Abstract
Introduction
Patients with multiple sclerosis (MS) commonly present musculoskeletal disorders characterized by lower bone mineral density (BMD) and muscle weakness. However, the underlying etiology remains unclear. Our objective is to identify shared pleiotropic genetic effects and estimate the causal relationship between MS and musculoskeletal disorders.
Materials and Methods
We conducted linkage disequilibrium score regression (LDSR), colocalization, and Mendelian randomization (MR) analyses using summary statistics from recent large-scale genome-wide association studies (GWAS), encompassing MS, falls, fractures, and frailty. Additional MR analyses explored the causal relationship with musculoskeletal risk factors, such as BMD, lean mass, grip strength, and vitamin D.
Results
We observed a moderate genetic correlation between MS and falls (RG = 0.10, P-value = 0.01) but not between MS with fracture or frailty in the LDSR analyses. MR revealed MS had no causal association with fracture and frailty but a moderate association with falls (OR: 1.004, FDR q-value = 0.018). We further performed colocalization analyses using nine SNPs that exhibited significant associations with both MS and falls in MR. Two SNPs (rs7731626 on ANKRD55 and rs701006 on OS9 gene) showed higher posterior probability of colocalization (PP.H4 = 0.927), suggesting potential pleiotropic effects between MS and falls. The nine genes are associated with central nervous system development and inflammation signaling pathways.
Conclusion
We found potential pleiotropic genetic effects between MS and falls. However, our analysis did not reveal a causal relationship between MS and increased risks of falls, fractures, or frailty. This suggests that the musculoskeletal disorders frequently reported in MS patients in clinical studies are more likely attributed to secondary factors associated with disease progression and treatment, rather than being directly caused by MS itself.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) is a demyelinating inflammatory autoimmune disorder characterized by continuous and diffuse changes in the white and grey matter, and damage to axons [1]. Despite recent advancements in disease-modifying therapies, patients with MS still exhibit an increased risk of musculoskeletal disorders including incidents of accidents and falls [2], fractures [3, 4], and frailty [5] when compared to unaffected controls.
Falls represent a debilitating consequence of MS, with as many as 56% of MS patients experiencing falls in any 3-month period [2]. A meta-analysis encompassing nine cohort studies suggests 1.58 times increased risk of fractures among patients with MS in comparison to their non-affected counterparts [6]. Frailty is an indicator of poor prognosis in patients suffering from systemic sclerosis [5] and a significantly higher percentage of MS patients display frailty in comparison to the control group, with percentages of 28% and 8%, respectively [5].
Multiple risk factors for developing musculoskeletal disorders in patients with MS have been proposed. These include systemic bone loss by chronic inflammatory status [7], muscle weakness due to immobility [8], ataxia from disruption of neuronal impulses [9], and bone and muscle loss due to MS treatment such as corticosteroid use [10]. In addition to these secondary factors, intrinsic elements of MS etiology may also be associated with increased musculoskeletal disorders. For instance, even early-stage comparatively young MS patients with minimal or no physical disability also displayed low bone mineral density (BMD) [11].
However, most of the findings were typical observational studies not eliminating potential biases from undefined residual confounding and reverse causation. Consequently, gaining a deeper understanding of the impact of genetically unmodifiable predisposing factors will provide valuable insights into the care of patients with MS.
To address this, we implemented LD score regression, colocalization and multiple Mendelian Randomization (MR) approaches to estimate the genetic pleiotropic effect and direct MS effects to 3 musculoskeletal outcomes (fracture, falls, and frailty) adjusting for the confounding effects from well-established bone and muscle disorder-related predisposing factors such as bone mineral density (BMD), lean body mass (whole body fat-free mass, appendicular lean mass), grip strengths and vitamin D levels.
We performed the following analyses: (1) Linkage Disequilibrium Score Regression (LDSR) to assess genetic heritability and genetic pleiotropy (correlations) between MS and 3 musculoskeletal traits (falls, fracture, and frailty) and predisposing factors; (2) Univariable and multivariable MR to assess the causal effect of MS on falls, fracture, and frailty, and heel estimated BMD (eBMD), whole body fat-free mass, appendicular lean mass, grip strengths and vitamin D levels; (3) Bidirectional MR to assess the directionality among fracture, falls, frailty; (4) Colocalization analysis to delineate shared genetic variants.
Materials and Methods
Linkage Disequilibrium Score Regression (LDSR)
LDSR can estimate cross-trait genetic correlations using GWAS summary statistics data [12]. We conducted LDSR analyses with the LD Hub interface [13] and the LDSC package (https://github.com/bulik/ldsc). We restricted our LDSR analyses to well-imputed SNPs (imputation quality score > 0.8) and SNPs with Minor Allele Frequency (MAF) ≥ 5% in the study populations. In addition, because outliers can unduly influence the regression, we also excluded SNPs with extremely large effect sizes (X12 > 80) [14]. The MS GWAS (47,429 MS cases and 68,374 non-MS healthy controls) summary statistics was obtained from the recent MS GWAS meta-analysis of the International Multiple Sclerosis Genetics Consortium (IMSGC) [15]. As for other musculoskeletal traits, we used GWAS summary statistics from the UK Biobank with the LD hub pipeline to estimate genetic heritability and assess correlations with MS.
Mendelian Randomization (MR)
MR is a widely used method using measured variation in genes (genotypes, SNPs) of exposure to examine the causal effect of exposures on disease outcomes in observational studies [16, 17].
Most GWAS summary statistics data were downloaded from the “MRC IEU OpenGWAS database” repository (https://gwas.mrcieu.ac.uk/) or each GWAS consortia.
The information on diagnostic criteria, phenotype definition, sample size, name of consortium, and dataset IDs from the database are available in Supplementary Table 1. The overall study design for MR is displayed in Fig. 1.
Exposure data
Instrumental variables (IVs) for MS were obtained from the recent GWAS meta-analysis of the IMSGC [15]. The detailed analysis and results description are provided in the previous IMSGC publication [15]. The estimated MS heritability is ~ 48%. Among the genome-wide significantly associated SNPs (p-values ≤ 5 × 10–8), 200 SNPs are located in the autosomal and non-MHC genomic region. Among these 200 SNPs, we further excluded 91 SNPs in LD with the lead SNPs. A total of 109 genome-wide associated SNPs were selected as IVs for MR analysis. The Effect allele, reference allele, effect allele frequency, and effect size information on these 109 SNPs are summarized in Supplementary Table 2. The minor alleles of these 109 SNPs are all larger than 10% in study populations. The effect size (OR) ranges from 1.06 to 1.23.
Outcome data
Fracture and fall GWAS data used in the analysis were selected from the UK Biobank data, fractured/broken in the last 5 years (ID: ukb-b-13346, n = 44,502 cases and 415,887 controls) [18] and falls last year (ID: ukb-b-2535, n = 461,725). Frailty GWAS data were obtained from a study by Atkins et al. in 2019 (n = 175,226) [19].
Predisposing factors of musculoskeletal outcomes
Known bone and muscle strength-related factors were used as covariates in multivariable MR (MVMR). They are heel-estimated BMD (eBMD) [19], appendicular lean mass, whole body fat-free mass, right handgrip strength, left grip strength [20] vitamin D [21]. These covariates were considered in MVMR to control for their potential confounding effects on musculoskeletal three outcomes.
Statistical analysis
Univariable MR between MS and three musculoskeletal traits as well as predisposing factors
Univariable MR was applied to assess the causal relationship between MS and 3 musculoskeletal outcomes (fracture, falls, and frailty) and 5 predisposing factors. We additionally performed MR between 5 predisposing factors and 3 musculoskeletal outcomes to examine potential underlying pathways between them. Multi-instrument MR strategy was applied. This approach involves conducting single instrumental variable MR analyses for each exposure or risk factor independently, and then the MR results from these multiple instrumental variables were combined through a fixed-effect meta-analysis. This meta-analysis allowed us to estimate the overall causal relationships between the exposures (MS and predisposing factors), and musculoskeletal outcomes.
Multivariable MR (MVMR) between MS and three musculoskeletal outcomes adjusting for predisposing factors
We also applied regression-based MVMR to account for many variants having pleiotropic effects that are associated with multiple predisposing factors. This method provides coefficients or effect sizes that represent the direct causal effects of multiple sclerosis (MS) on three distinct musculoskeletal outcomes while holding other predisposing factors constant. The estimation of causal effects in MVMR involves performing regression analyses of the associations between genetic variants and the outcome of interest on the associations between the same genetic variants and the selected predisposing factors. The intercept in these regression analyses is set to zero, and the weights used are the inverse variances of the associations with the outcome [22]. Predisposing factors that demonstrated significant associations in the univariable MR analysis with each musculoskeletal trait were included in the MVMR analysis.
Bidirectional MR among the three musculoskeletal outcomes
Bidirectional MR was performed among fracture, falls, and frailty to examine their mutual effects and directionality considering their highly correlated nature. In bidirectional MR, instruments for both exposure and outcome are used to evaluate whether the “exposure” variable causes the “outcome” or whether the “outcome” variable causes the “exposure”[23].
Heterogeneity analysis
We employed Cochran’s Q statistic as a diagnostic tool to assess the heterogeneity of IVs. Heterogeneity can indicate a potential violation of the necessary assumptions for MR or the presence of pleiotropic effects, where a single genetic variant influences multiple traits. Cochran’s Q statistic derived from the inverse variance weighted (IVW) estimate should follow a χ2 distribution with degrees of freedom equal to the number of SNPs minus 1. When there is excessive heterogeneity, it suggests that either the modeling assumptions for MR have been violated or that some of the genetic variants are not adhering to the MR assumptions [24]. This is termed ‘horizontal pleiotropy’[25]. When Q statistics showed significant heterogeneity, we applied the MR-PRESSO [26] method to reassess the MR effects after filtering out outlier SNPs that may be responsible for the observed heterogeneity. After removing these outliers, we compared the MR results obtained from the MR-PRESSO adjusted analysis with the fixed-effects MR results derived from the IVW approach.
Sensitivity analysis
The sensitivity analysis including IVW, weighted median, weighted mode, and MR-Egger tests was performed in univariable MR analysis. For MVMR, IVW and MR-Egger tests were evaluated. We also applied the MR-Egger regression test [27] to verify horizontal pleiotropy in each MR. Among the multiple methods, we set the results from IVW and outlier removal results from MR-PRESSO as primary findings.
All the MR analyses were conducted in R (version 4.0.0) and specialized packages, including TwoSampleMR [28], MendelianRandomization [29], MRPRESSO [30], and the MR-Base platform [31]. The causal effect size (beta or OR) with standard error and p-values were presented as appropriately. We applied a false discovery rate (FDR, q) to account for multiple testing corrections. The criteria used to select final instrument variables in each MR were GWAS significance: p < 5e−8, LD clumping: r2 > 0.001 within a 10 MB window, and proxy SNPs in 1000 Genomes EUR, r2 = 0.8 [32].
Colocalization
We performed colocalization analysis to identify genetic variants that were associated with both multiple sclerosis (MS) and falls as potential pleiotropic genetic effects. The R COLOC package (https://chr1swallace.github.io/coloc/index.html) was used [33]. The R COLOC package calculates approximate Bayes Factors, which help quantify the evidence for colocalized genetic variants between two traits. We focused on examining a 500 kb region around each site (250 kb on either side) [34] specifically targeting nine SNPs that displayed a significant association in the MR analysis between MS and falls. The posterior probabilities of H0 (no causal variant), H1 (causal variant for trait 1 only), H2 (causal variant for trait 2 only), H3 (two distinct causal variants), and H4 (one common causal variant) are calculated. Among their output results, PP (Post-probability > 95%) H4 was used to determine the high probability of colocalized genetic variants between 2 traits. Conversely low PP4 (< 50%) means we cannot identify which individual SNP is jointly causal with confidence [35].
Results
Genetic heritability and correlations by LDSR
LDSR was performed using genetic information from 1,293,150 single nucleotide polymorphisms (SNPs) in the MS GWAS dataset. After merging with the reference panel for LD, a total of 1,109,876 SNPs remained for the final analysis. LDSR demonstrated that MS exhibits a statistically significant moderate genetic correlation with falls (rG: 0.105, P-value = 0.010) but not with fracture (rG: − 0.017, P-value = 0.711) or frailty (rG: 0.151, P-value = 0.082). Additionally, both handgrip strengths and both leg fat-free masses also showed a genetically significant correlation with MS. In contrast, the whole-body fat-free mass did not exhibit a significant genetic correlation with MS. The heritability of these traits estimated from GWAS summary statistics was low or considered not high; fracture (h2:0.019), falls (h2: 0.033), and frailty (h2: 0.109) (Table 1).
Mendelian Randomization
Univariable MR
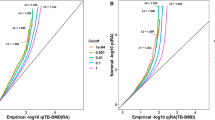
We didn’t find a significant causal relation between MS and fracture (OR: 1.002, 95% CI: 1.000–1.003, FDR q-value = 0.056); as well as no significant causal relation between MS and frailty (β: 0.009, 95% CI: 0.001–0.017, FDR q-value = 0.147) as shown in Table 2. After excluding outlier SNPs by MR-PRESSO and applying multiple testing corrections, we found a significant causal relation between MS and falls (OR: 1.004, 95% CI: 1.001–1.006, FDR q-value = 0.018). However, the causal relation between MS and falls has a moderate effect size (OR: 1.004), suggesting the causal relation is just a statistical significance due to large sample size in the MR analyses and may not be clinically meaningful. In addition to IVW and MR-PRESSO two MR methods, we performed additional MR analyses based on MR-egger, Weighted median and Weighted mode, three additional MR analyses. None of these additional MR analyses showed statistical significance (P-value > 0.05 on Supplementary Table 3). To evaluate the potential pleiotropic effect that may violate MR test assumption, a horizontal pleiotropy test was done by the MR Egger regression with the intercept test. We didn’t find any pleiotropy effect since the directionality p-value under the horizontal pleiotropy test are all > 0.05 (Supplementary Table 3). A scatter plot of univariable MR with multiple methods is presented in Fig. 2, suggesting a weak and positive causal relation between MS and falls. A funnel plot visualizing the MR results between MS and falls for each SNP was generated (Supplementary Fig. 1). No sign of genetic pleiotropy in IVW or MR-Egger methods was observed by funnel plot.
To further identify individual SNPs that contribute to MR analysis between MS and Falls, we performed MR analysis per SNP. Among 109 SNPs, 9 SNPs were found to be significantly associated between MS and falls (MR analysis p-values < 0.05 on supplementary Table 4). These 9 SNPs are rs9878602, rs7731626, rs9808753, rs10191360, rs11852059, rs1026916, rs701006, rs140522 and rs3737798 (Supplementary Table 4). Except for SNP rs10191360, all the other 8 SNPs showed positive causal relations between MS and Falls. Except for SNP rs9808753 (missense variant on the IFNGR2 gene), all the remaining 8 SNPs are non-coding variants and located in or near FOXP1, ANKRD55, GNNG2, STAT3, OS9, ODF3B and VANGL2 genes. These genes are involved in several pathophysiological pathways relevant to arthritis, infection, bone cancers, rhabdomyosarcoma, migraines, and neural tube defects (Supplementary Table 5).
Multivariable MR
In the MVMR analysis, adjustment of each predisposing factor observed by previous studies (that were identified as risk factors of musculoskeletal diseases) did not modify the overall MR results between MS and falls (P-values < 0.05 on Table 3). As for causal relation between MS and fractures, comparing to the unadjusted Model (univariate MR), similar results were found from MVMR analyses adjusting for each predisposing factor (Supplementary Table 6). The same MVMR analysis was also performed between MS and frailty. Compared to the unadjusted Model (univariate MR), similar results were found from MVMR analyses adjusting for each predisposing factor (Supplementary Table 7). The MVMR results suggested there are no clinical meaningful causal associations between MS and fractures as well as between MS and frailty.
Bidirectional MR among the 3 musculoskeletal outcomes
To account for the directional effects among the 3 musculoskeletal outcomes of fracture, fall, and frailty, we conducted bidirectional MR. Fall causally increased fracture risk (OR: 1.215, 95% CI: 1.098–1.345, P-value = 1.63E−04) and frailty risk (OR: 4.870, 95% CI: 2.412–9.832, P-value = 1.01E−05). Our results are consistent with previous findings that falls causally associated with an increased risk of fractures and frailty.
Colocalization analysis
In colocalization analysis using those nine significantly associated SNPs between MS and falls, two of them, rs7731626 and rs140522 presented over 92% colocalization rate (SNP probability of colocalization, single SNP PP.H4 = 0.927, supplementary Table 8).
Discussion
In this study, we identified genetic correlations with potentially shared pleiotropic effects between MS and falls proven by LDSR, colocalization, and MR. However, contrary to epidemiological observation of an increased risk of musculoskeletal traits (such as fractures and frailty) in MS patients, we did not find a meaningful causal relationship between MS and fractures as well as between MS and frailty via MR analyses. Specifically, none of the well-known muscle and bone-related predisposing factors (BMD, whole-body and appendicular fat-free masses, both grip strengths, and vitamin D) were causally affected by MS. In bidirectional MR among the three musculoskeletal outcomes (fracture, fall, and frailty), we found that falls causally increased the risk of both fracture and frailty. This observation is consistent with previous reports from many epidemiological studies; suggesting our MR analyses did have adequate statistical power and validated instrumental variables to pick up causal relation signals with the GWAS summary statistics we used. We further explored SNPs that are significantly associated with both MS and falls in a MR analysis. We identified 9 potential pleiotropic SNPs. These 9 SNPs are located in/near genes that are involved in pathophysiological pathways relevant to arthritis, infection, bone cancer, rhabdomyosarcoma, migraine, neural and tube defects. Two SNP rs7731626 and rs140522, located in/near ANKRD5 and OS9 genes are also confirmed by the by the colocalization analyses between MS GWAS and Falls GWAS. These two genes are associated with arthritis and bone cancer, suggesting the involvement in inflammation and autoimmunity in bone cells.
Most of the previous observational studies predominantly reported high fracture risk in MS in comparison to age-matched controls. For example, Bazelier et al. 2011 [36] reported threefold-increased hip fracture risk in patients with MS during 5 years of follow-up. In addition, the falls history was also higher in MS patients, suggesting increased fractures observed in MS patients in Bazelier et al.’s study might be due to an increased risk of falls. Falls are common in patients with MS. A large international data set demonstrated 56% MS patients fall at least once within 3 months period with 37% categorized as frequent fallers [2]. Notably, MS patients fall more frequently, experience more injurious falls, and are more likely to attribute their falls to tripping and distraction [37]. These epidemiological observations support our MR findings that MS causally increased the risk of falls.
Based on our genetic correlation, MR and colocalization analyses, it appears that genetic factors may causally increase risks for both MS and falls. However, it is important to note that the effects of these genetic factors on fall risk are relatively minimal; therefore, other non-genetic factors, such as medication effects may need to be taken into consideration. Medication use is a well-established risk factor for falls, either directly (affecting balance, attention, or muscle tone) or indirectly (as proxies of underlying conditions influencing the risk of falling; joint pain, arthrosis, and cardiovascular diseases). In particular, psychotropic drugs (antidepressants, anxiolytics, and anti-epileptics) use [38, 39] are strongly associated with falls in MS patients. A recent fall GWAS study examined the genetic correlation of falls with medication use and found medications such as opioids, anti-inflammatory and anti-rheumatic drugs and drugs for peptic ulcer and gastro-esophageal reflux disease were in positive genetic correlations with falls (40). Medication use associated with MS treatments and complications may be one of the strong risk factors for falls in MS patients.
Given the highly increased availability of public GWAS data, we could utilize LDSR, a multifaceted MR approach, and colocalization analysis together and could elucidate the causal relations and identify shared genetic pleiotropic effects to draw new perspectives on musculoskeletal traits in MS patients. However, it should be caution about the reliability and limitation of MR analyses due to the low heritability of many complex traits, including some of the musculoskeletal traits. Nevertheless, we are able to observe statistical significance causal relation between MS and falls and identify several possible shared pleiotropic genetic variants that genetically predisposed arthritis and bone cancers that might have a role in fall risk in MS patients.
In conclusion, our study does not provide evidence to support the notion that multiple sclerosis (MS) causally increases the risks of fractures and frailty. The musculoskeletal disorders frequently observed in clinical studies among MS patients may be more likely attributable to secondary factors associated with MS disease progression and its treatment. We identified genetic association between MS and falls with shared pleiotropic genetic factors.
References
Lassmann H. Pathogenic Mechanisms Associated With Different Clinical Courses of Multiple Sclerosis. Front Immunol. 2019;10.
Nilsagård Y, Gunn H, Freeman J, Hoang P, Lord S et al (2015) Falls in people with MS–an individual data meta-analysis from studies from Australia, Sweden, United Kingdom and the United States. Mult Scler 21:92–100
Hearn A, Silber E (2010) Osteoporosis in multiple sclerosis. Mult Scler 16:1031–1043
Marrie R, Cutter G, Tyry T, Vollmer T (2009) A cross-sectional study of bone health in multiple sclerosis. Neurology 73:1394–1398
Ayrignac X, Larochelle C, Keezer M, Roger E, Poirier J et al (2021) Frailty in ageing persons with multiple sclerosis. Mult Scler 27:613–620
Dong G, Zhang N, Wu Z, Liu Y, Wang L (2015) Multiple Sclerosis Increases Fracture Risk: A Meta-Analysis. Biomed Res Int 2015:650138
Schett G, David J (2010) The multiple faces of autoimmune-mediated bone loss. Nat Rev Endocrinol 6:698–706
Formica C, Cosman F, Nieves J, Herbert J, Lindsay R (1997) Reduced bone mass and fat-free mass in women with multiple sclerosis: effects of ambulatory status and glucocorticoid Use. Calcif Tissue Int 61:129–133
Josyula S, Mehta B, Karmon Y, Teter B, Batista S et al (2012) The nervous system’s potential role in multiple sclerosis associated bone loss. J Neurol Sci 319:8–14
Dovio A, Perazzolo L, Osella G, Ventura M, Termine A et al (2004) Immediate fall of bone formation and transient increase of bone resorption in the course of high-dose, short-term glucocorticoid therapy in young patients with multiple sclerosis. J Clin Endocrinol Metab 89:4923–4928
Moen S, Celius E, Sandvik L, Nordsletten L, Eriksen E, Holmøy T (2011) Low bone mass in newly diagnosed multiple sclerosis and clinically isolated syndrome. Neurology 77:151–157
Bulik-Sullivan BK, Loh P-R, Finucane HK, Ripke S, Yang J et al (2015) LD Score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat Genet 47:291–295
Zheng J, Erzurumluoglu AM, Elsworth BL, Kemp JP, Howe L et al (2017) LD Hub: a centralized database and web interface to perform LD score regression that maximizes the potential of summary level GWAS data for SNP heritability and genetic correlation analysis. Bioinformatics 33:272–279
Altshuler DM, Gibbs RA, Peltonen L, Altshuler DM, Gibbs RA et al (2010) Integrating common and rare genetic variation in diverse human populations. Nature 467:52–58
International Multiple Sclerosis Genetics Consortium. Multiple sclerosis genomic map implicates peripheral immune cells and microglia in susceptibility. Science. 2019;365(1095–9203 (Electronic)).
Smith G, Ebrahim S (2003) ‘Mendelian randomization’: can genetic epidemiology contribute to understanding environmental determinants of disease? Int J Epidemiol 32:1–22
Evans D, Smith G (2015) Mendelian Randomization: New Applications in the Coming Age of Hypothesis-Free Causality. Annu Rev Genomics Hum Genet 16:327–350
Li G, Thabane L, Papaioannou A, Ioannidis G, Levine M, Adachi J (2017) An overview of osteoporosis and frailty in the elderly. BMC Musculoskelet Disord 18:017–1403
Kemp J, Morris J, Medina-Gomez C, Forgetta V, Warrington N et al (2017) Identification of 153 new loci associated with heel bone mineral density and functional involvement of GPC6 in osteoporosis. Nat Genet 49:1468–1475
Taekema DG, Gussekloo J, Maier AB, Westendorp RGJ, Craen AJMd. Handgrip strength as a predictor of functional, psychological and social health. A prospective population-based study among the oldest old. Age and Ageing. 2010;39(3):331–7.
Hanwell H, Banwell B (2011) Assessment of evidence for a protective role of vitamin D in multiple sclerosis. Biochim Biophys Acta 1812:202–212
Burgess S, Thompson S (2015) Multivariable Mendelian randomization: the use of pleiotropic genetic variants to estimate causal effects. Am J Epidemiol 181:251–260
Evans D, Davey SG (2015) Mendelian Randomization: New Applications in the Coming Age of Hypothesis-Free Causality. Annu Rev Genomics Hum Genet 16:327–350
Greco MF, Minelli C, Sheehan N, Thompson J (2015) Detecting pleiotropy in Mendelian randomisation studies with summary data and a continuous outcome. Stat Med 34:2926–2940
Davey Smith G, Hemani G (2014) Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet 23:4
Verbanck M, Chen C-Y, Neale B, Do R (2018) Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 50:693–698
Burgess S, Thompson S (2017) Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol 32:377–389
TwoSampleMR 0.5.6: Mendelian randomization with GWAS summary data [Available from: https://mrcieu.github.io/TwoSampleMR/.
MendelianRandomization: Mendelian Randomization Package [Available from: https://cran.r-project.org/web/packages/MendelianRandomization/MendelianRandomization.pdf.
Verbanck M, Chen C-Y, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nature Genetics. 2016;2022.
Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife. 2018;7:e34408.
Hemani G, Zheng J, Wade KH, Laurin C, Elsworth B, Burgess S, et al. The MR-Base platform supports systematic causal inference across the human phenome. eLife 2018. doi: https://doi.org/10.7554/eLife.34408. eLife. 2018.
Giambartolomei C, Vukcevic D, Schadt EE, Franke L, Hingorani AD, Wallace C, et al. Bayesian Test for Colocalisation between Pairs of Genetic Association Studies Using Summary Statistics. PloS Genetics. 2014.
Foley CN, Staley JR, Breen PG, Sun BB, Kirk PDW et al (2021) A fast and efficient colocalization algorithm for identifying shared genetic risk factors across multiple traits. Nat Commun 12:764
Wallace C. Eliciting priors and relaxing the single causal variant assumption in colocalisation analyses. PloS Genetics. 2020.
Bazelier M, van Staa T, Uitdehaag B, Cooper C, Leufkens H et al (2011) The risk of fracture in patients with multiple sclerosis: the UK general practice research database. J Bone Miner Res 26:2271–2279
Mazumder R, Murchison C, Bourdette D, Cameron M. Falls in people with multiple sclerosis compared with falls in healthy controls. PLoS One. 2014;9.
Bazelier MT, Staa T-Pv, Uitdehaag BMJ, Cooper C, Leufkens HGM, Vestergaard P, et al. Risk of fractures in patients with multiple sclerosis A population-based cohort study. Neurology. 2012;78:1967–73.
Bazelier MT, Staa Tv, Uitdehaag BM, Cooper C, Leufkens HG, Vestergaard P, et al. The risk of fracture in patients with multiple sclerosis: The UK general practice research. Journal of Bone and Mineral Research. 2011;26:2271–2279.
Trajanoska K, Seppala LJ, Medina-Gomez C, Hsu Y-H, Zhou S, van Schoor NM, et al. Genetic basis of falling risk susceptibility in the UK Biobank Study. Communications Biology. 2020;3.
Acknowledgements
This study was funded by NIH grant (R01AR72199). The funders had no role in study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Funding
NIH,R01AR72199,Yi-Hsiang Hsu
Author information
Authors and Affiliations
Contributions
SJ: Data Analysis, Interpretation of results, Draft and revision of manuscript. MJT: Interpretation of results, Revision of manuscript. CS: Interpretation of results, Revision of manuscript. YHH: Conceptualization, Data acquisition, Interpretation of results, Revision of manuscript, Funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest.
Ethical approval
This is a study with secondary data analyses. All of the analyses were done with “summary statistics”, and no individual-level data was used. In addiiton, we solely used publicly available (freely downloadable) GWAS summary statistics, which neither require institutional ethics committee approval nor informed consent from the study populations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Jeong, S., Tsai, MJ., Shen, C. et al. Falls, fracture and frailty risk in multiple sclerosis: a Mendelian Randomization study to identify shared genetics. J Bone Miner Metab 42, 335–343 (2024). https://doi.org/10.1007/s00774-024-01504-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-024-01504-8