Abstract
Rapid screening tools are useful for identifying at-risk patients and referring them for further assessment and treatment, but none exist that consider the unique medical needs of pregnant women with eating disorders (EDs). There is a need for a rapid, sensitive, and specific screening tool that can be used to identify a potential ED in pregnancy. We started with a set of 25 questions, developed from our qualitative work along with other ED screening tools, and tested on a development (n = 190) and validation sample (n = 167). Statistical analysis included factor analysis and logistic regressions with ROC curves. Development and validation samples were combined for trimester analysis (n = 357). Refining the tool to 12 items demonstrated strong internal reliability (development alpha = 0.95, validation alpha = 0.91). With correlated errors, questions demonstrated acceptable CFA fit (development: GFI: 0.91, RMSEA: 0.10, NNFI: 0.95; validation: GFI: 0.85, RMSEA: 0.14, NNFI: 0.86). Similar fits were seen by trimester: first trimester n = 127, GFI: 0.89, RMSEA: 0.12, NNFI: 0.94; second trimester n = 150, GFI: 0.83, RMSEA: 0.14, NNFI: 0.88; third trimester n = 80, GFI: 0.99, NNFI: 0.99. Validation against current ED diagnosis demonstrated acceptable sensitivity and specificity using a cutoff of 39 (development sensitivity = 80.7%, specificity = 79.7%, OR = 16.42, 95% CI: 7.51, 35.88; validation sensitivity = 69.2%, specificity = 86.5%, OR: 17.43, 95% CI: 6.46, 47.01). Findings suggest the PEBS tool can reliably and sensitively detect EDs across pregnancy trimesters with 12 questions. A further implication of this work is to reduce health and mental health treatment disparities through this standard and rapid screening measure to ensure early identification and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The impact that eating disorders (EDs) have in pregnancy is considerable, although the best way to identify these disorders during this unique time remains to be determined. Estimates suggest that at least 5% of women experience some type of ED during pregnancy (Linna et al. 2014; Watson et al. 2013), although some estimates are much broader from 0.6 to 27.8% (Broussard 2012; Bye et al. 2020; Easter et al. 2013; Micali et al. 2007; Pettersson et al. 2016; Soares et al. 2009). These estimates reflect some of the challenges in identifying an ED in this population.
Women with EDs are more likely to have unplanned pregnancies, miscarriages, nutritional differences, and an increased risk of postpartum depression and anxiety as opposed to women without eating disorders (Chan et al. 2019; Kimmel et al. 2015; Zerwas & Claydon 2014). Some women with past EDs have similar nutritional patterns during pregnancy as individuals without EDs and many experiences an improvement in nutrition with pregnancy (Dörsam et al. 2019). However, there are some nutritional differences among individuals with a past or active ED which could affect fetal development. Additionally, there is burgeoning epigenetic research to show how modification of the genome can occur prenatally due to malnourishment, which can affect the developing fetus initially and throughout their life (Hoffman et al. 2017; Sebastiani et al. 2020). Identifying women with a current ED, those who are at-risk for developing an ED, and/or those who are at risk to relapse during pregnancy provides an opportunity for early intervention to improve outcomes for the mother and developing fetus.
Among women with infertility, 58% of those who presented with oligomenorrhea or amenorrhea had some form of an ED, none of whom disclosed those to their providers (Bruneau et al., 2017; Linna et al. 2014). This is consistent with recent qualitative evidence which suggests that many pregnant women with EDs during pregnancy or with a history of an ED do not feel comfortable disclosing information about their ED with their healthcare providers (Claydon et al., 2018). Other qualitative work on this topic indicates several barriers for identifying EDs during pregnancy which reinforce issues of stigma as well as limits to professional training (Bye et al. 2018). Additionally, most medical professionals are not well-trained in identifying pregnant women who may have an ED or clinically significant ED symptomatology unless they are in the psychiatry discipline or have taken continuing medical education specific to EDs (Anderson et al. 2017; Leddy et al. 2009). There is minimal training on EDs for medical professionals outside of the psychiatry specialty (Mahr et al., 2014), leaving most medical professionals who interact with pregnant women with limited knowledge on how to identify and help these patients.
To fill the gap with identification, rapid screening tools can be useful to assist with early screening. These rapid screening tools can assist in identifying at-risk patients, but currently, there are none that consider the unique characteristics and situation of pregnant women with EDs. The SCOFF is a five-item simple clinical tool used to identify a potential case of anorexia nervosa (AN) or bulimia nervosa (BN), but it is not validated in pregnancy (Morgan et al. 2013). Recent research has suggested that when used in a pregnant population, it can provide false positives, which has resulted in an expert consensus that the SCOFF is not the ideal tool for use in these populations (Bannatyne et al. 2018; Baudet et al. 2013). Currently, the Eating Disorder Examination Questionnaire (EDE-Q; Fairburn 2008) has the most psychometric data available in pregnancy but needs further validation and is too lengthy with 28 questions (Bannatyne et al. 2019).
Given those concerns, a few researchers have tried to adapt current measures such as the SCOFF (Hubin-Gayte and Squires 2012) or the EDE (Bannatyne et al. 2018) for use in a pregnant population. One revised version of the SCOFF used in a French pregnant population tried separating the SCOFF questions into pre-pregnancy and during pregnancy categories to identify and understand antenatal ED symptoms (Hubin-Gayte and Squires 2012). However, this method does not truly capture ED symptoms accurately during pregnancy (the time when both mother and developing fetus are at risk), and limited psychometrics were reported in the study. The adaptation of the EDE for pregnancy, known as the EDE-PV, had adequate internal reliability (0.59–0.67 for subscales) in a population of pregnant women who were overweight and/or obese (Bannatyne et al. 2018; Emery et al. 2017). However, the EDE-PV is a structured interview with multiple sections and is better for use as a full assessment, rather than for quick clinical identification. The EDE-PV has also not been validated in pregnant women who are under a BMI of 30 (Emery et al. 2017). But the use of BMI during pregnancy has been a topic of debate and it appears that is more accurate in the first trimester as the pregnancy progresses there are some other physiologic changes that may affect this parameter (Louise et al. 2020).
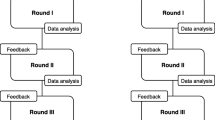
The aim of this study was to determine the psychometric properties for the Prenatal Eating Behaviors Screening (PEBS) Tool, which was created to address these concerns. The goal of this tool was to be rapid (less than 5 min to complete), applicable to most common EDs in pregnancy [AN, BN, binge eating disorder (BED), and other specified feeding and eating disorders (OSFED)], and valid across the span of pregnancy (all three trimesters). This was accomplished using large validation and development samples and making use of experts in both medical and ED research fields. Once validation was shown, the goal is for the Prenatal Eating Behaviors Screening (PEBS) Tool to be used as a rapid screen tool to identify pregnant women at risk in order to refer them for a specialist for further assessment.
Methods
PEBS item development
A series of questions were included from existing sources (e.g., EDE-Q, Fairburn 2008; SCOFF, Morgan et al. 1999; EDI-3, Clausen et al. 2011) and from pilot data themes from a previous study (Claydon et al. 2018). An initial list of 34 questions were combined into a single framework and reviewed by content experts, with an eye towards (1) adapting or using language to be appropriate for terms that should be used or avoided in the ED field (e.g., using person-first language; Weissman et al. 2016), (2) adapting or using language appropriate for women throughout their pregnancy (e.g., removing items that looked for a certain amount of weight loss over several months), and (3) making items follow similar Likert type patterns of responses for ease of respondent use (e.g., using “you” for stem, checking for consistency in “strongly agree” to “strongly disagree” in responses). Finally, questions were checked to ensure all four types of ED symptomology were represented by a content expert, and then a total of 9 questions were dropped for redundancy reasons. A final set of 25 questions underwent further piloting by a small sample (n = 3) of pregnant women with a diagnosed ED or history of an ED to check for face validity, accuracy in wording, and question interpretation by questioning relevance, language sensitivity, and accuracy as they filled out the study; all 25 items were then included in the development and validation samples. Supplemental Table 1 has the full list of 25 items along with a number of women responding to each Likert-type response for both samples.
Self-report ED diagnoses
As part of the survey, participants were asked to self-report whether they had ever been diagnosed with an eating disorder. If they selected yes, they were asked “Which eating disorders have you had” and could select any of the following: AN, BED, BN, or OSFED, formerly known as eating disorders not otherwise specified (EDNOS). Participants responded to each of those prompts by selecting: current professional diagnosis, past professional diagnosis, current self-diagnosis, or past self-diagnosis (see Appendix 1 for the complete survey). They were allowed to choose more than one answer in each category. Self-report ED diagnoses have been shown to be adequate in detecting current and lifetime AN and BN as measured by diagnostic interviews (Keski-Rahkonen et al. 2006). Participants were counted as having a current diagnosis (yes) if they selected either current professional diagnosis and/or current self-diagnosis for any of the four ED types. These current self-reported diagnoses were used because it was not feasible for the scope of a psychometric study to conduct full diagnostic interviews on all participants.
Pregnancy trimester
Pregnancy trimester was assessed by a self-reported week of pregnancy and categorized as first trimester, weeks 4–13; second trimester, weeks 14–27; and third trimester, weeks 28–40.
Participants
Two separate samples were collected for this study. The development sample was collected first via Amazon Mechanical Turk (MTurk, an online crowdsourcing site to complete tasks virtually), and online mother and pregnancy groups with an IRB-approved advertisement (see Appendix 2). This included 271 responses recorded between August 2020 and November 2020. Next, the validation sample was collected via SurveyCircle (an online survey exchange platform), a second MTurk sample excluding “super users”, and online mother and pregnancy groups and included 236 responses recorded between October 2020 and March 2021. Sample collection methods differed slightly based on including additional exclusions in MTurk sampling following recommendations from Litman and Robinson (2021) and then extending sampling to SurveyCircle to allow for additional responses in the validation sample. All participants were recruited from online groups based in North America or the UK; SurveyCircle has geographic constraints which were enabled to similarly draw from participants in North America and the UK. Although we did not ask about geographic location, other studies suggest the majority of users on MTurk are from the USA (75%) with India second at 16%, and Canada third at 1.1% (Difallah et al., 2018; Moss et al. 2020). A final restriction of English-language proficiency to complete this survey suggests that the majority of the sample are likely located in North America and the UK.
Human subjects
This study was filed with the referent university’s Institutional Review Board and exempt status was acknowledged (IRB#: 2003925385). Qualtrics software was used to host and distribute the survey and no protected health information (PHI) was obtained.
Data quality checks
Both datasets underwent a series of data quality checks to eliminate possible “bot” submissions and other data quality problems. First, cases were eliminated if they did not list the weeks pregnant as a number between 4 and 40 (development n = 67, validation n = 55). The weeks pregnant were selected as the initial restriction as it is a sample requirement that only pregnant women be included. This pregnancy week selection eliminated those not pregnant, unsure about pregnant status, and probable “bot” included but unlikely values (e.g., 80). Next, cases were eliminated if they did not complete at least 90% of the survey (development n = 9, validation n = 9). This was part of the decision tree because those cases would be dropped via pairwise deletion if they did not fill out the final 25 survey questions related to the eating disorder tool. Finally, cases were eliminated if they completed the survey in under 2 min (development n = 5, validation n = 5); this is assuming a loss of comprehension when reading speed exceeded 15 words per second. Final datasets included n = 190 (70.1%) for development, and n = 167 (70.8%) for validation. These response rates after quality control are consistent, if not higher with what is being seen for MTurk and other online survey platforms (Kennedy et al. 2020; Nayak and Narayan 2019). All analyses were conducted with SAS software, version 9.4 (SAS Institute, Inc. 2013).
Results
Development
Analyses were conducted first on the development dataset (n = 190). The goal of the developmental dataset was data reduction (to reduce from 25 items to a minimum number of items to accurately screen pregnant women for an ED) with a focus on relationship with current ED diagnosis. Within the development sample, the majority were 25–34 years old (n = 104; 54.74%), married (n = 164; 86.32%), White (n = 140; 74.07%), and had private insurance (n = 129; 67.89%). The mean week of pregnancy was 19.26 (SD = 10.61), and 30.0% had a current ED diagnosis (n = 57). Full descriptive statistics and demographic characteristics of the sample are presented in Table 1.
Internal reliability
Cronbach’s alpha was used to ensure the 25 items were consistent and had internal reliability; item correlations below 0.60 were first considered as possible for deletion. Five items were below 0.20, and another three below 0.60.
Relationship with current ED diagnosis
Each of the 25 items was then examined using non-parametric Mann–Whitney tests against self-reported current ED diagnosis (Table 2). The five items with the lowest internal consistency also did not have a statistically significant relationship with current ED diagnosis, alpha set to 0.05. Two items with modest internal reliability (below 0.60) had statistically significant but more modest relationships (p-values between 0.002 and 0.005) relative to the other items. All other items p < 0.0001.
Exploratory factor analysis
Next, a polychoric correlation matrix was output from the 25 items and used for all further factor analyses. First, exploratory factor analysis (EFA) was run with squared multiple correlation (smc) priors and full information maximum likelihood method, with a one and then two factor solution. Single factor with all items demonstrated best fit (Table 2: 64% variability, Tucker and Lewis: 0.58, AIC: 1553.86). Factor loadings below 0.70 were then removed, and another EFA run with a single factor on the final 12 items, resulting in significantly improved model fit (94% variance explained, Tucker and Lewis: 0.88, AIC: 183.55, all factor loadings above 0.72.)
Confirmatory factor analysis
EFA results guided CFA models, starting with a single factor solution, and then adding correlated errors of items related by ED diagnosis, and then substituting a second factor for ED diagnosis, all on the polychoric matrix of the items. The best fitting model was the single factor solution with correlated errors and is presented in Table 3. All factor loadings p < 0.0001. Final model included eight correlated errors, including three correlated errors pertaining to items related to BN, three correlated errors related to items about BED, and two sets of correlated errors for AN items (see Supplemental Path Diagram Figure A1 for correlated error terms). With correlated errors, questions demonstrated acceptable model fit (e.g., GFI: 0.91, RMSEA: 0.10, NNFI: 0.95).
Final scale clinical cutoff score and validation against current ED diagnosis
The final 12-item scale demonstrated excellent internal reliability, Cronbach’s alpha = 0.95. Items were summed and ranged from 12 to 60, M = 32.48 (SD = 13.9). Those with current ED diagnosis (n = 57, M = 45.63, SD = 8.4) had higher scores against all other participants (n = 133, M = 26.85, SD = 11.9), t (df = 188) = 12.37, p < 0.0001. Using logistic regression with receiver operating characteristic curve on current ED diagnosis, we found increased odds of 1.16 (Wald 95% CL 1.11, 1.21) for each point increase in the summed score, Table 3. A cutoff of 39 had good sensitivity (80.7%) and specificity (79.7%) for detecting current ED diagnosis, with an AUC of 0.88 (Fig. 1a). Those with a score of 39 or greater had 16.42 increased odds of having a current ED diagnosis relative to those with a score below 39. The final scale can be found in Appendix 3. Lower cutoffs could be used in order to maximize sensitivity over specificity. For example, a cutoff score of 34 gives a sensitivity of 89.5%, but reduces specificity to 71.4%. Using this cutoff results in N = 73, 38.4% of the sample as being identified by the screening tool, resulting in a similar OR of 16.4.
Validation
Final scale reliability and CFA were replicated with the smaller validation sample (n = 167), using the same cutoff of 39 found in the developmental dataset. The validation sample looked similar to the development sample. A majority of the sample were 25–34 years old (n = 91; 54.49%), married (n = 96; 57.49%), White (n = 107; 64.07%), and had private insurance (n = 90; 53.89%). The mean week of pregnancy was 18.91 (SD = 9.06), and 15.6% had a current ED diagnosis (n = 26).
The 12-item scale demonstrated slightly attenuated but still excellent internal reliability, Cronbach’s alpha = 0.91. Model fit statistics of the CFA on the polychoric matrix attenuated (Table 3); three items standardized factor loading dropped below the preferred 0.60 although all p-values remained significant. Although some model fit indicators also dropped below preferred values (e.g., RMSEA), generally acceptable model fit was also found for the validation model (i.e., GFI: 0.85, RMSEA: 0.14, NNFI: 0.86). Logistic regression indicated well-fitting sensitivity (69.2%) and specificity (86.5%) with the new sample at the same cutoff value of 39, with an AUC of 0.88 (Fig. 1b).
Trimester
Next, we wished to ascertain that the model would work for each trimester of pregnancy. Due to small samples within trimesters, the development and validation samples were combined for this analysis and then stratified by trimester. Due to the small sample for the third trimester, a different method (ULS) for the CFA was used, and thus, some estimates are not available. The polychoric correlation matrix by trimester was used for all factor analyses. Generally acceptable model fit indices were found (first trimester n = 127, GFI: 0.89, RMSEA: 0.12, NNFI: 0.94; second trimester n = 150, GFI: 0.83, RMSEA: 0.14, NNFI: 0.88; third trimester n = 80, GFI: 0.99, NNFI: 0.99). AUC against current ED diagnosis ranged from 0.85 to 0.89 (Fig. 2). Sensitivity (67.9 to 77.8%) and specificity (79.3 to 85.7%) were also acceptable with the cutoff score of 39 and retained increased odds of having a current ED diagnosis relative to a score below 39 (OR range: 13.64 to 17.68).
Discussion
The findings from this research suggest the PEBS tool can reliably and sensitively detect EDs in pregnancy with only 12 questions. This would provide a rapid initial screen to allow clinicians to refer women for further assessment. The American College of Obstetricians and Gynecologists (ACOG) in their practice bulletin 740 states that health care providers should be comfortable screening and recognizing patients with eating disorders. Still, only a professional expert should make the final diagnosis (ACOG 2018). It is well known that patients with eating disorders are at risk of having higher rates of anxiety and postpartum depression and babies with a small fetal head circumference (Kimmel et al. 2016). Universal screening for ED in pregnancy has not been established or recommended by professional organizations, although it has been acknowledged that there are clinical management strategies that are currently missing (Paslakis and Zwaan 2019). Considering that many patients with eating disorders engage in weight cycling, clinicians may focus on those groups during pregnancy (Marchesini et al. 2004). Applying the PEBS tool to those patients at the highest risk, could represent an opportunity for clinicians to identify a potential ED in pregnancy. Identifying EDs during pregnancy may allow for appropriate referrals to mental health providers, physicians, and registered dietitians to improve women’s psychological and physical well-being during pregnancy and promote better maternal and child health outcomes.
Strengths and limitations
The final PEBS tool with 12 items meets clinical recommendations, suggesting that brief screening instruments contain 15 items or less and use a simple cutoff score (Marquer et al. 2012). This allows the tool to be easily used by clinicians who have limited time with patients. Additionally, this screening tool was tested on a large sample of pregnant women across all trimesters.
There are some limitations inherent in the methodology which are important to note. First, the sample collected were only English-speaking since the tool is designed to be validated in English first. Therefore, the PEBS tool may not be culturally or linguistically appropriate in all populations and will need to be tailored and translated as needed. Second, convenience sampling was employed which has biases based on that sampling technique. Third, the data collection for the development and validation sample was conducted at slightly different time points, although within a few months of each other. Fourth, there was a smaller sample gathered for the third trimester, which gives us less information on how the tool works relative to the first two trimesters, although there is still sound psychometric data for the third trimester. All model fits ranged from acceptable to good. However, future studies may consider more stringent model fit criteria. Fifth, our final alpha coefficients are high (above 0.90), which raises some question about scale homogeneity at the expense of content coverage and validity (Streiner 2003). However, we believe that we addressed this concern by having content experts review the final 12 items to ensure that we incorporated symptomatology in the final questions that demonstrated the multifaceted nature of the breadth of eating disorders. Sixth, we did not conduct diagnostic interviews with participants to gather their current and past ED diagnoses, but instead asked for self-report of self and professional diagnoses. Comparison with a diagnostic tool would be ideal, but self-reported diagnoses have been shown to be a good indicator of current and lifetime ED diagnoses (Keski-Rahkonen et al. 2006). Additionally, survey collection was conducted during the COVID-19 pandemic and for the safety of participants, an online survey was deemed to be most appropriate. One diagnostic online survey assessment possibility is the digital version of the eating disorder assessment for DSM-5 (EDA-5; Sysko et al. 2015). However, the EDA-5 takes approximately 20–30 min to complete, significantly adding to participant burden and reducing the likelihood of obtaining a large enough sample for meaningful results. Finally, the PEBS tool may screen positive for women with a prior ED, but who are currently in recovery. However, the sensitivity and specificity are high for the PEBS tool, which indicates that women are being identified based on their current risk.
Future research and conclusions
One of the most critical aspects of research is the translation, in order to ensure that the information gathered is made applicable and available to the people that it can help the most. To that end, following this publication, informational booklets on how to use the PEBS tool will be made available to clinicians, along with referral resources. This will bridge the research-practice gap that perpetuates incremental change rather than allowing for broad dissemination of results. Additionally, a feasibility study will be conducted in order to see how the 12 item PEBS tool works in a clinical setting. To address the limitations of self-report diagnoses, this follow-up study will utilize a smaller confirmatory sample with diagnostic interviews for EDs. A pencil/paper and online version of the PEBS tool have also been created to allow for further ease of dissemination and use. Additionally, future research will have to tailor and translate this tool so that it can be more linguistically and culturally appropriate for diverse populations. A further implication of this work is to reduce health and mental health treatment disparities in pregnant women through this standard and rapid screening measure to ensure early identification and treatment.
Data availability
Data and materials are available upon reasonable request from the authors.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
ACOG Committee Opinion No (2018) 740: Gynecologic care for adolescents and young women with eating disorders. Obstet Gynecol 131(6):e205–e213. https://doi.org/10.1097/AOG.0000000000002652
Anderson K, Accurso EC, Kinasz KR, Le Grange D (2017) Residents’ and fellows’ knowledge and attitudes about eating disorders at an academic medical center. Acad Psychiatry 41(3):381–384. https://doi.org/10.1007/s40596-016-0578-z
Bannatyne AJ, Hughes R, Stapleton P, Watt B, MacKenzie-Shalders K (2018) Signs and symptoms of disordered eating in pregnancy: a Delphi consensus study. BMC Pregnancy and Childbirth 18(1). https://doi.org/10.1186/s12884-018-1849-3
Bannatyne, A. J., McNeil, E., Stapleton, P., MacKenzie-Shalders, K., & Watt, B. (2019). Disordered eating measures validated in pregnancy samples: a systematic review. Eating Disorders, 1–26. https://doi.org/10.1080/10640266.2019.1663478
Baudet ML, Montastier E, Mesthe P, Oustric S, Lepage B, Ritz P (2013). The SCOFF score: a screening tool for eating disorders in family practice. e-SPEN Journal 8(3):e86–e89. https://doi.org/10.1016/j.clnme.2013.03.001
Broussard B (2012) Psychological and behavioral traits associated with eating disorders and pregnancy: a pilot study. J Midwifery Womens Health 57(1):61–66. https://doi.org/10.1111/j.1542-2011.2011.00089.x
Bruneau M, Colombel A, Mirallié S, Fréour T, Hardouin J-B, Barrière P, Grall-Bronnec M (2017) Desire for a child and eating disorders in women seeking infertility treatment. PLOS ONE 12(6). https://doi.org/10.1371/journal.pone.0178848
Bye A, Shawe J, Bick D, Easter A, Kash-Macdonald M, Micali N (2018) Barriers to identifying eating disorders in pregnancy and in the postnatal period: a qualitative approach. BMC Pregnancy Childbirth 18(1):1–10. https://doi.org/10.1186/s12884-018-1745-x
Bye A, Nath S, Ryan EG, Bick D, Easter A, Howard LM, Micali N (2020) Prevalence and clinical characterisation of pregnant women with eating disorders. European Eating Disorders Review : the Journal of the Eating Disorders Association 28(2):141–155. https://doi.org/10.1002/erv.2719
Chan CY, Lee AM, Koh YW, Lam SK, Lee CP, Leung KY, Tang CS (2019) Course, risk factors, and adverse outcomes of disordered eating in pregnancy. Int J Eat Disord 52(6):652–658. https://doi.org/10.1002/eat.23065
Clausen L, Rosenvinge JH, Friborg O, Rokkedal K (2011) Validating the eating disorder inventory-3 (EDI-3): a comparison between 561 female eating disorders patients and 878 females from the general population. J Psychopathol Behav Assess 33(1):101–110. https://doi.org/10.1007/s10862-010-9207-4
Claydon EA, Davidov DM, Zullig KJ, Lilly CL, Cottrell L, Zerwas SC (2018) Waking up every day in a body that is not yours: a qualitative research inquiry into the intersection between eating disorders and pregnancy. BMC Pregnancy Childbirth 18(463):1–13. https://doi.org/10.1186/s12884-018-2105-6
Difallah D, Filatova E, Ipeirotis P (2018) Demographics and dynamics of mechanical Turk workers. In Proceedings of the Eleventh ACM International Conference on Web Search and Data Mining (WSDM ’18). Association for computing machinery, New York, NY, US. 135–143. https://doi.org/10.1145/3159661
Dörsam AF, Preißl H, Micali N, Lörcher SB, Zipfel S, Giel KE (2019) The impact of maternal eating disorders on dietary intake and eating patterns during pregnancy: a systematic review. Nutrients 11(4):840. https://doi.org/10.3390/nu11040840
Easter A, Bye A, Taborelli E, Corfield F, Schmidt U, Treasure J, Micali N (2013) Recognising the symptoms: how common are eating disorders in pregnancy? Eur Eat Disord Rev 21(4):340–344. https://doi.org/10.1002/erv.2229
Emery RL, Grace JL, Kolko RP, Levine MD (2017) Adapting the eating disorder examination for use during pregnancy: preliminary results from a community sample of women with overweight and obesity. Int J Eat Disord 50(5):597–601. https://doi.org/10.1002/eat.22646
Fairburn CG (2008) Eating disorder examination questionnaire (EDE-Q 6.0). In: Cognitive behavior therapy and eating disorders (pp. 309–313). New York: Guilford Press
Hoffman DJ, Reynolds RM, Hardy DB (2017) Developmental origins of health and disease: current knowledge and potential mechanisms. Nutr Rev 75(12):951–970. https://doi.org/10.1093/nutrit/nux053
Hubin-Gayte M, Squires C (2012) Étude de l’impact de la grossesse sur les comportements alimentaires à travers l’utilisation du questionnaire SCOFF. L’evolution Psychiatrique 77:201–212. https://doi.org/10.1016/j.evopsy.2012.01.002
Kennedy R, Clifford S, Burleigh T, Waggoner P, Jewell R, Winter N (2020) The shape of and solutions to the MTurk quality crisis. Polit Sci Res Methods 8(4):614–629. https://doi.org/10.1017/psrm.2020.6
Keski-Rahkonen A, Sihvola E, Raevuori A, Kaukoranta J, Bulik CM, Hoek HW, Rissanen A, Kaprio J (2006) Reliability of self-reported eating disorders: optimizing population screening. Int J Eat Disord 39(8):754–762. https://doi.org/10.1002/eat.20277
Kimmel MC, Ferguson EH, Zerwas S, Bulik CM, Meltzer-Brody S (2015) Obstetric and gynecologic problems associated with eating disorders. Int J Eat Disord 49(3):260–275. https://doi.org/10.1002/eat.22483
Zerwas S, Claydon E (2014). Eating disorders across the lifespan: from menstruation to menopause. In D. L. Barnes (Ed.), Women's reproductive mental health across the lifespan (pp. 237–261). Springer International Publishing. https://doi.org/10.1007/978-3-319-05116-1_13
Kimmel MC, Ferguson EH, Zerwas S, Bulik CM, Meltzer-Brody S (2016) Obstetric and gynecologic problems associated with eating disorders. nt J Eat Disord 49(3):260–275. https://doi.org/10.1002/eat.22483
Leddy MA, Jones C, Morgan MA, Schulkin J (2009) Eating disorders and obstetric-gynecologic care. J Womens Health 18(9):1395–1401. https://doi.org/10.1089/jwh.2008.1183
Linna MS, Raevuori A, Haukka J, Suvisaari JM, Suokas JT, Gissler M (2014) Pregnancy, obstetric, and perinatal health outcomes in eating disorders. American Journal of Obstetrics and Gynecology 211(4):392-el-392.e8. https://doi.org/10.1016/j.ajog.2014.03.067
Litman L, Robinson J (2021) Conducting online research on Amazon Mechanical Turk and beyond. Sage Publications
Louise J, Deussen AR, Dodd JM (2020) Gestational weight gain-re-examining the current paradigm. Nutrients 12(8):2314. https://doi.org/10.3390/nu12082314
Marchesini G, Cuzzolaro M, Mannucci E, Grave RD, Gennaro M, Tomasi F, Barantani EG, Melchionda N (2004) Weight cycling in treatment-seeking obese persons: data from the Quovadis Study. Int J Obes 28(11):1456–1462. https://doi.org/10.1038/sj.ijo.0802741
Mahr F, Farahmand P, Bixler EO, Domen RE, Moser EM, Nadeem T, Levine RL, Halmi KA (2014) A national survey of eating disorder training. Int J Eat Disord 48(4):443–445. https://doi.org/10.1002/eat.22335
Marquer C, Barry C, Mouchenik Y, Hustache S, Djibo DM, Manzo ML, Falissard B, Révah-Lévy A, Grais RF, Moro M.-R (2012) A rapid screening tool for psychological distress in children 3–6years old: results of a validation study. BMC Psychiatry 12(170). https://doi.org/10.1186/1471-244x-12-170
Micali N, Treasure J, Simonoff E (2007) Eating disorders symptoms in pregnancy: a longitudinal study of women with recent and past eating disorders and obesity. J Psychosom Res 63(3):297–303. https://doi.org/10.1016/j.jpsychores.2007.05.003
Morgan JF, Reid F, Lacey JH (1999) The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ 319(7223):1467–1468. https://doi.org/10.1136/bmj.319.7223.1467
Moss AJ, Rosenzweig C, Robinson J, Litman L (2020) Demographic stability on mechanical Turk despite COVID-19. Trends Cogn Sci 24(9):678–680. https://doi.org/10.1016/j.tics.2020.05.014
Nayak MSDP, Narayan KA (2019) Strengths and weaknesses of online sureys. IOSR Journal of Humanities and Social Sciences (IOSR-JHSS) 5(5):31–38. https://doi.org/10.9790/0837-2405053138
Paslakis G, Zwaan M (2019) Clinical management of females seeking fertility treatment and of pregnant females with eating disorders. Eur Eat Disord Rev 27(3):215–223. https://doi.org/10.1002/erv.2667
Weissman RS, Becker AE, Bulik CM, Frank GKW, Klump KL, Steiger H, Strober M, Thomas J, Waller G, Walsh BT (2016) Speaking of that: terms to avoid or reconsider in the eating disorders field. Int J Eat Disord 49(4):349–353. https://doi.org/10.1002/eat.22528
Pettersson CB, Zandian M, Clinton D (2016) Eating disorder symptoms pre- and postpartum. Arch Womens Ment Health 19(4):675–680. https://doi.org/10.1007/s00737-016-0619-3
SAS (2013) Statistical analysis software. Users’ guide statistics version 9.4. SAS Institute Inc., Cary
Sebastiani G, Andreu-Fernández V, HerranzBarbero A, Aldecoa-Bilbao V, Miracle X, MelerBarrabes E, Balada Ibañez A, Astals-Vizcaino M, Ferrero-Martínez S, Gómez-Roig MD, García-Algar O (2020) Eating disorders during gestation: implications for mother’s health, fetal outcomes, and epigenetic changes. Front Pediatr 8:587. https://doi.org/10.3389/fped.2020.00587
Soares RM, Nunes MA, Schmidt MI, Giacomello A, Manzolli P, Camey S, Buss C, Drehmer M, Melere C, Hoffman J, Ozcariz S, Manenti CN, Pinheiro AP, Duncan BB (2009) Inappropriate eating behaviors during pregnancy: prevalence and associated factors among pregnant women attending primary care in southern Brazil. Int J Eat Disord 42(5):387–393. https://doi.org/10.1002/eat.20643
Watson H, Von Holle A, Hamer R, Knoph Berg C, Torgersen L, Magnus P, Bulik C (2013) Remission, continuation and incidence of eating disorders during early pregnancy: a validation study in a population-based birth cohort. Psychol Med 43(8):1723–1734. https://doi.org/10.1017/S0033291712002516
Streiner DL (2003) Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess 80(1):99–103
Sysko R, Glasofer DR, Hildebrandt T, Klimek P, Mitchell JE, Berg KC, Peterson CB, Wonderlich SA, Walsh BT (2015) The eating disorder assessment for DSM-5 (EDA-5): development and validation of a structured interview for feeding and eating disorders. Int J Eat Disord 48(5):452–463. https://doi.org/10.1002/eat.22388
Acknowledgements
With gratitude and appreciation to Seneca Demoss-Jennings and Kelsi Taylor who assisted with initial questionnaire development. An additional sincere note of appreciation to Kristin Ranson who helped to develop a visual version of the tool included in Appendix 3 that can be disseminated to the public and clinicians.
Funding
The Ophelia Fund/Rhode Island Foundation helped to fund the creation of a version of the tool which is included in the paper and for dissemination to clinicians after. Research reported in this publication was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number 5U54GM104942-05.
Author information
Authors and Affiliations
Contributions
EC developed the study idea, oversaw the study process, developed the screening tool in conjunction with CL (and student research support in acknowledgments), recruited participants, and wrote the manuscript along with CL, JC, and ODG. CL co-developed the screening tool with EC, planned and conducted the analyses, and interpreted and wrote up the results, tables, and figures, as well as reviewed the entirety of the paper. JC assisted with managing data, developing tables, conducting and assisting with writing the literature review, and reviewing the entirety of the paper. ODG provided the clinical expertise that was necessary to highlight the relevance of this screening tool to obstetricians and the population they serve; ODG added this to the introduction and discussion as well as providing insight on and reviewing the entirety of the paper.
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Claydon, E.A., Lilly, C.L., Ceglar, J.X. et al. Development and validation across trimester of the Prenatal Eating Behaviors Screening tool. Arch Womens Ment Health 25, 705–716 (2022). https://doi.org/10.1007/s00737-022-01230-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-022-01230-y