Abstract
To test the hypothesis that 1 week of combined sleep and light interventions (SALI), which phase-advance (shift earlier) melatonin circadian rhythms, improves mood significantly more than phase-delay (shift later) SALI. After a 2-month diagnostic evaluation for premenstrual dysphoric disorder (PMDD per DSM-5 criteria) in a university clinical research setting, 44 participants enrolled in baseline studies were randomized in the luteal phase at home to (A) a phase-advance intervention (PAI): 1 night of late-night wake therapy (LWT: sleep 9 pm–1 am) followed by 7 days of the morning (AM) bright white light (BWL), or (B) a phase-delay intervention (PDI): 1 night of early-night wake therapy (EWT: sleep 3–7 am) plus 7 days of the evening (PM) BWL. After a month of no intervention, participants underwent the alternate intervention. Outcome measures were mood, the melatonin metabolite, 6-sulfatoxymelatonin (6-SMT), and actigraphy (to assess protocol compliance). At baseline, atypical depression correlated positively with phase delay in 6-SMT offset time (r = .456, p = .038). PAI advanced 6-SMT offset from baseline more than PDI (p < .05), and improved raw mood scores more than PDI (p < .05). As hypothesized, percent improvement in mood correlated positively with a phase advance from baseline in 6-SMT offset time (p < .001). Treatment with 1 night of advanced/restricted sleep followed by 7 days of AM BWL (PAI) was more efficacious in reducing PMDD depression symptoms than a PDI; mood improvement occurred in association with phase advance in 6-SMT offset time. Combined SALIs offer safe, efficacious, rapid-acting, well-tolerated, non-pharmacological, non-hormonal, affordable, repeatable home interventions for PMDD. Clinical Trials.gov NCT # NCT01799733.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A potentially disabling condition, premenstrual dysphoric disorder (PMDD) causes extensive personal suffering, occupational impairment, and disruption of interpersonal and family relationships. While 20–80% of women report mood, cognitive, and behavioral disturbances associated with their menstrual cycle (Hamilton et al. 1984; Parry and Wehr 1987), PMDD can progress from premenstrual syndrome (PMS) to major depression (MD) (Halbreich and Endicott 1985; Hamilton et al. 1984), increase risks for peripartum and menopausal depression (Parry et al. 1995), and exacerbate bipolar illness (Dias et al. 2011; Payne 2011). Premenstrual mood symptoms meet criteria for a mental disorder in 5–8% of menstruating women (Accortt et al. 2008; American Psychiatric Association 2013; Yonkers et al. 2008). Current PMDD treatments are only marginally efficacious (< 60% response) (Halbreich et al. 2006), and many women do not want to use, or cannot tolerate, taking chronic antidepressant medications for a periodic illness. Pharmacological interventions are not efficacious in over 40% of women (Halbreich et al. 2006), are associated with problematic side effects, increase the risk of breast and ovarian cancer (Cosgrove et al. 2011), and do not improve health outcomes (Borenstein et al. 2007). Consequently, enhanced PMDD treatments are needed (Borenstein et al. 2007).
A single night of total or partial “wake therapy” (WT) (previously called therapeutic sleep deprivation) produces a rapid, albeit transient, antidepressant response in 40–60% of patients (Giedke and Schwarzler 2002; Schilgen and Tolle 1980; Wirz-Justice and Van den Hoofdakker 1999; Wirz-Justice and Terman 2012; Wirz-Justice et al. 2013; Wu and Bunney 1990). Early-night wake therapy (EWT: i.e., remaining awake until 3:00 am, then sleeping from 3:00–7:00 am), or late-night wake therapy (LWT: i.e., sleeping from 9:00 pm–01:00 am and remaining awake until the following night), benefits mood as much as “total-night” WT (Leibenluft and Wehr 1992; Parry and Wehr 1987; Wirz-Justice et al., 2013). LWT is more efficacious than EWT in some, but not all, MDs (Parry and Wehr 1987; Wirz-Justice et al. 2013). We confirmed wake therapy efficacy in PMDD (Parry and Wehr 1987; Parry 1995) and peripartum depression (Parry et al. 2000, 2019).
Light treatment sustains wake therapy benefits often lost after recovery sleep, and wake therapy hastens and potentiates light treatment effects taking 5–10 weeks to significantly improve mood in peripartum non-seasonal depression (Corral et al. 2000, 2007; Epperson et al. 2004; Oren et al. 2002; Wirz-Justice et al. 2011). We previously reported and replicated the independent antidepressant effects of light (Parry et al. 1989; 1993; 1997a) and wake therapy (Parry and Wehr, 1987; Parry et al. 1995) in PMDD. AM light significantly improved scores on the Hamilton Rating Scale for Depression (HRSD) by 50% (Parry et al. 1997a), replicated using a shorter, brighter light pulse (Parry et al. 2011). LWT significantly reduced mean HRSD depression scores by 62.2% (Parry et al. 1995). In the current study, we combined wake and light interventions to enhance their individual benefits.
As misaligned circadian rhythms characterize mood disorders (Goel et al. 2013; Monteleone et al. 2011; Srinivasan et al. 2006; Wehr and Wirz-Justice 1982), we sought to test the hypothesis that wake and light interventions exert antidepressant effects by correcting misaligned circadian rhythms (CRs), best measured by melatonin in humans. In PMDD, we previously found plasma melatonin CR were phase delayed (shifted later) in the symptomatic luteal, compared with the asymptomatic follicular, menstrual cycle phase, which correlated with more depressed mood (Parry et al. 1997b, 2008a). Consistent with the internal coincidence model of sleep deprivation and depression (Wehr and Wirz-Justice 1981), baseline timing disturbances between sleep and melatonin became normalized after treatment (Parry et al. 1989, 1997a, 1999). We reasoned that advancing and restricting sleep with 1 night of LWT followed by 7 days of the morning (AM) bright white light (BWL), which phase advances CRs (active intervention), would benefit mood more than delaying and restricting sleep with a single night of EWT followed by 7 days of the evening (PM) BWL, which phase delays CRs (control intervention).
Methods
Overview
We described the essential features of our protocol including screening, eligibility, inclusion, and exclusion criteria previously (Parry et al. 1995, 1997a,b, 2008a). In the present study, we used a randomized-order, crossover design, studying NC and PMDD women during luteal phases of two separate menstrual cycles. Using a “crossover” design, we tested each participant twice, with two contrasting interventions separated by 1 month. For the first intervention, half the subjects were assigned to a phase advance intervention (PAI): (1) A partial night (4 h) of phase-advancing sleep (sleep 9 pm–1 am, followed by wakefulness), followed by 7 consecutive mornings of AM BWL (light-emitting diode-LED administered for 60 min) within 30 min after wake time; or (2) a phase delay intervention (PDI): A partial night (4 h) of phase-delaying sleep (remain awake until 3 am, then sleep 3–7 am), followed by 7 consecutive evenings of PM BWL (administered for 60 min), starting 90 min before anticipated sleep onset. See Fig. 1. We assessed intervention effects on (1) the urinary melatonin metabolite, 6-sulfatoxymelatonin (6-SMT); (2) mood; and (3) sleep/activity (actigraphy, to confirm protocol compliance). We tested the following hypotheses (H):
Study flow: Luteinizing hormone surge (LHS) marks ovulation. Women begin actigraphy recordings on LHS for 10 days on menstrual cycle days (CD) 14–24. In months 2, 3, and 5, beginning on CD 14, women collect urine samples for 6-sulphatoxymelatonin (6-SMT) for 36 h over 2 nights between 8 and 9 days after the LHS (c. CD 22–23). They undergo phase-advance sleep (PAS) or phase-delay sleep (PDS) at home on the night of the LHS, and receive bright morning (AM) or bright evening (PM) light on days 1–7 after LHS (CD 15–21) in a counterbalanced, cross-over design in months 3 and 5. Mood ratings (Structured Interview Guide for the Hamilton Rating Scale for Depression (HRSD) with Atypical Depression supplement-SIGH-ADS) are obtained as follows: months 1 and 2—once per week; months 3 and 5—LHS (Pre-PAI/PDI), daily LHS + 1 day → LHS + 2 days, and once during the evening after last treatment day (LHS + 7/8 days). Blind raters assessed mood by the SIGH-ADS once during month 4 and once a month after intervention 2 for 3 months to clinically monitor relapse
-
H1.
PAI vs. PDI will normalize melatonin circadian rhythms in PMDD by phase-advancing urinary melatonin timing measures (i.e., 6-SMT offset time).
-
H2.
PAI will improve mood more than PDI.
-
H3.
Mood improvement will correlate positively with the magnitude of phase-advance in 6-SMT offset time after PAI.
Statistical analyses
For inferential tests of H1 and H2, we used a 2 × 2, within subjects/repeated measures Analyses of Variance to compare the effects of PAI vs. PDI on PMDD mood, 6-SMT timing, and sleep measures, before and after interventions. For H3, we evaluated the relationships of changes in mood and sleep to changes in 6-SMT timing using Pearson correlations.
Procedures
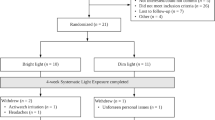
We received 688 calls from women interested in participating. We screened 368 via telephone and scheduled 137 for screening visits. A total of 85 women enrolled in the screening phase and 44 (29 PMDD + 15 NC) were randomized to intervention from 5/1/13 to 4/30/18. Of these, 15 PMDD and 8 NC completed the entire protocol and two participants completed at least one intervention arm.
The University of California San Diego Institutional Review Board approved the protocol, and all participants gave written informed consent after procedures were explained fully. Participants were without alcohol abuse, significant medical illness, or medication that would interfere with study measures.
To establish DSM-IV-TR (APA, 2000) entrance and baseline criteria, trained clinicians used the Structured Clinical Interview for DSM-IV (SCID) (First et al.1995) and assessed pre- and post-treatment mood (see Fig. 1 legend) with the Structured Interview Guide for the Hamilton Rating Scale for Depression (HRSD) with Atypical Depression supplement (SIGH-ADS) (Williams and Terman 2003); participants completed 2 months of daily mood ratings in which, for study inclusion, PMDD participants were required to be asymptomatic during the follicular menstrual cycle phase, and demonstrate a 30% increase in symptoms in the luteal phase. From the pool of volunteers, we obtained mood data on PMDD and essentially asymptomatic, normal control (NC) women. We excluded patients with substance use, bipolar, and primary anxiety disorders.
Documenting sleep time
We documented compliance with sleep and wake protocol requirements by actigraphy and by requiring participants to telephone the laboratory every 30 min while awake between 9 pm and 7 am.
Light Box
Subjects sat before a portable (5.5″ × 6.25″) Litebook® light box (an array of 60 cool white light-emitting diodes behind a clear plastic screen with an intensity of 1350 lx and an irradiance of 2.41 × 10−9 w/cm2 at a distance of 21 in, and spectral emission peaks at 464 nm and 564 nm) (The Litebook Company Ltd., Alberta, Canada) for 60 min. Participants did not stare directly at the light source as it could cause discomfort, but is not harmful. The distance of the subject from the light source was calibrated individually for each light box using a Meterman LM631 Digital Light Meter (Meterman Test Tools, Everett, WA) to ensure an intensity of 1350 lx at 21 in. We provided a measuring tape to ensure the proper distance between the light source and the subject. Ambient light intensity and spectra were documented by the Actiwatch Spectrum.
Dependent Measures
For a complete description of 6-SMT and actigraphy measures, please see Supplementary Online Resource for Archives of Women’s Mental Health.
Results
Baseline demographic characteristics of study participants are reported in Table 1.
Protocol deviation
Some PMDD participants (9 of 24) deviated from the design protocol by not self-administering morning light during the active PAI (LWT + AM BWL) portion of the study. A comparison of improvements (percent changes) from baseline mood measures in those who fully complied (N = 15) vs. those who did not (N = 9) showed women who self-administered morning light per protocol experienced significantly greater improvements (percent reductions from baseline) in HRSD (71.5 vs. 42.5%, p = 0.001), atypical (83.0 vs. 48.0%, p = 0.003), and SIGH-ADS (76.2 vs. 48.0%, p = 0.002) scores. Thus, as expected, adding bright white light exposure for 1 week after wake therapy increased mood benefits significantly beyond those achieved with wake therapy alone. (The remainder of this report focuses entirely on outcomes of the 15 women who complied with both wake + light interventions.)
At baseline, the cosine-derived 6-SMT offset was significantly correlated with the atypical mood score of the SIGH-ADS in PMDD + NC combined (r = + 0.456, p = 0.038; see Fig. 2); i.e., greater phase-delay in 6-SMT offset was associated with greater atypical depressed mood (e.g., symptoms of increased appetite, weight gain, sleepiness, and fatigue).
PAI vs. PDI effects on 6-SMT timing
Post-intervention, MANOVA showed the PAI advanced 6-SMT timing from baseline more than PDI (F(3,18) = 4.04, p = 0.023 for trend). Simple effects analysis showed, as hypothesized (H1), advance in 6-SMT offset was significantly greater after PAI vs. PDI (mean + / − SD = + 0.84 + / − 1.36 vs. + 0.28 + / − 2.35 h, p < 0.001). Post-intervention changes in 6-SMT onset and acrophase did not differ significantly (p > 0.05).
Mood Effects of PAI vs. PD
Both PAI and PDI improved objective, interview-assessed depression; however, as hypothesized, PAI improved mood significantly more than PDI on HRSD, atypical, and SIGH-ADS indices (see Fig. 3.)
Percent change (improvement from baseline) in mood measures was significantly greater after phase-advance intervention (PAI) vs. phase-delay intervention (PDI) for Hamilton Rating Scale for Depression (HRSD), Atypical, and Structured Interview Guide for the Hamilton Rating Scale for Depression (HRSD) with Atypical Depression supplement (SIGH-ADS) scores (all p < .05)
Relationship of mood change to 6-SMT change
The mean percent change from baseline was significantly greater after PAI (the active condition) vs. PDI (control condition) for atypical mood (88.95 + / − 17.1 vs. 58.49 + / − 43.6%, p = 0.028%) and SIGH-ADS score (75.77 + / − 17.8 vs. 63.61 + / − 21%, p = 0.025). Furthermore, as hypothesized (H3), advance in 6-SMT offset time after PAI was positively correlated with the magnitude of improvement in HRSD score (r = + 0.815, p = 0.001) and SIGH-ADS score (r = + 0.695, p = 0.008). Thus, greater mood improvement after PAI was associated with greater phase advance in 6-SMT offset time (see Fig. 4A, B). In contrast, after the PDI, the change in 6-SMT offset did not correlate significantly with improvement in HRSD, atypical, or SIGH-ADS score (all p > 0.05).
Advance in 6-sulfatoxymelatonin (6-SMT) offset time after phase-advance intervention (PAI) correlated positively with magnitude of improvement in A Hamilton Rating Scale for Depression (HRSD) (r = + .815, p = .001) and B the Structured Interview Guide for the Hamilton Rating Scale for Depression (HRSD) with atypical depression supplement (SIGH-ADS) score (r = + 0.695, p = .008)
Sleep effects of PAI vs. PDI.
Neither PAI nor PDI produced significant changes from baseline in sleep parameters (timing of sleep onset, offset, mid-sleep, or total sleep time); nor were any sleep changes significantly correlated with mood or 6-SMT changes.
Discussion
The aim of this study was to determine whether PMDD depressed mood could be improved using phase-advancing sleep and light intervention (SALI) to correct the phase delay in melatonin circadian rhythms (CR) we found in PMDD (Parry et al. 1997a, 2008a). We hypothesized that since estradiol advances, and progesterone delays CR (Albers et al. 1981; Morin et al. 1977), fluctuations in these hormones during the menstrual cycle could dysregulate CR, and correcting CR misalignment could thereby improve depressed mood. In support of this hypothesis, we found the following: (1) In the baseline luteal phase, PMDD atypical depression symptoms were associated with a greater phase delay of 6-SMT offset; (2) A phase-advance intervention (PAI: late-night wake therapy-LWT plus AM bright white light-BWL) produced significantly greater mood improvement than a phase-delay intervention (PDI: early-wake therapy-EWT plus PM BWL); and (3) After PAI, improvement in HRSD and SIGH-ADS mood scores correlated significantly with phase advance in 6-SMT offset.
Importantly, we designed the study arms to create identical sleep restriction durations (4 h), plus identical bright light exposures (60 min/day for 7 days), but at different times of day, to effect maximal CR realignment. Thus, the treatments varied only in the times of day when sleep restriction and light exposure were instituted, with PAI designed to advance 6-SMT timing vs. PDI. That mood benefits and 6-SMT phase-advanced timing were, indeed, significantly correlated in the PAI vs. PDI study arms confirmed that hypothesis.
We discuss implications of these findings in relation to previous literature below.
-
1.
Phase delay in CRs characterizes other depressive disorders. Lewy et al. (2006) reported phase-delayed melatonin CR in seasonal affective disorder; we found phase-delayed plasma melatonin CR in postpartum and menopausal depressed participants (Parry et al. 2008b, c); and Tuunainen et al. (2002) found phase-delayed 6-SMT rhythms in post-menopausal depression. Phase-delayed CR, or delayed chronotype, also were associated with later sleep onset times in peri- and post-menopausal women (Meliska et al. 2011). One possible explanation is that later sleep onset times and chronotypes reflect later wake times, which prevents CR synchronization from morning bright light. The resulting misalignment of CR then contributes to depressive mood, according to the internal coincidence model of sleep and depression (Wehr and Wirz-Justice 1981). Under the influence of progesterone in the luteal phase, both PMDD and normal control women delay melatonin CR in the luteal vs. follicular menstrual cycle phase; but only PMDD women experience mood symptoms then (Parry et al. 2008a), suggesting that individuals with depressive histories are more vulnerable to developing symptoms during acute phase shifts, as occurs in jet lag (Parry 2002). That symptoms remit in the early follicular phase when phase-advancing estradiol increases and phase-delaying progesterone decreases (as with sleep and light interventions that restore a CR phase advance in the luteal phase), suggests CR abnormalities in PMDD are more state, than trait, dependent. Also, noteworthy is that baseline phase-delayed CR were associated with atypical symptoms that characterize depressions associated with the reproductive cycle and seasonal affective disorder (Parry et al. 1987). These symptoms are particularly responsive to light therapy (Terman et al. 1989).
-
2.
That the PAI, a phase-advancing SALI, reduced depression scores significantly more than the PDI, a phase-delaying SALI, confirms the hypothesis that phase-advancing CR is particularly effective in reducing PMDD depressed mood. Mood improvement after light treatment has been associated with a corrective phase shift of melatonin CRs in other depressive disorders: by Epperson et al. (2004) with bright light therapy for antepartum depression; by Terman et al. (2001) in winter depression; with the activity rhythm in unipolar depression (Dallaspezia et al. 2012); and in other mood disorders (Benedetti et al. 2005; Bloching et al. 2000; Colombo et al. 2000; Even et al. 2008; Fritzsche et al. 2001; Golden et al. 2005; Kripke et al. 1983; Loving et al. 2002; Neumeister et al. 1996; Parry and Maurer 2003; Riemann et al. 1999; Sokolski et al. 1995; Tuunainen et al. 2004; van den Burg et al. 1990; Wehr et al. 1985; Wu et al. 2009), thereby potentially providing new approaches to investigate and treat PMDD.
-
3.
The correlation of mood improvement magnitude with 6-SMT phase advance after PAI suggests the intervention engages a relevant pathogenesis: phase-delayed melatonin in the luteal menstrual cycle phase.
These results suggest potential benefits for other reproductively related mood disorders when a circadian pathophysiology is identified. For example, in pregnancy, we showed plasma and urinary melatonin were phase advanced in depressed vs. healthy participants (Parry et al. 2008b), and mood improved significantly more after phase-delaying than phase-advancing SALI. In contrast, in postpartum-depressed participants plasma and urinary melatonin were phase delayed (Parry et al. 2008b), and mood improved more after phase-advancing than phase-delaying SALI. In menopausal, like postpartum-depressed participants, plasma and urinary melatonin were phase delayed (Parry et al. 2008c), and mood improved more after phase-advancing vs. phase-delaying SALI. Thus, each reproductively related depressive disorder has a specific chronobiological abnormality that provides a basis for optimizing interventions targeted to specific pathogenic mechanisms.
The advantage of combining sleep and light interventions is that the sleep intervention hastens and potentiates mood benefits of light treatment, and light treatment maintains mood benefits of sleep intervention, which otherwise may be lost after a night of recovery sleep (Wirz-Justice 2011). Initially, we used the sleep intervention alone in PMDD (Parry and Wehr 1987; Parry et al. 1995) where, in contrast to other mood disorders, women with PMDD did not relapse after a night of recovery sleep; i.e., they were more night 2, rather than night 1, responders, which may indicate a more serotonergic, rather than noradrenergic, pathophysiology, supported by extensive studies (see review Parry 2001). As light treatment alone in non-seasonal depression may require at least 5 weeks to improve mood significantly (Parry and Maurer 2003), light treatment, without the priming effect of wake therapy, is less efficacious for PMDD when administered during the necessarily limited time period of 7 days in the symptomatic late luteal phase (Parry et al. 1989, 1993). The advantage of combining interventions is that sleep interventions may produce rapid improvements, which are subsequently sustained by light interventions.
These sleep and light interventions are safe, efficacious, rapid-acting, affordable, readily repeatable, well-tolerated with few side effects, non-pharmacological and non-hormonal home treatments that can be administered by paraprofessionals without office or clinic visits.
Study limitations include a relatively small sample size, from only a single study site, and melatonin measured by 6-SMT rather than plasma. Further, as 37.5% of participants did not complete the full protocol, we confined conclusions about primary study outcomes to results of only participants who completed the full protocol. Although in our earlier study of wake therapy (Parry et al. 1995), the duration of benefit lasted up to 6 months, the durability of sleep + light benefits in the present study needs to be tested.
References
Accortt EE, Freeman MP, Allen JJ (2008) Women and major depressive disorder: clinical perspectives on causal pathways. J Womens Health (larchmt) 17(10):1583–1590. https://doi.org/10.1089/jwh.2007.0592
Albers HE, Gerall AA, Axelson JF (1981) Effect of reproductive state on circadian periodicity in the rat. Physiol Behav 26(1):21–25
American Psychiatric Association (2013) American Psychiatric Association. DSM-5: Diagnostic and Statistical Manual of Mental Disorders, 5th edn. APA
APA (2000) Diagnostic and Statistical Manual of Mental Disorders - Fourth Edition - Text Revision (DSM-IV-TR), 4th edn. American Psychiatric Association
Benedetti F, Barbini B, Fulgosi MC, Colombo C, Dallaspezia S, Pontiggia A, Smeraldi E (2005) Combined total sleep deprivation and light therapy in the treatment of drug-resistant bipolar depression: acute response and long-term remission rates. J Clin Psychiatry 66(12):1535–1540
Bloching B, Dechene C, Taschner KL (2000) Outlasting antidepressant effect of late partial sleep deprivation by bright light therapy. J Sleep Res 9:21
Borenstein JE, Dean BB, Leifke E, Korner P, Yonkers KA (2007) Differences in symptom scores and health outcomes in premenstrual syndrome. J Womens Health (larchmt) 16(8):1139–1144. https://doi.org/10.1089/jwh.2006.0230
Colombo C, Lucca A, Benedetti F, Barbini B, Campori E, Smeraldi E (2000) Total sleep deprivation combined with lithium and light therapy in the treatment of bipolar depression: replication of main effects and interaction. Psychiatry Res 95(1):43–53
Corral M, Kuan A, Kostaras D (2000) Bright light therapy’s effect on postpartum depression. Am J Psychiatry 157(2):303–304
Corral M, Wardrop AA, Zhang H, Grewal AK, Patton S (2007) Morning light therapy for postpartum depression. Arch Womens Ment Health 10(5):221–224. https://doi.org/10.1007/s00737-007-0200-1
Cosgrove L, Shi L, Creasey DE, Anaya-McKivergan M, Myers JA, Huybrechts KF (2011) Antidepressants and breast and ovarian cancer risk: a review of the literature and researchers’ financial associations with industry. PLoS ONE 6(4):e18210. https://doi.org/10.1371/journal.pone.0018210
Dallaspezia S, Benedetti F, Colombo C, Barbini B, Fulgosi MC, Gavinelli C, Smeraldi E (2012) Optimized light therapy for non-seasonal major depressive disorder: effects of timing and season. J Affect Disord 138(3):337–42. https://doi.org/10.1016/j.jad.2012.01.019
Dias RS, Lafer B, Russo C, Del Debbio A, Nierenberg AA, Sachs GS, Joffe H (2011) Longitudinal follow-up of bipolar disorder in women with premenstrual exacerbation: findings from STEP-BD. Am J Psychiatry 168(4):386–394. https://doi.org/10.1176/appi.ajp.2010.09121816
Epperson CN, Terman M, Terman JS, Hanusa BH, Oren DA, Peindl KS, Wisner KL (2004) Randomized clinical trial of bright light therapy for antepartum depression: preliminary findings. J Clin Psychiatry 65(3):421–425
Even C, Schroder CM, Friedman S, Rouillon F (2008) Efficacy of light therapy in nonseasonal depression: a systematic review. J Affect Disord 108(1–2):11–23. https://doi.org/10.1016/j.jad.2007.09.008
First MB, Gibbon M, Spitzer RL, Williams JBW (1995) Structured Clinical Interview for DSM-IV Axis I Disorders - Research Version. Biometerics Research Department, New York State Psychiatric Institute
Fritzsche M, Heller R, Hill H, Kick H (2001) Sleep deprivation as a predictor of response to light therapy in major depression. J Affect Disord 62(3):207–215
Giedke H, Schwarzler F (2002) Therapeutic use of sleep deprivation in depression. Sleep Med Rev 6(5):361–377
Goel N, Basner M, Rao H, Dinges DF (2013) Circadian rhythms, sleep deprivation, and human performance. Prog Mol Biol Transl Sci 119:155–190. https://doi.org/10.1016/B978-0-12-396971-2.00007-5
Golden RN, Gaynes BN, Ekstrom RD, Hamer RM, Jacobsen FM, Suppes T, Wisner KL, Nemeroff CB (2005) The efficacy of light therapy in the treatment of mood disorders: a review and meta-analysis of the evidence. Am J Psychiatry 162(4):656–662
Halbreich U, Endicott J (1985) Relationship of dysphoric premenstrual changes to depressive disorders. Acta Psychiatr Scand 71(4):331–338
Halbreich U, O’Brien PM, Eriksson E, Backstrom T, Yonkers KA, Freeman EW (2006) Are there differential symptom profiles that improve in response to different pharmacological treatments of premenstrual syndrome/premenstrual dysphoric disorder? CNS Drugs 20(7):523–547
Hamilton JA, Parry BL, Alagna SW, Blumenthal SJ, Herz E (1984) Premenstrual mood changes: a guide to evaluation and treatment. Psychiatr Ann 14(6):426–435
Kripke DF, Risch SC, Janowsky DS (1983) Lighting up depression. Psychopharmacol Bull 19:526–530
Leibenluft E, Wehr TA (1992) Is sleep deprivation useful in the treatment of depression? Am J Psychiatry 149(2):159–168
Lewy AJ, Lefler BJ, Emens JS, Bauer VK (2006) The circadian basis of winter depression. Proc Natl Acad Sci U S A 103(19):7414–7419
Loving RT, Kripke DF, Shuchter SR (2002) Bright light augments antidepressant effects of medication and wake therapy. Depress Anxiety 16(1):1–3
Meliska CJ, Martinez LF, Lopez AM, Sorenson DL, Nowakowski S, Parry BL (2011) Relationship of morningness-eveningness questionnaire score to melatonin and sleep timing, body mass index and atypical depressive symptoms in peri- and post-menopausal women. Psychiatry Res 188(1):88–95. https://doi.org/10.1016/j.psychres.2010.12.010
Monteleone P, Martiadis V, Maj M (2011) Circadian rhythms and treatment implications in depression. Prog Neuropsychopharmacol Biol Psychiatry 35(7):1569–1574. https://doi.org/10.1016/j.pnpbp.2010.07.028
Morin LP, Fitzgerald KM, Zucker I (1977) Estradiol shortens the period of hamster circadian rhythms. Science 196(4287):305–307
Neumeister A, Goessler R, Lucht M, Kapitany T, Bamas C, Kasper S (1996) Bright light therapy stabilizes the antidepressant effect of partial sleep deprivation. Biol Psychiatry 39(1):16–21
Oren DA, Wisner KL, Spinelli M, Epperson CN, Peindl KS, Terman JS, Terman M (2002) An open trial of morning light therapy for treatment of antepartum depression. Am J Psychiatry 159(4):666–669
Parry BL (1995) Mood disorders linked to the reproductive cycle in women. In: Bloom FE, Kupfer DJ (eds) Psychopharmacology: The Fourth Generation of Progress. Raven Press Ltd, pp 1029–1042
Parry BL (2001) The role of central serotonergic dysfunction in the aetiology of premenstrual dysphoric disorder: therapeutic implications. CNS Drugs 15(4):277–285
Parry BL (2002) Jet lag: minimizing it’s effects with critically timed bright light and melatonin administration. J Mol Microbiol Biotechnol 4(5):463–466
Parry BL, Maurer EL (2003) Light treatment of mood disorders. Dialogues Clin Neurosci 5(4):353–365
Parry BL, Wehr TA (1987) Therapeutic effect of sleep deprivation in patients with premenstrual syndrome. Am J Psychiatry 144(6):808–810
Parry BL, Rosenthal NE, Tamarkin L, Wehr TA (1987) Treatment of a patient with seasonal premenstrual syndrome. Am J Psychiatry 144(6):762–766
Parry BL, Berga SL, Mostofi N, Sependa PA, Kripke DF, Gillin JC (1989) Morning versus evening bright light treatment of late luteal phase dysphoric disorder. Am J Psychiatry 146(9):1215–1217
Parry BL, Mahan AM, Mostofi N, Klauber MR, Lew GS, Gillin JC (1993) Light therapy of late luteal phase dysphoric disorder: an extended study. Am J Psychiatry 150(9):1417–1419
Parry BL, Cover H, Mostofi N, LeVeau B, Sependa PA, Resnick A, Gillin JC (1995) Early versus late partial sleep deprivation in patients with premenstrual dysphoric disorder and normal comparison subjects. Am J Psychiatry 152(3):404–412
Parry BL, Berga SL, Mostofi N, Klauber MR, Resnick A (1997) Plasma melatonin circadian rhythms during the menstrual cycle and after light therapy in premenstrual dysphoric disorder and normal control subjects. J Biol Rhythms 12(1):47–64
Parry BL, Udell C, Elliott JA, Berga SL, Klauber MR, Mostofi N, LeVeau B, Gillin JC (1997) Blunted phase-shift responses to morning bright light in premenstrual dysphoric disorder. J Biol Rhythms 12(5):443–456
Parry BL, Mostofi N, LeVeau B, Nahum HC, Golshan S, Laughlin GA, Gillin JC (1999) Sleep EEG studies during early and late partial sleep deprivation in premenstrual dysphoric disorder and normal control subjects. Psychiatry Res 85(2):127–143
Parry BL, Curran ML, Stuenkel CA, Yokimozo M, Tam L, Powell KA, Gillin JC (2000) Can critically timed sleep deprivation be useful in pregnancy and postpartum depressions? J Affect Disord 60(3):201–212
Parry BL, Meliska CJ, Martinez LF, Lopez A, Sorenson D, Hauger R, Elliott JA (2008) Late, but not early, wake therapy reduces morning plasma melatonin: relationship to mood in Premenstrual Dysphoric Disorder. Psychiatry Res 161(1):76–86
Parry BL, Meliska CJ, Sorenson DL, Lopez AM, Martinez LF, Nowakowski S, Elliott JA, Hauger RL, Kripke DF (2008) Plasma melatonin circadian rhythm disturbances during pregnancy and postpartum in depressed women and women with personal or family histories of depression. Am J Psychiatry 165(12):1551–1558
Parry BL, Meliska CJ, Sorenson DL, Lopez AM, Martinez LF, Nowakowski S, Hauger RL, Elliott JA (2008) Increased melatonin and delayed offset in menopausal depression: role of years past menopause, follicle-stimulating hormone, sleep end time, and body mass index. J Clin Endocrinol Metab 93(1):54–60
Parry BL, Meliska CJ, Sorenson DL, Martinez LF, Lopez AM, Elliott JA, Hauger RL (2011) Reduced phase-advance of plasma melatonin after bright morning light in the luteal, but not follicular, menstrual cycle phase in premenstrual dysphoric disorder: an extended study. Chronobiol Int 28(5):415–424. https://doi.org/10.3109/07420528.2011.567365
Parry BL, Meliska CJ, Lopez AM, Sorenson DL, Martinez LF, Orff HJ, Hauger RL, Kripke DF (2019) Early versus late wake therapy improves mood more in antepartum versus postpartum depression by differentially altering melatonin-sleep timing disturbances. J Affect Disord 245:608–616. https://doi.org/10.1016/j.jad.2018.11.064
Payne J (2011) Bipolar disorder in women with premenstrual exacerbation. Am J Psychiatry 168(4):344–346. https://doi.org/10.1176/appi.ajp.2011.11010171
Riemann D, Konig A, Hohagen F, Kiemen A, Voderholzer U, Backhaus J, Bunz J, Wesiack B, Hermle L, Berger M (1999) How to preserve the antidepressive effect of sleep deprivation: a comparison of sleep phase advance and sleep phase delay. Eur Arch Psychiatry Clin Neurosci 249(5):231–237
Schilgen, B., & Tolle, R. (1980). Partial sleep deprivation as therapy for depression. Arch Gen Psychiatry, 37(3), 267–271. http://www.ncbi.nlm.nih.gov/pubmed/7189111
Sokolski KN, Reist C, Chen CC, DeMet EM (1995) Antidepressant responses and changes in visual adaptation after sleep deprivation. Psychiatry Res 57(3):197–207
Srinivasan V, Smits M, Spence W, Lowe AD, Kayumov L, Pandi-Perumal SR, Parry B, Cardinali DP (2006) Melatonin in mood disorders. World J Biol Psychiatry 7(3):138–151
Terman M, Terman JS, Quitkin FM, McGrath PJ, Stewart JW, Rafferty B (1989) Light therapy for seasonal affective disorder A Review of Efficacy. Neuropsychopharmacology 2(1):1–22
Terman JS, Terman M, Lo ES, Cooper TB (2001) Circadian time of morning light administration and therapeutic response in winter depression. Arch Gen Psychiatry 58(1):69–75
Tuunainen A, Kripke DF, Elliott JA, Assmus JD, Rex KM, Klauber MR, Langer RD (2002) Depression and endogenous melatonin in postmenopausal women. J Affect Disord 69(1–3):149–158
Tuunainen A, Kripke DF, and Endo T. (2004). Light therapy for non-seasonal depression (Cochrane Database Syst Review). In The Cochrane Library. Issue 2. John Wiley & Sons https://doi.org/10.1002/14651858CD004050
van den Burg W, Bouhuys AL, van den Hoofdakker RH, Beersma DG (1990) Sleep deprivation in bright and dim light: antidepressant effects on major depressive disorder. J Affect Disord 19(2):109–117
Wehr TA, Wirz-Justice A (1981) Internal coincidence model for sleep deprivation and depression. In: Koella WP (ed) Sleep 1980. Karger, pp 26–33
Wehr TA, Wirz-Justice A (1982) Circadian rhythm mechanisms in affective illness and in antidepressant drug action. Pharmacopsychiatria 15(1):31–39
Wehr TA, Rosenthal NE, Sack DA, Gillin JC (1985) Antidepressant effects of sleep deprivation in bright and dim light. Acta Psychiatr Scand 72(2):161–165
Williams JB, Terman M (2003) Structured Interview Guide for the Hamilton Depression Rating Scale with Atypical Depression Supplement (SIGH-ADS). New York State Prychiatric Institute
Wirz-Justice A (2011) The implications of chronobiology for psychiatry. Psychiatric Times 56–61. https://www.cmellc.com/landing/pdf/A11001101.pdf
Wirz-Justice A, Terman M (2012) Chronotherapeutics (light and wake therapy) as a class of interventions for affective disorders. Handb Clin Neurol 106:697–713. https://doi.org/10.1016/B978-0-444-52002-9.00042-5
Wirz-Justice A, Van den Hoofdakker RH (1999) Sleep deprivation in depression: what do we know, where do we go? Biol Psychiatry 46(4):445–453
Wirz-Justice A, Bader A, Frisch U, Stieglitz RD, Alder J, Bitzer J, Hosli I, Jazbec S, Benedetti F, Terman M, Wisner KL, Riecher-Rossler A (2011) A randomized, double-blind, placebo-controlled study of light therapy for antepartum depression. The Journal of Clinical Psychiatry 72(7):986–993. https://doi.org/10.4088/JCP.10m06188blu
Wirz-Justice A, Benedetti F, Terman M (2013) Chronotherapeutics for affective disorders : a clinician’s manual for light and wake therapy, 2nd edn. Karger
Wu JC, Bunney WE (1990) The biological basis of an antidepressant response to sleep deprivation and relapse: review and hypothesis. Am J Psychiatry 147(1):14–21
Wu JC, Kelsoe JR, Schachat C, Bunney BG, Demodena A, Golshan S, Gillin JC, Potkin SG, Bunney WE (2009) Rapid and sustained antidepressant response with sleep deprivation and chronotherapy in bipolar disorder. Biol Psychiatry 66(3):298–301
Yonkers KA, O’Brien PM, Eriksson E (2008) Premenstrual syndrome. Lancet 371(9619):1200–1210. https://doi.org/10.1016/S0140-6736(08)60527-9
Funding
This work was supported by the National Institutes of Health R01 AT007169.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Parry, B.L., Meliska, C.J., Martinez, L.F. et al. A 1-week sleep and light intervention improves mood in premenstrual dysphoric disorder in association with shifting melatonin offset time earlier. Arch Womens Ment Health 26, 29–37 (2023). https://doi.org/10.1007/s00737-022-01283-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-022-01283-z