Abstract
Purpose
The international perinatal literature focuses on depression in the postpartum period. Prevalence and pathways of depression, anxiety and stress from pregnancy through the first postpartum year are seldom investigated.
Methods
MAMMI is a prospective cohort study of 3009 first-time mothers recruited in pregnancy. Depressive, anxiety and stress symptoms measured using the Depression, Anxiety and Stress Scale (DASS 21) in pregnancy and at 3-, 6-, 9- and/or 12-months postpartum.
Results
Prevalence of depressive and stress symptoms was lowest in pregnancy, increasing to 12-months postpartum. Anxiety symptoms remained relatively stable over time. In the first year after having their first baby, one in ten women reported moderate/severe anxiety symptoms (9.5%), 14.2% reported depression symptoms, and one in five stress symptoms (19.2%). Sociodemographic factors associated with increased odds of postpartum depression, anxiety and stress symptoms were younger age and being born in a non-EU country; socioeconomic factors were not living with a partner, not having postgraduate education and being unemployed during pregnancy. Retrospective reporting of poor mental health in the year prior to pregnancy and symptoms during pregnancy were strongly associated with poor postpartum mental health.
Conclusions
The current findings suggest that the current model of 6-week postpartum care in Ireland is insufficient to detect and provide adequate support for women’s mental health needs, with long-term implications for women and children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although many women navigate pregnancy, birth and motherhood in good physical and mental health, it is a significant transition (Jomeen 2017; Jomeen and Martin 2008; Nelson 2013; Parfitt and Ayers 2014), and adverse mental health effects are widely recognised (Jomeen 2004; Lee 2000). Perinatal mental health problems are among the most common health issues associated with childbearing (Howard and Khalifeh 2020), and are of public health concern owing to the long-term consequences for a woman’s wellbeing (Meltzer-Brody and Stuebe 2014), intimate relationships (Yeaton-Massey and Herrero, 2019), the mother-infant bond (Cirulli et al. 2003) and the physical, social and cognitive development of her child (O’Connor et al. 2016; Schuurmans and Kurrasch, 2013). In addition, maternal suicide remains the leading cause of direct deaths occurring within a year after the end of pregnancy in the UK (Knight et al. 2021) and Ireland (O’Hare et al. 2021).
A review of longitudinal studies of antenatal and postpartum depression reports prevalence of 17.2% and 13.1% respectively (Underwood et al. 2016). Another review found higher prevalence of depression in the antenatal and postpartum periods among women in low and middle income countries (LMIC) compared to women in high-income countries (HIC) (Antenatal: LMIC = 19.2%, HIC = 9.2%; Postpartum: LMIC = 18.7%, HIC = 9.5%) (Woody et al. 2017). There is considerable variation in the depression prevalence reported between countries and cultures (Abdollahi et al. 2011; Halbreich and Karkun 2006).
While research in the perinatal period has predominately focused on depression, there is increasing interest on the impacts of anxiety, and comorbid anxiety and depression (Austin et al. 2010; Falah-Hassani et al. 2016; Farr et al. 2014). There is variation in the prevalence of anxiety disorders between the antenatal and postpartum period, between countries and cultures and between HIC and LMIC (Dennis et al. 2017) and evidence of higher prevalence of anxiety than depression both during and after pregnancy (Lee et al. 2007; Wenzel et al. 2003).
Stress is considered a distinct negative emotional state with deleterious impact on one’s overall mental health (Lovibond and Lovibond 1995a, b) and has been linked to negative outcomes for mother and child (Dunkel Schetter and Tanner 2012). Investigation of perinatal/maternal stress is frequently subsumed with anxiety and reported as ‘distress’ in the perinatal literature (Bryson et al. 2021).
A history of mental health problems is a key, and frequently cited, risk factor for poor maternal mental health outcomes (van der Waerden et al. 2015; Patton et al. 2015). Other risks include low socioeconomic status, inadequate social or emotional support, poor partner relationship, current domestic abuse, past abuse, refugee or asylum seeker status, undesirable obstetric outcomes, undesirable neonatal outcomes or an unplanned pregnancy (Fisher et al. 2012; Gartland et al. 2019; Paschetta et al. 2014).
Perinatal mental health in Ireland
Ireland’s first National Maternity Strategy (Department of Health 2016) led to the development and publication of the Specialist Perinatal Mental Health Model of Care for Ireland (Health Service Executive (HSE) 2017). Though the model is ‘informed by national and international epidemiological evidence of need’ (HSE 2017 p7), estimates of the numbers of women affected by perinatal mental illnesses in Ireland are extrapolated from the UK data such as Prevention in Mind (Hogg 2013), and JCP-MH (2012).
Currently, in Ireland, there are no data collected or published at a national level on the prevalence, pathways, outcomes or long-term development of perinatal mental health problems. Information regarding women’s perinatal mental health comes from individual studies (Department of Health 2016). In addition, perinatal maternal health care, provided by the public sector, generally ceases for mothers at 6-week postpartum. Women who experience perinatal mental health problems beyond this period are not supported within the maternity care system, or by a system enabled to readily detect and offer treatment; rather, women must identify their own needs and seek treatment.
Researcher and clinician understanding of the current state of perinatal mental health in Ireland come from several disparate sources. Huschke et al’s (2020) recent review of the available data demonstrates substantial variation in reported prevalence. The prevalence of depression during pregnancy ranged from 1% (McAuliffe et al. 2011) to 86% (Carolan-Olah and Barry 2014), and postpartum depression from 11% (Cruise et al. 2018) to 28.6% (Cryan et al. 2001). Similarly, antenatal anxiety prevalence varied from 27.3% (Togher et al. 2017) to 75% (Carolan-Olah and Barry 2014). Importantly, the review did not identify data on postpartum anxiety prevalence. Prevalence of stress during pregnancy varied from 25% (Bennett and Kearney 2018) to 75% (Carolan-Olah and Barry 2014), with a single study reporting 8% in the postpartum period (Bennett and Kearney 2018). A possible reason for such wide variation may be differences in sample composition and size, criteria for inclusion, measurements used and assessment time points. Additionally, the authors note that only one study included a representative sample (Cruise et al. 2018).
In light of the sparse, contradictory and absent data on perinatal mental health in Ireland, there is a need for a better understanding of the prevalence, trajectories over time and risk factors for poor perinatal mental health for women giving birth in Ireland. The current study adds to the Irish and international literature using the advantages of data collect on depression, anxiety and stress at multiple time point across the first postpartum year, with a largely representative sample.
The current paper uses data from a large prospective cohort study of nulliparous women giving birth in Ireland to (1) describe the prevalence of depression, anxiety and stress during pregnancy and the first year postpartum; (2) assess changes in prevalence over the first year of motherhood and (3) identify factors associated with poor postpartum mental health.
Methods
Design
This study is part of the larger MAMMI (Maternal health And Maternal Morbidity in Ireland) study, a multi-site, multi-strand, longitudinal cohort study examining the health of first-time mothers giving birth in Ireland. The MAMMI study is a mixed-methods study incorporating self-completion surveys, data collection from consenting women’s maternity records and one-to-one interviews with women experiencing a specific morbidity, for example sexual health problems (Daly et al. 2018; O’Malley et al. 2019, 2018) (for details on study design: https://www.tcd.ie/mammi/).
Recruitment
Nulliparous women were recruited at their first booking visit, with the majority enrolling in the second trimester of pregnancy, (average 17.5 weeks’ gestation), from three maternity hospitals in Ireland between January 2012 and March 2017. Eligible women were nulliparous, aged 18 years and over and able to read and understand English sufficiently to complete the surveys.
Midwives in the participating recruitment sites offered all women meeting the study’s eligibility criteria a study information pack at their first antenatal appointment. Approximately 8243 women received the study information across the three research sites; 3131 participants completed the enrolment questionnaire, giving a response rate of 38%. Follow-up was at 3-, 6-, 9- and 12-months postpartum. No incentive was given for participation. Ethics approval was granted by the three hospitals and the university research ethics committees.
Participants
Of the 3131 women who completed the enrolment questionnaire in pregnancy, 122 had a miscarriage, stillbirth or seriously ill baby in the NICU and were excluded. The majority of women were born in Ireland (73.8%), were aged 30 years or older (73.9%), were living with a partner (97.3%) and had postgraduate education (71.7%) (see Table 1). A flowchart of participation is presented in Fig. 1.
While there is limited national data in Ireland, available data for the study recruitment period suggest that the cohort is broadly representative in terms of maternal age and country of birth (CSO 2016; Coulter-Smith 2016; IMIS 2016), but may have a higher proportion of women living with their partner, in paid work, and fewer women who had spontaneous vaginal births (see Supplementary Table 1 for more details) (Daly et al. 2019).
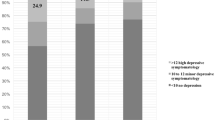
The sample for this paper comprised 2380 women who completed the DASS at 2 or more follow-ups in the first year postpartum. Prevalence of symptoms at each time point is presented graphically for the 1806 women who completed the DASS at all time points from pregnancy to 12-months postpartum.
Measures
Self-report on mental and social factors in the year PRIOR and DURING index pregnancy
Participants were asked ‘During the last 12 months BEFORE your pregnancy did you experience…’ and ‘Since the start of your pregnancy, have you experienced…’.
-
feeling depressed, low mood or sad (lasting 2 weeks or more)
-
intense anxiety (such as panic attacks)
-
relationship problems with your partner/spouse
-
fear of a partner
Response options were ‘often’, ‘occasionally’, ‘rarely’, and ‘never’. Responses were dichotomised as often/occasionally versus rarely/never.
Pregnancy and birth
In the baseline questionnaire, participants were asked if the index pregnancy was conceived with assistance from fertility treatments. Response options included ‘Fertility drugs’, ‘In Vitro Fertilisation (IVF)’, ‘Intracytoplasmic sperm injection (ICSI)’ and ‘Other (please describe)’. Weeks’ gestation at enrolment and birth was calculated using the estimated due date and date of enrolment and infant birth date respectively. Mean gestation at enrolment was 17.5 weeks (range 4.0–39.7 weeks). Maternal self-report of mode of birth and infant birth weight were employed for this study, as they have been shown to be very reliable when compared to hospital records (Gartland et al. 2012).
Repeated mental health assessment
The short form Depression, Anxiety and Stress Scale (DASS 21) (Henry and Crawford 2005; Lovibond and Lovibond 1995a, b) was used to assess mental health symptoms at enrolment in pregnancy and at 3-, 6-, 9- and 12-months postpartum. Three scales of 7 items are rated on a 4-point scale ranging from 0 ‘Did not apply to me at all’ to 3 ‘Applied to me very much or most of the time’. The Depression scale includes dysphoria, hopelessness, devaluation of life and self-deprecation. The Anxiety scale includes autonomic arousal, skeletal muscle effects and situational anxiety. The Stress scale includes difficulty relaxing, nervous arousal and being easily upset/agitated. Good reliability and discriminant validity have been reported (Brown et al. 1997; Crawford and Henry 2003; Henry and Crawford 2005). The DASS excludes potential confounders such as sleep disturbance, appetite and weight changes, tiredness and fatigue, which may not be appropriate indicators of depression, anxiety or stress among pregnant and postpartum populations. Cronbach alpha coefficients for each subscale have been reported as very good in both pregnant (Depression; α = 0.82, Anxiety; α = 0.79, Stress; α = 0.89) (Xavier et al. 2016) and postpartum (Depression; α = 0.84, Anxiety; α = 0.77, Stress; α = 0.86) (Miller et al. 2006) populations.
At each time point, scales were summed to create a total scale score. A dichotomous variable was created for each scale to identify none or low symptoms versus moderate to severe symptoms using the recommended cut off scores: ≥ 7 for the depression scale, ≥ 6 for anxiety and ≥ 10 for stress (Lovibond and Lovibond 1995a, b). Scoring above the cut off scores indicates clinically relevant levels of psychological distress. A 12-month period prevalence variable was created for each scale to identify moderate to severe symptoms reported at one or more of the 3-, 6-, 9- or 12-month follow-ups.
Sociodemographic and socioeconomic data
Sociodemographic information (relationship status, age, country of birth) and socioeconomic (education qualifications, employment and housing) were collected at enrolment and follow-up.
Data analysis
Regression analyses were conducted to assess if baseline DASS scores reported by women at enrolment in pregnancy were affected by timing of enrolment in weeks’ gestation or by trimester. Prevalence of depression, anxiety and stress symptoms in pregnancy and at 3, 6, 9 and 12 months were calculated at each time point as the proportion of women reporting clinically relevant level symptoms divided by the number of women who completed the scale. Logistic regression was used to model associations between report of depression, anxiety and stress in the first year postpartum and (1) maternal sociodemographic and socioeconomic characteristics and (2) preceding social, physical and maternal factors. Models examining associations between preceding factors and postpartum mental health (2) were adjusted for sociodemographic and socioeconomic factors associated with postpartum mental health in step (1).
Results
Maternal mental health in pregnancy and the first year postpartum
Women completed the DASS at enrolment in pregnancy with gestations ranging from 4 to 39 weeks (mean gestation = 17.5). The majority of women enrolled in the second trimester (75.5%). Linear regression modelling identified no difference in baseline total DASS scores by weeks’ gestation (F(1,2374) = − 0.003, 95% CI − 0.030, 0.025, p = 0.854) or the odds of reporting moderate/severe depressive, anxiety or stress symptoms in pregnancy by trimester (data not shown). Therefore, DASS scores in pregnancy are presented as a single time point rather than stratified by gestation.
To examine the prevalence of moderate/severe mental health symptoms over time, a subsample of women who completed the DASS at every time point (pregnancy, and at 3-, 6-, 9-, and 12-months postpartum) are presented in Fig. 2. Different patterns in the prevalence of moderate/severe depression, anxiety and stress symptoms reported over time were observed and are described below.
As shown in Fig. 2, the proportion of women classified as having moderate/severe depressive symptoms was lowest in pregnancy (3.9%), and significantly higher at 6- and 12-months postpartum (≈6.0%). The proportion of women reporting moderate/severe anxiety symptoms was relatively consistent from pregnancy (4.5%) across the first year postpartum (≈4.0), with overlapping 95% confidence intervals indicating no statistically significant differences. Stress was different again, with the lowest proportion of women reporting moderate/severe levels of stress in pregnancy (4.8%), rising to 7.7% at 3 months postpartum and remaining significantly higher across the following time points (see Fig. 2).
Demographic and birth factors associated with postpartum mental health
Associations between demographic factors and report of poor mental health in the first year postpartum are shown in Table 1 for the larger sample of 2380 women who completed the DASS in a minimum of 2 postpartum follow-ups.
In the first year after having their first baby, one in ten women reported moderate/severe anxiety symptoms (9.5%), more than one in ten reported moderate/severe depression symptoms (14.2%) and one in five reported moderate/severe stress (19.2%).
Demographic factors
Being younger (< 30 years) was associated with higher odds of reporting depression, anxiety and stress symptoms in the first year postpartum. For example, women aged 18–24 years in pregnancy had higher odds of reporting depressive symptoms (OR = 2.8, 95% CI 1.8–4.2), anxiety (OR = 3.5, 95% CI, 2.2–5.4) and stress (OR = 2.4, 95% CI 1.7–3.6) compared to women in the median age (30–34 years). Being born in a non-EU country, not living with a partner, not having postgraduate education and being unemployed during pregnancy were associated with 2–3 times higher odds of reporting depressive symptoms, anxiety symptoms or stress in the first year of mothering.
Birth factors
Having a pre-term birth was associated with higher odds of postpartum depressive symptoms, while giving birth via a caesarean section was associated with higher odds of postpartum depressive and stress symptoms. The baby’s birth weight was not associated with poor postpartum mental health.
Health and social factors associated with postpartum mental health
Factors in the year prior to the pregnancy (retrospective report)
Poor mental health in the year prior to the index pregnancy was strongly associated with poor postpartum mental health as shown in Table 2. Endorsement of depressive or anxiety symptoms as happening occasionally or often in the year prior to the pregnancy was associated with a four to sevenfold increase in the odds of depressive, anxiety or stress symptoms in the first year postpartum, after adjusting for maternal age, education and relationships status. Similarly, relationship problems in the year prior to the pregnancy were associated with a twofold increase in the odds of postpartum depressive, anxiety or stress symptoms. Fertility treatment to conceive this pregnancy was not associated with poor mental health in the first year postpartum.
Factors in pregnancy
Endorsement of two items asking about depressive or anxiety symptoms during pregnancy was associated with a four to fivefold increase in the odds of depression, anxiety or stress postpartum. Moderate to severe depression, anxiety and stress symptoms (DASS) during pregnancy were associated with a five to 12-fold increase in the odds of reporting moderate to severe postpartum symptoms, with the highest odds observed for the same dimension. For example, depressive symptoms in pregnancy were associated with odds of 12.8 (95% CI 8.3–19.8) for postpartum depressive symptoms compared to women not reporting depressive symptoms in pregnancy.
Other factors during pregnancy associated with postpartum depressive, anxiety and stress symptoms included relationship problems, fear of a partner and, (for depressive symptoms only) not living with a partner.
While prior depressive or anxiety symptoms were strongly associated with postpartum mental health, it is important to note that most women with poor postpartum mental health had not reported these symptoms in pregnancy. Of women with depressive symptoms in the first year postpartum, 69.1% had not reported depressive symptoms in pregnancy (on the single item or the DASS). Similarly, 71% of women with postpartum anxiety symptoms had not reported anxiety symptoms in pregnancy.
Discussion
In this large Irish cohort of first-time mothers, one in seven women reported moderate to severe depressive, and one in ten reported moderate to severe anxiety symptoms at some points in the first postpartum year. This study’s findings are congruent with those from other longitudinal studies of perinatal depression and anxiety reported in developed countries (Dennis et al. 2017; Underwood et al. 2016). One in five women in the MAMMI study cohort reported moderate to severe stress symptoms in their first year of mothering, congruent with a study identified from the USA, where 21% of multiparous women reported moderate/severe stress at ≈5-months postpartum (Clout and Brown 2015).
Depression, anxiety and stress were highest among younger first-time mothers (< 30 years). This is in line with international (Agnafors et al. 2019; Silverman et al. 2017) and Irish (Cruise et al. 2018) data (which was conducted with a representative sample) indicating that motherhood at a younger age represents increased risk for poor mental health. Additional factors indicating socioeconomic disadvantage were lower educational qualification attainment, not cohabiting with a partner and maternal unemployment during pregnancy and sociodemographic risk was being born in a non-EU country—these factors were all more common for the younger mothers compared to older first-time mothers. For example, 27% of mothers aged 18–24 years had postgraduate education compared to 76% of mothers aged 35 or older; similarly, 62% were working in pregnancy compared to 95% of older mothers. This study’s findings correspond with international data on socioeconomic and sociodemographic risk factors for poorer postpartum mental health (Goyal et al. 2010). It is worth noting that the findings on unemployment, lower educational qualification attainment, living apart from a partner and being born in a non-EU country highlight at risk groups who may benefit from facilitated access to perinatal mental health services and support. Socioeconomic disadvantage is linked to exposure to multiple risks with cumulative impact, such as decreased financial resources and social support, resulting in greater barriers to accessing mental health services and reduced likelihood of disclosing mental health symptoms to health care professionals (Goyal et al. 2010; Kimerling and Baumrind 2005). The sociodemographic risk implied by a woman being born outside of an EU country is of particular importance in an Irish context as the ethnic diversity of the population living and giving birth in Ireland is projected to continue to increase (CSO 2016). In addition, disparities in racial and ethnic minority access to mental health care is noted in Irish ( Bojarczuk et al. 2015) and the international literature (Cook et al. 2017).
As with reported depressive and anxiety symptoms, reported stress symptoms were more common for mothers in the younger age groups. In 2018, 62.4% of first-time mothers were aged 30 years or over, and 26% of first births were to women aged 35 years or older (HPO 2021). It may be that decreased resources available to the younger mothers are more strongly associated with stress (Easterbrooks et al. 2011), while older mothers may have more social and economic resources to buffer or protect their mental health.
Women with pre-term births had increased likelihood of experiencing symptoms of depression and stress (borderline statistical significance) in their first postpartum year. This is congruent with the literature, which reports two to six times increase in postpartum anxiety and/or depressive symptoms among mothers with pre-term infants (Farr et al. 2014).
Following adjustment for maternal age, education and relationship status, women who reported relationship problems or being afraid of their partner during the pregnancy had higher odds of experiencing moderate to severe depressive, anxiety and stress symptoms in the postpartum period. While relationship problems should not be conflated with intimate partner violence, these findings on relationship problems and fear of partner highlight that clinicians need to provide all women with an opportunistic window to discuss available supports and resource pathways, and assistance to access support where required.
The current study further adds to the international literature highlighting that mental health symptoms prior to pregnancy are strong indicators of potential postpartum issues (Dunkel Schetter and Tanner 2012; Bryson et al. 2021). Notably, in the MAMMI study cohort, a positive response to two single-item questions on the experience of depression or anxiety were associated with a four to sevenfold increase in the odds of moderate to severe postpartum depressive, anxiety or stress symptoms. Comparably, the two-item Whooley questions, which assess recent low mood and loss of interest or pleasure, have been found to have high sensitivity and modest specificity in detecting depression and high acceptability with women (Bosanquet et al. 2015; National Collaborating Centre for Mental Health 2007; Yapp et al. 2019). Integration of the current questions into routine antenatal clinical visits offers a time-efficient and potentially non-invasive means of identifying risk for both anxiety and depression symptoms among women who may benefit from closer postpartum monitoring and support. Additionally, moderate to severe symptoms during pregnancy on the DASS were associated with five to 12-fold increased odds of moderate to severe symptoms in the postpartum. The relationship between self-reported symptomatology detected by the DASS in pregnancy and subsequent increase in symptomology in the postpartum suggest that the DASS may offer a robust means of antenatal screening for a broader scope of mental health issues occurring postpartum. Suggested use of the two single-item questions or the DASS, however, are offered with the caveat that women’s disclosures in the current study were made with the expectation of anonymity rather than to a healthcare professional which may circumvent possible self-censoring that women engage in due to stigma or concerns about healthcare or child service intervention.
Although reports of depressive or anxiety symptoms during pregnancy were strongly associated with mental health problems in the postpartum, it is important to note that a majority of women who reported postpartum moderate to severe depression and anxiety symptoms did not report symptoms during pregnancy (69.1% and 71% respectively). Additionally, the current study identified variation in the prevalence of depressive, anxiety and stress symptoms across the first year, with peaks observed for depressive and stress symptoms at 6- and 12-months postpartum. The majority of women reporting postpartum symptoms without prior history and the variability in symptomatology support the need for repeated enquiry about mental health in both antenatal and postpartum care.
In Ireland, maternal postpartum care typically concludes at 6-week postpartum. This study’s findings suggest that the current model of postpartum care in Ireland is insufficient to detect, and provides adequate support for women’s mental health needs. Furthermore, women birthing in Ireland have reported that their postpartum care is predominately infant-centered and infrequently facilitates opportunities for women to discuss their own physical or mental health (Daly et al. 2021). Continued postpartum contact is vital to ensure that women who develop symptoms beyond 6-week postpartum are identified and receive the support that they need to regain optimum health.
Strengths and limitations
The strengths of this study include the use of a robust data collection instrument, a large sample size and frequent data collection across the first postpartum year. The findings need to be considered in light of the following limitations: although the sample is broadly representative of women giving birth in Ireland in terms of nationality and age, the sample was over representative of women living with their partner and in paid work. Additionally, limited data on socioeconomic and obstetric outcomes at a national level preclude a detailed comparison of the representativeness of the cohort. Thus, the findings may not be generalisable to women beyond the predominant sample demographics.
Conclusion
International and Irish research on perinatal mental health has focused on depression and the early postpartum months. There is limited data, particularly within an Irish context, to inform policy and practice on a broader range of mental health challenges and their development as women progress through motherhood. The current study offers findings from a large prospective Irish cohort study describing the prevalence and trajectories of depressive, anxiety and stress symptoms from pregnancy and the first year postpartum, and factors associated with poor maternal mental health. These findings are important to building a robust foundation of data on perinatal mental health in Ireland to inform national action.
This study’s findings suggest there are a substantial proportion of first-time mothers who experience depressive, anxiety and stress symptoms in pregnancy and the first postpartum year. Indices of sociodemographic and socioeconomic disadvantage indicate that younger mothers, women without higher education, women who are unemployed and women not living with a partner in pregnancy are at increased risk for reporting poor postpartum mental health, as are women who report relationship problems or fear of a partner.
The variation in mental health symptoms across the first year postpartum and new onset of symptoms imply that women would benefit from prolonged contact and support from maternity care services beyond the 6-week postpartum that is currently the norm for maternal care in Ireland.
Given the well-documented adverse impact of poor postpartum mental health for a woman’s wellbeing, her functioning as a mother and the cognitive and emotional development of her child (George et al. 2013; Cirulli et al. 2003; Yeaton-Massey and Herrero 2019; O’Connor et al. 2016; Schuurmans and Kurrasch 2013; Surkan, Kennedy, Hurley, Black, 2011; Hay, Pawlby, Waters, Perra, Sharp 2010), clinicians and researchers should be mindful that maternal mental health encompasses more than the experience of depression. Clinicians need also to be attentive to identifying and meeting women’s mental health needs through facilitation of disclosure, appropriate knowledge of (Higgins et al. 2018) and referral to, care and treatment pathways to ensure timely care of women.
References
Abdollahi F, Lye MS, Zain A, Ghazali SS, Zarghami M (2011) Postnatal depression and its associated factors in women from different cultures. Iran J Psychiatry Behav Sci 5(2):5–11
Agnafors S, Bladh M, Svedin CG, Sydsjö G (2019) Mental health in young mothers, single mothers and their children. BMC Psychiatry 19(1):112. https://doi.org/10.1186/s12888-019-2082-y
Austin MP, Hadzi-Pavlovic D, Priest SR, Reilly N, Wilhelm K, Saint K, Parker G (2010) Depressive and anxiety disorders in the postpartum period: how prevalent are they and can we improve their detection? Arch Womens Ment Health 13(5):395–401. https://doi.org/10.1007/s00737-010-0153-7
Bennett AE, Kearney JM (2018) Factors associated with maternal wellbeing at four months post-partum in Ireland. Nutrients 10:5. https://doi.org/10.3390/nu10050609
Bosanquet K, Bailey D, Gilbody S, Harden M, Manen M, Nutbrown S, McMillan D (2015) Diagnostic accuracy of the Whooley questions for the identification of depression: a diagnostic meta-analysis. BMJ Open 5(12):e008913. https://doi.org/10.1136/bmjopen-2015-008913
Brown TS, Chorpita BF, Korotitsch W, Barlow DH (1997) Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav Res Ther 35:1–79
Bryson H, Perlen S, Price A, Mensah F, Gold L, Dakin P, Goldfeld S (2021) Patterns of maternal depression, anxiety, and stress symptoms from pregnancy to 5 years postpartum in an Australian cohort experiencing adversity. Arch Womens Ment Health 1-11. https://doi.org/10.1007/s00737-021-01145-0
Bojarczuk S, Marchelewska E, Prontera M (2015) Ethnic Minorities and Mental Health in Ireland: Barriers and Recommendations. Cairdre Report. Cairde, 19 Belvedere Place, Dublin 1
Carolan-Olah M, Barry M (2014) Antenatal stress: an Irish case study. Midwifery 30(3):310–316. https://doi.org/10.1016/j.midw.2013.03.014
Central Statistics Office (CSO) (2016) Vital Statistics Annual Report, Births. Available at: https://www.cso.ie/en/releasesandpublications/ep/p-plfp/populationandlabourforceprojections2017-2051/.
Cirulli F, Berry A, Alleva E (2003) Early disruption of the mother-infant relationship: effects on brain plasticity and implications for psychopathology. Neurosci Biobehav Rev 27(1–2):73–82. https://doi.org/10.1016/s0149-7634(03)00010-1
Clout D, Brown R (2015) Sociodemographic, pregnancy, obstetric, and postnatal predictors of postpartum stress, anxiety and depression in new mothers. J Affect Disord 188:60–67. https://doi.org/10.1016/j.jad.2015.08.054
Cook BL, Trinh NH, Li Z, Hou SS, Progovac AM (2017) Trends in racial-ethnic disparities in access to mental health care, 2004–2012. Psychiatr Serv 68(1):9–16. https://doi.org/10.1176/appi.ps.201500453
Coulter-Smith S (2016) The Rotunda Hospital Clinical Report 2015 Dublin, Ireland. Available at: https://rotunda.ie/rotunda-pdfs/Clinical%20Reports/Rotunda%20Annual%20Report%202016.pdf
Crawford JR, Henry JD (2003) The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. Br J Clin Psychol 42:111–131. https://doi.org/10.1348/014466503321903544
Cruise SM, Layte R, Stevenson M, O’Reilly D (2018) Prevalence and factors associated with depression and depression-related healthcare access in mothers of 9-month-old infants in the Republic of Ireland. Epidemiol Psychiatr Sci 27(5):468–478. https://doi.org/10.1017/s2045796017000026
Cryan E, Keogh F, Connolly E, Cody S, Quinlan A, Daly I (2001) Depression among postnatal women in an urban Irish community. Ir J Psychol Med 18(1):5–10. https://doi.org/10.1017/S0790966700006145
Daly D, Clarke M, Begley C (2018) Urinary incontinence in nulliparous women before and during pregnancy: prevalence, incidence, type, and risk factors. Int Urogynecol J 29(3):353–362. https://doi.org/10.1007/s00192-018-3554-1
Daly D, Carroll M, Barros M, Begley C (2019) Stop, think, reflect, realize-first-time mothers’ views on taking part in longitudinal maternal health research. Health Expect 22(3):415–425. https://doi.org/10.1111/hex.12861
Daly D, Moran P, Wuytack F, Hannon S, Hannon K, Martin, Y, Peoples M, Begley C, Newnham E (2021) The maternal health-related issues that matter most to women in Ireland as they transition to motherhood - a qualitative study. Women Birth. https://doi.org/10.1016/j.wombi.2021.01.013
Dennis CL, Falah-Hassani K, Shiri R (2017) Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry 210(5):315–323. https://doi.org/10.1192/bjp.bp.116.187179
Department of Health (2016) Creating a better future together: National Maternity Strategy 2016 – 2026. Dublin.
Dunkel Schetter C, Tanner L (2012) Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatry 25(2):141–148. https://doi.org/10.1097/YCO.0b013e3283503680
Easterbrooks MA, Chaudhuri JH, Bartlett JD, Copeman A (2011) Resilience in parenting among young mothers: family and ecological risks and opportunities. Child Youth Serv Rev 33(1):42–50. https://doi.org/10.1016/j.childyouth.2010.08.010
Falah-Hassani K, Shiri R, Dennis CL (2016) Prevalence and risk factors for comorbid postpartum depressive symptomatology and anxiety. J Affect Disord 198:142–147. https://doi.org/10.1016/j.jad.2016.03.010
Farr SL, Dietz PM, O’Hara MW, Burley K, Ko KY (2014) Postpartum anxiety and comorbid depression in a population-based sample of women. J Womens Health 23(2):120–128. https://doi.org/10.1089/jwh.2013.4438
Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, Holmes W (2012) Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ 90(2):139G-149G. https://doi.org/10.2471/BLT.11.091850
Gartland D, Donath S, MacArthur C, Brown SJ (2012) The onset, recurrence and associated obstetric risk factors for urinary incontinence in the first 18 months after a first birth: an Australian nulliparous cohort study. BJOG 119(11):1361–1369. https://doi.org/10.1111/j.1471-0528.2012.03437.x
Gartland D, Giallo R, Woolhouse H, Mensah F, Brown SJ (2019) Intergenerational impacts of family violence—mothers and children in a large prospective pregnancy cohort study. EClinicalMedicine 15:51–61. https://doi.org/10.1016/j.eclinm.2019.08.008
George A, Luz RF, De Tychey C, Thilly N, Spitz E (2013) Anxiety symptoms and coping strategies in the perinatal period. BMC Pregnancy Childbirth 13(1):233. https://doi.org/10.1186/1471-2393-13-233
Goyal D, Gay C, Lee KA (2010) How much does low socioeconomic status increase the risk of prenatal and postpartum depressive symptoms in first-time mothers? Women’s Health Issues 20(2):96–104. https://doi.org/10.1016/j.whi.2009.11.003
Halbreich U, Karkun S (2006) Cross-cultural and social diversity of prevalence of postpartum depression and depressive symptoms. J Affect Disord 91(2–3):97–111. https://doi.org/10.1016/j.jad.2005.12.051
Hay DF, Pawlby S, Waters CS, Perra O, Sharp D (2010) Mothers’ antenatal depression and their children’s antisocial outcomes. Child Dev 81(1):149–165. https://doi.org/10.1111/j.1467-8624.2009.01386.x
Health Service Executive (2017) Specialist perinatal mental health services – model of care for Ireland. Available at: https://www.hse.ie/eng/services/list/4/mental-health-services/specialist-perinatal-mental-health/specialist-perinatal-mentalhealth-services-model-of-care-2017.pdf
Henry JD, Crawford JR (2005) The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol 44:227–239. https://doi.org/10.1348/014466505x29657
Higgins A, Downes C, Carroll M, Gill A, Monahan M (2018) There is more to perinatal mental health care than depression: public health nurses reported engagement and competence in perinatal mental health care. J Clin Nurs 27(3–4):e476–e487. https://doi.org/10.1111/jocn.13986
Hogg S (2013) Prevention in mind. all babies count: spotlight on perinatal mental health. London, NSPCC. Available at https://www.nspcc.org.uk/globalassets/documents/research-reports/all-babies-count-spotlight-perinatal-mentalhealth.pdf.
Howard LM, Khalifeh H (2020) Perinatal mental health: a review of progress and challenges. World Psychiatry 19(3):313–327. https://doi.org/10.1002/wps.20769
Howard LM, Molyneaux E, Dennis CL, Rochat T, Stein A, Milgrom J (2014) Non-psychotic mental disorders in the perinatal period. Lancet 384(9956):1775–1788. https://doi.org/10.1016/s0140-6736(14)61276-9
Healthcare Pricing Office (HPO) (2021) Perinatal Statistics Report 2018. Available at: https://www.hpo.ie/latest_hipe_nprs_reports/NPRS_2018/Perinatal_Statistics_Report_2018.pdf
Huschke S, Murphy-Tighe S, Barry M (2020) Perinatal mental health in Ireland: a scoping review. Midwifery 89:102763. https://doi.org/10.1016/j.midw.2020.102763
Irish Maternity Indicator System (IMIS) (2016) National Report 2016, Health Service Executive, Clinical Programme for Obstetrics and Gynaecology. Available at: https://www.hse.ie/eng/about/who/acute-hospitals-division/woman-infants/national-reports-on-womens-health/imis-2016-national-report1.pdf
Joint Commissioning Panel for Mental Health (2012) Guidance for commissioners of perinatal mental health services. London, JCP-MH. Available at https://www.jcpmh.info/wp-content/uploads/jcpmh-perinatal-guide.pdf
Jomeen J (2004) The importance of assessing psychological status during pregnancy, childbirth and the postnatal period as a multidimensional construct: a literature review. Clin Eff Nurs 8(3):143–155. https://doi.org/10.1016/j.cein.2005.02.001
Jomeen J (2017) Psychological context of childbirth. Mayes’ Midwifery. Elsevier, London, pp 186–199
Jomeen J, Martin CR (2008) Reflections on the notion of post-natal depression following examination of the scoring pattern of women on the EPDS during pregnancy and in the post-natal period. J Psychiatr Ment Health Nurs 15(8):645–648. https://doi.org/10.1111/j.1365-2850.2008.01282.x
Kimerling R, Baumrind N (2005) Access to specialty mental health services among women in California. Psychiatr Serv 56(6):729–734. https://doi.org/10.1176/appi.ps.56.6.729
Knight M, Bunch K, Tuffnell D, Patel R, Shakespeare J, Kotnis R, Kenyon S, Kurinczuk JJ (eds) on behalf of MBRRACE-UK (2021) Saving lives, improving mothers’ care - lessons learned to inform maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2017–19. National Perinatal Epidemiology Unit, University of Oxford, Oxford
Lee C (2000) Psychology of women’s health: a critique. In: Ussher JM (ed) Women’s Health: Contemporary International Perspectives. British Psychological Society, Leicester
Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui HW, Fong DY (2007) Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet Gynecol 110(5):1102–1112. https://doi.org/10.1097/01.Aog.0000287065.59491.70
Lovibond PF, Lovibond SH (1995a) The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther 33(3):335–343. https://doi.org/10.1016/0005-7967(94)00075-u
Lovibond SH, Lovibond PF (1995b) Manual for the Depression Anxiety Stress Scales, 2nd edn. Psychology Foundation, Sydney
McAuliffe A, Russell NE, Fenton J (2011) Psychological services for women giving birth in a large Irish tertiary referral maternity unit. Psychiatrist 35(3):92–94. https://doi.org/10.1192/pb.bp.109.029165
Meltzer-Brody S, Stuebe A (2014) The long-term psychiatric and medical prognosis of perinatal mental illness. Best Pract Res Clin Obstet Gynaecol 28(1):49–60. https://doi.org/10.1016/j.bpobgyn.2013.08.009
Miller RL, Pallant JF, Negri LM (2006) Anxiety and stress in the postpartum: is there more to postnatal distress than depression? BMC Psychiatry 6:12. https://doi.org/10.1186/1471-244X/6/12
National Collaborating Centre for Mental Health (2007) National Institute for Health and Clinical Excellence: Guidance. In: Antenatal and Postnatal Mental Health: The NICE Guideline on Clinical Management and Service Guidance. British Psychological Society. The British Psychological Society & The Royal College of Psychiatrists, Leicester, UK
Nelson AM (2013) Transition to Motherhood. J Obstet Gynecol Neonatal Nurs 32(4):465–477. https://doi.org/10.1177/0884217503255199
O’Connor TG, Monk C, Burke AS (2016) Maternal affective illness in the perinatal period and child development: findings on developmental timing, mechanisms, and intervention. Curr Psychiatry Rep 18(3):24. https://doi.org/10.1007/s11920-016-0660-y
O’Hara MW, Wisner KL (2014) Perinatal mental illness: definition, description and aetiology. Best Pract Res Clin Obstet Gynaecol 28(1):3–12. https://doi.org/10.1016/j.bpobgyn.2013.09.002
O’Hare MF, Manning E, Corcoran P, Greene RA on behalf of MDE Ireland (2021) Confidential Maternal Enquiry in Ireland, Data Brief No 5. MDE Ireland, Cork
O’Malley D, Higgins A, Begley C, Daly D, Smith V (2018) Prevalence of and risk factors associated with sexual health issues in primiparous women at 6 and 12 months postpartum; a longitudinal prospective cohort study (the MAMMI study). BMC Pregnancy Childbirth 18(1):196. https://doi.org/10.1186/s12884-018-1838-6
O’Malley D, Smith V, Higgins A (2019) Women’s solutioning and strategising in relation to their postpartum sexual health: a qualitative study. Midwifery 77:53–59. https://doi.org/10.1016/j.midw.2019.06.012
Parfitt Y, Ayers S (2014) Transition to parenthood and mental health in first-time parents. Infant Ment Health J 35(3):263–273. https://doi.org/10.1002/imhj.21443
Paschetta E, Berrisford G, Coccia F, Whitmore J, Wood AG, Pretlove S, Ismail KM (2014) Perinatal psychiatric disorders: an overview. Am J Obstet Gynecol 210(6):501-509.e506. https://doi.org/10.1016/j.ajog.2013.10.009
Patton GC, Romaniuk H, Spry E, Coffey C, Olsson C, Doyle LW, Oats J, Hearps S, Carlin JB, Brown S (2015) Prediction of perinatal depression from adolescence and before conception (VIHCS): 20-year prospective cohort study. Lancet 386:875–883. https://doi.org/10.1016/S0140-6736(14)62248-0
Schuurmans C, Kurrasch DM (2013) Neurodevelopmental consequences of maternal distress: what do we really know? Clin Genet 83(2):108–117. https://doi.org/10.1111/cge.12049
Silverman ME, Reichenberg A, Savitz DA, Cnattingius S, Lichtenstein P, Hultman CM, Larsson H, Sandin S (2017) The risk factors for postpartum depression: a population-based study. Depress Anxiety 34(2):178–187. https://doi.org/10.1002/da.22597
Surkan PJ, Kennedy CE, Hurley KM, Black MM (2011) Maternal depression and early childhood growth in developing countries: systematic review and meta-analysis. Bull World Health Organ 89(8):608–615. https://doi.org/10.2471/BLT.11.088187
Togher KL, Treacy E, O’Keeffe GW, Kenny LC (2017) Maternal distress in late pregnancy alters obstetric outcomes and the expression of genes important for placental glucocorticoid signalling. Psychiatry Res 255:7–26
Underwood L, Waldie K, D’Souza S, Peterson ER, Morton S (2016) A review of longitudinal studies on antenatal and postnatal depression. Arch Womens Ment Health 19(5):711–720. https://doi.org/10.1007/s00737-016-0629-1
van der Waerden J, Galéra C, Saurel-Cubizolles MJ, Sutter-Dallay AL, Melchior M (2015) Predictors of persistent maternal depression trajectories in early childhood: results from the EDEN mother-child cohort study in France. Psychol Med 45(9):1999–2012. https://doi.org/10.1017/s003329171500015x
Wenzel A, Haugen EN, Jackson LC, Robinson K (2003) Prevalence of generalized anxiety at eight weeks postpartum. Arch Womens Ment Health 6(1):43–49. https://doi.org/10.1007/s00737-002-0154-2
Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG (2017) A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord 219:86–92. https://doi.org/10.1016/j.jad.2017.05.003
Xavier S, Bento E, Azevedo J, Marques M, Soares MJ, Freitas V, Mota D, Macedo A, Pereira AT (2016) Validation of the Depression, Anxiety and Stress Scale–DASS-21 in a community sample of Portuguese pregnant women. Eur Psychiatry 33:3. https://doi.org/10.1016/J.EURPSY.2016.01.600
Yapp E, Howard LM, Kadicheeni M, Telesia LA, Milgrom J, Trevillion K (2019) A qualitative study of women’s views on the acceptability of being asked about mental health problems at antenatal booking appointments. Midwifery 74:126–133. https://doi.org/10.1016/j.midw.2019.03.021
Yeaton-Massey A, Herrero T (2019) Recognizing maternal mental health disorders: beyond postpartum depression. Curr Opin Obstet Gynecol 31(2):116–119. https://doi.org/10.1097/gco.0000000000000524
Acknowledgements
We thank the midwives and antenatal clinic staff at participating hospitals who helped facilitate the research recruitment, and the women participants who generously shared their time and experiences.
Funding
Open Access funding provided by the IReL Consortium. The MAMMI study was funded by parts of three grants awarded by the Health Research Board (HRB) Ireland [grant numbers HPF/2011/18, HRA_HSR/2012/28, grant HPF-2016–1671]. The current study is funded by Trinity College Dublin’s Provost PhD Scholarship Award 2018 (recipient D. Daly, PhD candidate S. Hannon). These doctoral awards are generously funded through alumni donations and Trinity’s Commercial Revenue Unit. The funders had no participation in any aspect of the study or data analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Research Ethics Committees of Trinity College Dublin and the Ethics committees of the three hospital recruitment sites: Rotunda Hospital Dublin, Coombe Women and Infants University Hospital and Galway University Hospital.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Disclaimer
The funding bodies had no role in relation to the design or conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; decisions for publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hannon, S., Gartland, D., Higgins, A. et al. Maternal mental health in the first year postpartum in a large Irish population cohort: the MAMMI study. Arch Womens Ment Health 25, 641–653 (2022). https://doi.org/10.1007/s00737-022-01231-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-022-01231-x