Abstract
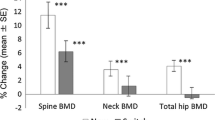
We explored the relationship between plasma total homocysteine concentration and osteoporosis in postmenopausal patients with type 2 diabetes. Postmenopausal patients with type 2 diabetes (n = 258) were enrolled in a cross-sectional hospital-based study. Osteoporosis was documented by dual energy X-ray absorptiometry. Plasma total homocysteine concentration was measured using fluorescence polarization immunoassay. Risk factors for osteoporosis and determinants of homocysteine were obtained from blood samples and interviewer questionnaire. We found that plasma total homocysteine levels were higher in subjects with osteoporosis and diabetes than without [(9.5 ± 2.0) vs. (10.4 ± 2.4) μmol/l, p = 0.001]. The association of homocysteine with osteoporosis was independent of possible risk factors for osteoporosis in diabetes (e.g., duration of diabetes, HbA1c, body mass index, serum 25-hydroxyvitamin D, thiazolidinediones, and retinopathy) and determinants of homocysteine concentration (age, serum folate and vitamin B12, renal status, and biguanide use) [OR 1.40 (1.02–1.90), p = 0.036]. In addition, bone mineral density was closely correlated with homocysteine as a continuous variable after adjusting for age [r = −0.64 (−0.69 to −0.58), p = 0.002]. Furthermore, per increase of 5.0 μmol/l, plasma homocysteine was related to osteoporosis, after controlling for per unit increase of other factors [OR 1.42 (1.07–1.96), p = 0.027]. The optimal cut-off point for the plasma homocysteine level distinguishing diabetic patients with osteoporosis from without was 10.18 μmol/l. The results suggest that plasma total homocysteine concentration is independently associated with the occurrence of osteoporosis in postmenopausal patients with type 2 diabetes. Future prospective studies are warranted to clarify the relationship.
Similar content being viewed by others
References
Yang W, Lu J, Weng J, Jia W, Ji L, Xiao J, China National Diabetes and Metabolic Disorders Study Group (2010) Prevalence of diabetes among men and women in China. N Engl J Med 362:1090–1101
Tyagi N, Vacek TP, Fleming JT, Vacek JC, Tyagi SC (2011) Hyperhomocysteinemia decreases bone blood flow. Vasc Health Risk Manag 7:31–35
Starkebaum G, Harlan JM (1986) Endothelial cell injury due to copper-oxidized hydrogen peroxide generation from homocysteine. Clin Invest 77:1370–1376
Stamler JS, Osborne JA, Jaraki O, Rabbani LE, Mullins M, Singel D (1993) Adverse vascular effects of homocysteine are modulated by endothelial-derived relaxing factor and related oxides of nitrogen. Clin Invest 91:308–318
Abdella NA, Mojiminiyi OA, Akanji AO, Moussa MA (2002) Associations of plasma homocysteine concentration in subjects with type 2 diabetes mellitus. Acta Diabetol 39:183–190
Jacques PF, Bostom AG, Wilson PW, Rich S, Rosenberg IH, Selhub J (2001) Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort. Am J Clin Nutr 73:613–621
Chico A, Perez A, Cordoba A, Arcelus R, Carreras G, de Leiva A (1998) Plasma homocysteine is related to albumin excretion rate in patients with diabetes mellitus: a new link between diabetic nephropathy and cardiovascular disease? Diabetologia 41:684–693
Mudd SH, Pool JR (1975) Labile methyl balance for normal humans on various dietary regimens. Metabolism 24:721–733
Baines M, Kredan MB, Usher J, Davison A, Higgins G, Taylor W (2007) The association of homocysteine and its determinants: MTHFR genotype, folate, vitamin B12 and vitamin B6 with bone mineral density in postmenopausal British women. Bone 40:730–736
Ganji V, Kafai MR (2009) Demographic, lifestyle, and health characteristics and serum B vitamin status are determinants of plasma total homocysteine concentration in the post-folic acid fortification period, 1999–2004. J Nutr 139:345–352
Isidro ML, Ruano B (2010) Bone disease in diabetes. Curr Diabetes Rev 6:144–155
Viégas M, Costa C, Lopes A, Griz L, Medeiro MA, Bandeira F (2011) Prevalence of osteoporosis and vertebral fractures in postmenopausal women with type 2 diabetes mellitus and their relationship with duration of the disease and chronic complications. J Diabetes Complicat 25:216–221
WHO: World Health Organization (2006) Diabetes mellitus: report of a WHO Study Group. World Health Org, Geneva
WHO: World Health Organization (2003) Prevention and management of osteoporosis. World Health Organ Tech Rep Ser 921:1–164
Chinese Nutrition Society (2008) Chinese dietary guidelines. Tibet People’s Publishing Company Press, China
Leboff MS, Narweker R, LaCroix A, Wu L, Jackson R, Lee J (2009) Homocysteine levels and risk of hip fracture in postmenopausal women. J Clin Endocrinol Metab 94:1207–1213
Refsum H, Smith AD, Ueland PM, Nexo E, Clarke R, McPartlin J (2004) Facts and recommendations about total homocysteine determinations: an expert opinion. Clin Chem 50:1482–1483
Hao L, Ma J, Zhu J, Stampfer MJ, Tian Y, Willett WC (2007) Vitamin B-12 deficiency is prevalent in 35- to 64-year-old Chinese adults. J Nutr 137:1278–1285
Bonassi MR, Chada BE, Eduardo FC, Marcelo LE, Rodrigues DLG (2007) Effects of estrogen and estrogen-progestogen therapy on homocysteine levels and their correlation with carotid vascular resistance. Gynecol Endocrinol 23:619–624
Viégas M, Costa C, Lopes A, Griz L, Medeiro MA, Bandeira F (2011) Prevalence of osteoporosis and vertebral fractures in postmenopausal women with type 2 diabetes mellitus and their relationship with duration of the disease and chronic complications. J Diabetes Complicat 25:216–221
Kuyumcu ME, Yesil Y, Oztürk ZA, Cınar E, Kızılarslanoglu C, Halil M (2012) The association between homocysteine (hcy) and serum natural antioxidants in elderly bone mineral densitometry (BMD). Arch Gerontol Geriatr 55:739–743
Robert RM, Paul FJ, Jacob S, Katherine LT, Elizabeth JS, Kerry EB (2004) Homocysteine as a predictive factor for hip fracture in older persons. N Engl J Med 350:2042–2049
Yamamoto M, Yamaguchi T, Yamauchi M, Sugimoto T (2009) Low serum level of the endogenous secretory receptor for advanced glycation end products (esRAGE) is a risk factor for prevalent vertebral fractures independent of bone mineral density in patients with type 2 diabetes. Diabetes Care 32:2263–2268
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Eng J Med 359:1577–1589
Hong XM, Hsu YH, Henry TD, Tang GF, Liu X (2007) Association of the methylenetetrahydrofolate reductase C677T polymorphism and fracture risk in Chinese postmenopausal women. Bone 40:737–742
Li JB, Wang CY, Chen JW, Feng ZQ, Ma HT (2004) Expression of liver IGF-1 gene and its serum IGF-1 level in rats with diabetes. World J Gastroenterol 10:255–259
Raisz LG (2005) Pathogenesis of osteoporosis concepts, conflicts, and prospects. J Clin Invest 115:3318–3325
Mao R, Fan Y, Chen F, Fu S (2008) Genetic polymorphism of MTHFR G1793A in Chinese populations. Eur J Epidemiol 23:363–368
Chan E, Fonseca VA (2003) Management of hyperhomocysteinemia. Metab Syndr Relat Disord 1:159–170
House AA, Eliasziw M, Cattran DC, Churchill DN, Oliver MJ, Fine A (2010) Effect of B-vitamin therapy on progression of diabetic nephropathy: a randomized controlled trial. JAMA 303:1603–1609
Li JB, Wang CY, Chen JW, Li XL, Feng ZQ, Ma HT (2010) The preventive efficacy of methylcobalamin on rat peripheral neuropathy influenced by diabetes via neural IGF-1 levels. Nutr Neurosci 13:79–86
Acknowledgments
We would like to thank National Natural Science Foundation (81070655) of China and Jiangsu Provincial Natural Science Foundation (BK2009441) of China for supporting this project. This work would not have been possible without the funding.
Conflict of interest
All authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Jianbo, L., Zhang, H., Yan, L. et al. Homocysteine, an additional factor, is linked to osteoporosis in postmenopausal women with type 2 diabetes. J Bone Miner Metab 32, 718–724 (2014). https://doi.org/10.1007/s00774-013-0548-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-013-0548-4