345–351
Eastell R, Christiansen C, Grauer A, Kutilek S, Libanati C, McClung MR, Reid IR, Resch H, Siris E, Uebelhart D, Wang A, Weryha G, Cummings SR (2011) Effects of denosumab on bone turnover markers in postmenopausal osteoporosis. J Bone Miner Res 26:530–537
Jamal SA, West SL, Miller PD (2012) Fracture risk assessment in patients with chronic kidney disease. Osteoporos Int 23:1191–1198
Jamal SA, Hayden JA, Beyene J (2007) Low bone mineral density and fractures in long-term hemodialysis patients: a meta-analysis. Am J Kidney Dis 49:674–681
Disease K (2011) Improving global outcomes (KDIGO) CKD-MBD update work group (2017) KDIGO 2017 clinical practice guideline update for the diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 7:1–59
Evenepoel P, Cunningham J, Ferrari S, Haarhaus M, Javaid MK, Lafage-Proust MH, Prieto-Alhambra D, Torres PU, Cannata-Andia J, European Renal Osteodystrophy (EUROD) workgroup; an initiative of the CKD-MBD working group of the ERA-EDTA; and the committee of Scientific Advisors and National Societies of the IOF (2021) Diagnosis and management of osteoporosis in chronic kidney disease stages 4 to 5D: a call for a shift from nihilism to pragmatism. Osteoporos Int 32:2397–2405
Huynh AL, Baker ST, Stewardson AJ, Johnson DF (2016) Denosumab-associated hypocalcaemia: incidence, severity and patient characteristics in a tertiary hospital setting. Pharmacoepidemiol Drug Saf 25:1274–1278
Festuccia F, Jafari MT, Moioli A, Fofi C, Barberi S, Amendola S, Sciacchitano S, Punzo G, Menè P (2017) Safety and efficacy of denosumab in osteoporotic hemodialysed patients. J Nephrol 30:271–279
Fukagawa M, Yokoyama K, Koiwa F, Taniguchi M, Shoji T et al (2013) Clinical practice guideline for the management of chronic kidney disease-mineral and bone disorder. Ther Apher Dial 17:247–288
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Research idea and study design: K.K., A.N., and T.Y.; data acquisition: K.K., A.K., and T.Y.; data analysis/interpretation: K.K. and A.N.; statistical analysis: K.K. and A.N.; and supervision or mentorship: I.O. and T.Y. Each author contributed important intellectual content during manuscript drafting or revision and accepted accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work were appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethical approval
All procedures involving human participants were approved by the institutional review board of our hospital (approval number: 34–387 [11544]) and conducted in accordance with the ethical standards of the 1964 Helsinki Declaration and its later amendments.
Patient consent
As this was a retrospective study, the need to obtain informed consent from patients was waived by the institutional review board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kato, K., Yaginuma, T., Kobayashi, A. et al. Long-term effects of denosumab on bone mineral density and turnover markers in patients undergoing hemodialysis. J Bone Miner Metab 42, 264–270 (2024). https://doi.org/10.1007/s00774-024-01505-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-024-01505-7







