Abstract
Studies in high-income countries (HICs) have shown that variability in maternal-fetal attachment (MFA) predict important maternal health and child outcomes. However, the validity of MFA ratings in low- and middle-income countries (LMICs) remains unknown. Addressing this gap, we assessed measurement invariance to test the conceptual equivalence of the Prenatal Attachment Inventory (PAI: Muller, 1993) across eight LMICs. Our aim was to determine whether the PAI yields similar information from pregnant women across different cultural contexts. We administered the 18-item PAI to 1181 mothers in the third trimester (Mean age = 28.27 years old, SD = 5.81 years, range = 18–48 years) expecting their first infant (n = 359) or a later-born infant (n = 820) as part of a prospective birth cohort study involving eight middle-income countries: Ghana, Jamaica, Pakistan, Philippines, Romania, South Africa, Sri Lanka and Vietnam. We used Multiple Group Confirmatory Factor Analyses to assess across-site measurement invariance. A single latent factor with partial measurement invariance was found across all sites except Pakistan. Group comparisons showed that mean levels of MFA were lowest for expectant mothers in Vietnam and highest for expectant mothers in Sri Lanka. MFA was higher in first-time mothers than in mothers expecting a later-born child. The PAI yields similar information about MFA across culturally distinct middle-income countries. These findings strengthen confidence in the use of the tool across different settings; future studies should explore the use of the PAI as a screen for maternal behaviour that place children at risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Postpartum depression (PPD) is a key area of research in the field of maternal and child health (Field 2010), and research is increasingly recognising the crucial importance of pregnancy as a period of potential risk and opportunity for intervention. However, research on maternal psychological health has scarcely been conducted outside of high-income countries (HICs) (known as the 10/90 gap; COHRED 1990; Henrich et al. 2010). That said, reviews that have focused on research in low- and middle-income countries (LMICs) have demonstrate that prenatal stress is as strongly associated with adverse infant outcomes as in HICs (Buffa et al. 2018; Parsons et al. 2012) and that rates of PPD often exceed those reported for HICs (e.g. Fisher et al. 2012; Woody et al. 2017). Given this, it is critically important to test the universality of processes underlying maternal and infant mental health in culturally and economically diverse contexts, as outcomes differ crucially across contexts (Vidyasagar 2006).
One area of focus, as illustrated in a recent systematic review (Tichelman et al. 2019), has been the role of maternal-fetal attachment (MFA)—defined as the strength of mothers’ emotional ties with the fetus (and also known as prenatal bonding; Walsh 2010). MFA assessments capture variability in expectant mothers’ behaviours, cognitions and emotions towards the fetus, which appear important for positive prenatal health practices such as giving up smoking (e.g. Lindgren 2001), attending clinics and exercising regularly (Cinar et al. 2017). In a meta-analysis of 14 studies that both spanned prenatal and postnatal periods and included direct observational ratings of parent-infant interactions, Foley and Hughes (2018) found that MFA predicted caregiver sensitivity in interactions with their infant, which is a potent influence on children’s cognitive and socio-emotional development (Mills-Koonce et al. 2015). Thus, valid measurement of MFA has potentially far-reaching clinical implications for the health of both mothers and infants (Laxton-Kane and Slade 2002).
Predictors of MFA include gestational age (Yarcheski et al. 2009), good maternal mental health (Rollè et al. 2020), social support and first pregnancy (Tichelman et al. 2019). In contrast, MFA appears unrelated to demographics (e.g., education, age, marital status), fertility treatment, fetal defects or planned pregnancies (Tichelman et al. 2019). In a systematic review of 41 studies, Rollè et al. (2020) showed that treatment for depression can improve MFA. However, this research field is limited by its narrow focus on parents (mainly mothers) living in HICs (Brandon et al. 2009). For example, all but two of the 77 studies included in Tichelman et al.’s (2019) review were from HICs.
Of the two MFA studies with LMIC samples included in Tichelman et al.’s (2019) review, the first involved 672 mothers in rural Bangladesh. Edhborg et al. (2011) found prenatal MFA (assessed via a translation of the widely used Prenatal Attachment Inventory; PAI: Muller 1993) was positively associated with bonding when the infant was 2–3 months old and negatively associated with PPD symptoms. In the second study, Lingeswaran and Bindu (2012) assessed the feasibility of measuring MFA in India with a sample of 230 pregnant women using the Maternal-Fetal Assessment Scale (MFAS; Cranley 1981). Their findings showed average MFA scores (M = 87.43, SD = 10) were at the lower end of the range (minimum 70–maximum 114), which the authors interpreted as reflecting social and economic restrictions on women’s ability to develop a relationship with the fetus, coupled with a cultural emphasis upon birth rather than pregnancy. However, another study in India (not included in Tichelman et al. 2019) found no association between PAI scores and depression in gestational surrogates or matched controls (Lamba et al. 2018). Existing findings therefore paint a mixed picture regarding the construct validity of the PAI in LMICs. Furthermore, in both the Bangladeshi and Indian samples, the Cronbach’s alpha was lower than for English versions and included no further psychometric analysis of the questionnaires.
Punamäki et al. (2017) asked 511 expectant Palestinian mothers living in Gaza to complete the PAI. They reported that lack of social support mediated the association between war trauma and reduced MFA, but found MFA was unrelated to PPD. Given the scarcity of research on MFA in LMICs, it is difficult to judge whether this lack of association reflects the particular challenges of living in a war zone, a more general contrast in the salience of MFA across resource settings or cultural differences in the meaning or validity of the instruments used (note Punamäki et al. (2017) were unable to replicate the established PAI factor structure).
A key step in evaluating the conceptual equivalence of MFA ratings across different contexts is to construct latent factor models and test for measurement invariance across groups. That is, assessing whether a tool shows an equivalent structure and meaning across distinct groups. Theoretically, assessing whether an instrument yields similar information in different LMICs is necessary to test the cultural universality of inferences about specific causal pathways. Practically, demonstrating across-site equivalence is useful in establishing whether similar or distinct methods of identifying at-risk individuals should be used across settings.
The current study first aimed to assess the conceptual and measurement equivalence of the PAI across eight LMICs in widely different global regions. By testing for measurement invariance across eight LMICs, we aim to establish whether PAI items capture variation in how MFA is manifest across different groups. Finally, if measurement invariance is established, our next two aims were to compare mean levels of MFA across site and birth parity.
Methods
Participants
Trained female fieldworkers invited women attending antenatal appointments to participate in Evidence for Better Lives Study – Foundational Research (EBLS-FR), a prospective birth cohort study in eight different sites (N = 1208) that represent distinct social and cultural conditions across major world regions: Koforidua (Ghana, n = 150), Kingston (Jamaica, n = 152), Tarlai Kalan (Pakistan, n = 150), Valenzuela (Philippines, n = 154), Cluj-Napoca (Romania, n = 150), Ragama (Sri Lanka, n = 152), Worcester (South Africa, n = 150) and Hue (Vietnam, n = 150). Inclusion criteria were as follows: (i) third trimester of pregnancy (i.e. weeks 29–40), (ii) aged over 18 and (iii) living primarily within the study’s defined geographical area. The average recruitment rate across sites was 82%. Table 1 presents sample characteristics by site for the 1181 women expecting singleton pregnancies in the current study (excluding 27 multiple pregnancies). On average, mothers were 28.27 years old, SD = 5.81 years, range: 18–48 years (note expectant mothers in Jamaica, Pakistan and South Africa were significantly younger than mothers in Romania, Ghana, Sri Lanka and Vietnam). For 359 /1181 (30%), this was their first pregnancy (note half of the Romanian mothers were experiencing their first pregnancy whilst Pakistan had the smallest proportion of women experiencing their first pregnancy across sites). The sample was diverse in terms of level of education: 4% none, 11% primary, 48% secondary, 16% vocational and 21% university (lowest to highest level of maternal education, respectively: Pakistan, Ghana, Jamaica, South Africa, Vietnam, Sri Lanka, Philippines and Romania).
Procedure
Information sheets, consent forms and questionnaires were translated (using guidelines from the World Health Organization; http://www.who.int/substance_abuse/research_tools/transla- tion/en/) into the most frequently spoken languages by the participants, who provided either written or audio-recorded informed consent. Expectant mothers in their third trimester of pregnancy (M = 33.23 weeks gestation, SD = 3.36) completed the PAI and reported on demographic factors/reproductive history as part of a structured interview. The Ethics Boards of each university approved the EBLS-FR protocol (Valdebenito et al. 2020).
Measures
Maternal-fetal attachment
Expectant mothers completed the 18-item PAI (Muller 1993). Participants rated how often they engaged in specific thoughts or behaviours towards the fetus (e.g., ‘I feel love for the baby’ or ‘I stroke the baby through my tummy’) on a 4-point scale: 1 = almost never, 2 = sometimes, 3 = often, 4 = almost always. A review of MFA questionnaires concluded that the PAI is psychometrically sound (e.g., Cronbach’s alpha ranges between .81 and .93) and, unlike other measures, includes behaviours and thoughts and feelings towards the fetus (van den Bergh and Simons 2009).
Background measures
Expectant mothers also reported on their age, socioeconomic status, education and previous pregnancies/ births.
Data analysis
We analysed the data using a latent variable framework in Mplus (Version 8.4; Muthén and Muthén 2018) and used Confirmatory Factor Analysis (CFA) to test measurement models and compare mean levels of MFA. Data screening indicated that there was no variability in responses to item 3 ‘I enjoy feeling the baby move’ in the Philippines and so it was removed from further analyses. Furthermore, the limited spread in the 4 response options across sites for the remaining the items indicated scores should be collapsed into dichotomous indicators (i.e., disagree/agree). This is in line with Rutkowski et al.’ (2019) recommended approach for dealing with floor/ceiling effects in response categories. Analyses applied the weighted least squares mean and variance adjusted (WLSMV) estimator. Following Muller’ (1993) original contention that MFA is unidimensional, we tested a 1-factor model alongside a 3-factor solution reflecting the dimensions of anticipation, differentiation and interaction suggested by some previous studies (e.g., Pallant et al. 2014). We evaluated model fit using three primary criteria: Comparative Fit Index (CFI) > 0.90, Tucker Lewis Index (CFI) > 0.90, Root Mean Square Error of Approximation (RMSEA) < 0.08 (Brown 2015). To test measurement invariance across site and parity, we used multigroup CFA, which involves systematically adding equality constraints to the model and testing the change in model fit of these nested models (Byrne 2012). Nested model comparisons were judged to be invariant if the CFI decreased by ≤0.020 and RMSEA increased by ≤ .003 (Svetina et al. 2020). First, we used a configural model to test for equivalence in the pattern of item loadings across site and then parity groups (i.e., the organisation of the construct is similar). If this model showed acceptable fit, we then proceeded to test metric (weak factorial) invariance, specifying that factor loadings were equal across sites (i.e., each item contributes in a similar way to the construct). If metric invariance was not achieved, we sought to improve model fit by inspecting modification indices to evaluate whether releasing item constraints would yield a partially invariant model. Next, for items that showed metric invariance, we tested for scalar (strong factorial) invariance, which involves equivalence of item thresholds (i.e., the cut-off underling the distribution of scores is consistent). Finally, if we established scalar invariance, we proceeded to test the mean differences in MFA by constraining the mean of the reference group to zero and freely estimating the other group means (Byrne 2012).
Results
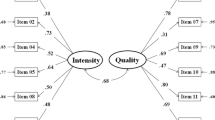
MFA factor structure
Both the 1-factor and 3-factor solution showed an acceptable fit to the data for all sites (Table 2). However, given the high overlap between the 3 factors (r = > .8) we proceeded to test the across-site equivalence of the 1-factor solution.
Tests of measurement invariance across site
The configural model showed poor model fit, CFI = 0.627, TLI = 0.633, RMSEA = 0.11, SRMR = 0.061. Inspection of the modification indices suggested the removal of Pakistan would improve the model fit. Indeed, the configural model for the 7 remaining sites showed good model fit, CFI = 0.925, TLI = 0.912, RMSEA = 0.05, SRMR = 0.061. Adding metric constraints did not significantly reduce model fit: CFI = 0.921, TLI = 0.914, RMSEA = 0.05, SRMR = 0.075, but imposing constraints to examine scalar invariance did reduce model fit. Inspection of modification indices led to releasing equality constraints of factor intercepts for 15 items (items 10 ‘I know when the baby is asleep’, 12 ‘I feel love for the baby’ and 16 ‘I stroke the baby through my tummy’ were invariant). Thus, a partially scalar invariant model was considered to have an acceptable model fit, CFI = 0.901, TLI = 0.897, RMSEA = 0.060.
Cross-cultural differences in prenatal attachment
Using the partial scalar-invariant model, we tested for mean differences in the latent factor across sites. We adopted a Bonferroni correction and adjusted the alpha level (i.e., p < .007) to account for multiple comparisons. With Ghana as the reference site, we found mean between-site differences in MFA, with lower levels in Vietnam, b = −.50, z = −3.78, p < .001, and higher levels in Sri Lanka, b = .73, z = 3.00, p < .001, however no significant contrasts with expectant mothers in Jamaica, Romania, Philippines and South Africa.
Parity and prenatal attachment
The model testing the equivalence of the configural model across parity showed acceptable fit, CFI = 0.911, TLI = 0.894, RMSEA = 0.053, SRMR = 0.052. Adding metric constraints led to a slight improvement in model fit, CFI = 0.912, TLI = 0.902, RMSEA = 0.051, SRMR = 0.06 and imposing constraints to examine scalar invariance did not significantly reduce model fit, CFI = 0.903, TLI = 0.902, RMSEA = 0.052, SRMR = 0.066. We subsequently compared the mean of the MFA latent factor across primiparous and multiparous women, which demonstrated higher MFA in first-time mothers: b = −.21, z = −2.19, p = .029.
Discussion
Evidence for links between MFA and clinically relevant pre- and post-natal behaviours (Rollè et al. 2020; Tichelman 2019) has relied heavily on studies from a few HICs. Addressing this gap, 1181 expectant mothers completed the PAI to examine the conceptual equivalence of MFA across eight LMICs: Ghana, Jamaica, Pakistan, Philippines, Romania, South Africa, Sri Lanka and Vietnam. The PAI showed conceptual and measurement equivalence for pregnant women in seven of the eight sites, with mean levels of MFA being lowest amongst expectant mothers in Vietnam and highest amongst expectant mothers in Sri Lanka. Whilst conceptually similar across levels of parity, MFA was greater in first-time mothers.
A Modified Measure of MFA shows Cross-Cultural Equivalence
Consistent with findings from studies that have adapted the PAI for use in non-English speaking HICs (e.g., Pavše et al. 2019), our analyses support a one-factor MFA model. Similar to previous research with the PAI in India (Lamba et al. 2018), the items contributing to MFA were dichotomised into agree/disagree options. The MFA latent factor exhibited partial measurement invariance across seven out of the eight sites—with some of item thresholds freely estimated at the scalar level of invariance. Taken together, this suggests that a simplified two-option (agree/disagree) PAI is appropriate for use across culturally diverse groups, which should increase confidence in the validity of cross-cultural comparisons, as well as in the use of the PAI in efforts to improve the health and wellbeing of women across the world (UN General Assembly 2015).
That said, the PAI did not pass the first level of equivalence testing in Pakistan. Closer inspection of item responses in Pakistan revealed a near-floor effect for seven items. For example, few expectant Pakistani mothers endorsed items such as: I stroke the baby through my tummy or I imagine calling the baby by name. This may reflect other contrasts between Pakistan and the other sites, including elevated rates of infant mortality (i.e., < 5 years of age = 74 per 1000 live births), poverty (i.e., GDP pc = $1550) and education (as highlighted in Table 1: expectant mothers in Pakistan received significantly lower levels of education than all sites aside from Ghana). The lack of item endorsement may reflect a coping strategy for the mothers. For example, in seminal ethnographic research in the Alto do Cruzeiro, a shantytown in northeast Brazil, Sheper-Hughes (1992) described how, in the context of high infant mortality, impoverished mothers inhibited attachment towards their infant after birth (e.g., not attributing human qualities towards their infants). Alternatively, prevailing belief systems may render specific items or explicit endorsement of items inappropriate. Ethnographic studies have emphasised expectant mothers in Pakistan are very discreet about their pregnancies, with open conversations both within and outside of the family seen as immodest (i.e., inferring disclosure of sexual activity) and inviting nazar (the evil eye of jealousy), which may harm the unborn infant (Qureshi and Pacquiao 2013; Qamar 2016). Thus, women may internalise rather than externalise their developing bond. Highlighting the importance of cultural appropriateness, Arafah et al. (2020) included four new items in the PAI to capture the MFA amongst Arabic-speaking women in Qatar (e.g., ‘I am careful with my activities so nothing will hurt my baby’). Future qualitative research might therefore help highlight relevant questions for pregnant women in Pakistan or whether the MFA construct lacks validity in this context.
Site-specific differences in MFA
Whilst we often lack good cross-cultural research, establishing the conceptual and measurement equivalence of measures across different cultures is a key pre-requisite for drawing valid group comparisons (Boer et al. 2018). Having established that the PAI shows measurement invariance across seven sites, we found lower levels of MFA in Vietnam and higher levels in Sri Lanka, than in the other five countries. One factor that might contribute to these site contrasts is variation in antenatal care. For example, in Sri Lanka, the overwhelming majority of expectant mothers use the free, comprehensive maternal healthcare package, which includes antenatal classes that encourage expectant mothers to promote specific behaviours, to seek partner support and to think about their developing infants as individuals (Hemachandra 2011). Future research is needed to unpack the, potentially diverse, origins of differences in MFA, for example cultural norms, sampling and economic factors. Our study reinforces the importance of testing the equivalence of measures in multi-site studies in order to make meaningful comparisons.
First-time pregnancy: a time to reflect?
First-time mothers reported higher MFA than mothers in later pregnancies. Whilst similar results studies have been reported in high- (e.g., Tichleman et al. 2019) and upper-middle-income countries (e.g. Turkey; Özcan et al. 2018), the measurement invariance tests employed in the current study increase the confidence that there is a true and meaningful effect of parity. One simple explanation is that first-time mothers have greater psychological space for thinking about their new infant than mothers who are already taking care of younger infants. Our results suggest this parity effect is culturally universal—indeed, the magnitude of this effect appears stronger in this study than in previous meta-analyses (Yarcheski et al. 2009; Tichelman et al. 2019).
Strengths and limitations
The inclusion of data from eight LMICs is a key strength of the study. Notably, similar studies of measurement equivalence have excluded data from LMICs due to a low response rate (e.g., Zhang 2020). That said, our samples were recruited using a non-probabilistic sampling strategy, which potentially limits the generalisability of our results to the wider population. Furthermore, although the average rate of recruitment was high (82%), there was between-site variability (i.e., ranging from 50% in Sri Lanka to 98% in Pakistan) which suggests further research is required to rule out the possibility that elevated rates of MFA reported by expectant mothers in Sri Lanka are not the result of selection bias. In addition, sample characteristics differed across sites, for example in terms of education (see Table 1). However, having established the measurement properties of the PAI as an index of MFA, future research can examine the cultural universality/specificity of these associations as well explore the use of the PAI as a screener for maternal behaviours that may place children at risk.
Conclusions
By adapting the PAI to yield a simple but valid tool that shows cross-cultural equivalence in seven LMICs and across birth order, we hope to stimulate further work examining prenatal psychological processes underpinning maternal and infant adjustment across the first 1000 days.
Change history
15 April 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00737-021-01122-7
References
Arafah D, Thomas B, Fenton TR, Sabr Y, Metcalfe A (2020) Validity and reliability of the Arabic version of Muller’s prenatal attachment inventory. J Psychosom Obstet Gynecol 1–9. https://doi.org/10.1080/0167482X.2020.1713083
Boer D, Hanke K, He J (2018) On detecting systematic measurement error in cross-cultural research: a review and critical reflection on equivalence and invariance tests. J Cross-Cult Psychol 49:713–734. https://doi.org/10.1177/0022022117749042
Brandon AR, Pitts S, Denton WH, Stringer CA, Evans HM (2009) A history of the theory of prenatal attachment. J Prenat Perinat Psychol Health 23(4):201–222
Brown T (2015) Confirmatory factor analysis for applied research, 2nd edn. Guilford Press, London
Buffa G, Dahan S, Sinclair I, St-Pierre M, Roofigari N, Mutran D, Rondeau J-J, Dancause KN (2018) Prenatal stress and child development: a scoping review of research in low- and middle-income countries. PLoS One 13:e0207235. https://doi.org/10.1371/journal.pone.0207235
Byrne B (2012) Structural equation modeling with Mplus: basic concepts, applications, and programming (multivariate applications series). Routledge, New York
Cinar N, Caka SY, Topal S, Yuvaci HU, Erkorkmaz U (2017) The relation of health-related practices of pregnant women, fatigue and prenatal attachment. J Coll Physicians Surg Pak 27:693–698
Commission on Health Research for Development (1990) Health research: essential link to equity in development. Oxford University Press, New York
Cranley M (1981) Development of a tool for the measurement of maternal attachment during pregnancy. MS Nurs Res 30:281–284. https://doi.org/10.1097/00006199-198109000-00008
Edhborg M, Nasreen H-E, Kabir ZN (2011) Impact of postpartum depressive and anxiety symptoms on mothers’ emotional tie to their infants 2–3 months postpartum: a population-based study from rural Bangladesh. Arch Womens Ment Health 14:307–316. https://doi.org/10.1007/s00737-011-0221-7
Field T (2010) Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev 33:1–6. https://doi.org/10.1016/j.infbeh.2009.10.005
Fisher J, Mello MCD, Patel V, Rahman A, Tran T, Holton S, Holmes W (2012) Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: a systematic review. Bull World Health Organ 90:139–149. https://doi.org/10.2471/BLT.11.091850
Foley S, Hughes C (2018) Great expectations? Do mothers’ and fathers’ prenatal thoughts and feelings about the infant predict parent-infant interaction quality? A meta-analytic review. Dev Rev 48:40–54. https://doi.org/10.1016/j.dr.2018.03.007
Hemachandra N (2011) Maternal care package: a guide to field healthcare workers. Family Health Bureau, Ministry of Health. Sri Lanka
Henrich J, Heine SJ, Norenzayen A (2010) The weirdest people in the world? Behav Brain Sci 33:1–75. https://doi.org/10.1017/S0140525X0999152X
Lamba N, Jadva V, Kadam K, Golombok S (2018) The psychological well-being and prenatal bonding of gestational surrogates. Hum Reprod 33:646–653. https://doi.org/10.1093/humrep/dey048
Laxton-Kane M, Slade P (2002) The role of maternal prenatal attachment in a woman’s experience of pregnancy and implications for the process of care. J Reprod Infant Psychol 20:253–266. https://doi.org/10.1080/0264683021000033174
Lindgren K (2001) Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Res Nurs Health 24:203–217. https://doi.org/10.1002/nur.1023
Lingeswaran A, Bindu H (2012) Validation of Tamil version of Cranley’s 24-item maternal–fetal attachment scale in Indian pregnant women. J Obstet Gynaecol India 62:630–634. https://doi.org/10.1007/s13224-012-0175-3
Mills-Koonce W, Willoughby M, Zvara B, Barnett M, Gustafsson H, Cox MJ (2015) Mothers’ and fathers’ sensitivity and children’s cognitive development in low- income, rural families. J Appl Dev Psychol 38:1–10. https://doi.org/10.1016/j.appdev.2015.01.001
Muller ME (1993) Development of the prenatal attachment inventory. West J Nurs Res 15:199–215. https://doi.org/10.1177/019394599301500205
Muthén LK, Muthén B (2018) Mplus. The comprehensive modelling program for applied researchers: user’s guide 5. Muthén, B & Muthén, LK, Los Angeles
Özcan NK, Boyacıoğlu NE, Dikeç G, Dinç H, Enginkaya S, Tomruk N (2018) Prenatal and postnatal attachment among Turkish mothers diagnosed with a mental health disorder. Issues Ment Health Nurs 39:795–801. https://doi.org/10.1080/01612840.2018.1455773
Pallant JF, Haines HM, Hildingsson I, Cross M, Rubertsson C (2014) Psychometric evaluation and refinement of the Prenatal Attachment Inventory. J Reprod Infant Psychol 32:112–125. https://doi.org/10.1080/02646838.2013.871627
Parsons CE, Young KS, Rochat TJ, Kringelbach ML, Stein A (2012) Postnatal depression and its effects on child development: a review of evidence from low- and middle-income countries. Br Med Bull 101:57–79. https://doi.org/10.1093/bmb/ldr047
Pavše L, Tul N, Velikonja V (2019) Analysis of the internal structure of the Slovenian version of the Prenatal Attachment Inventory (PAI) [Analiza notranje strukture slovenskega prevoda Lestvice vezi med nosečnico in plodom (PAI). Psiholoska Obzorja 28:11–18. https://doi.org/10.20419/2019.28.496
Punamäki RL, Isosävi S, Qouta SR, Kuittinen S, Diab SY (2017) War trauma and maternal–fetal attachment predicting maternal mental health, infant development, and dyadic interaction in Palestinian families. Attach Hum Dev 19:463–486. https://doi.org/10.1080/14616734.2017.1330833
Qamar AH (2016) Belief in the evil eye and early childcare in rural Punjab, Pakistan. Asian Ethnology 75:397–418. https://doi.org/10.2307/asianeth.75.2.397
Qureshi R, Pacquiao D (2013) Ethnographic study of experiences of Pakistani women immigrants with pregnancy, birthing, and postpartum care in the United States and Pakistan. J Transcult Nurs 24:355–362. https://doi.org/10.1177/1043659613493438
Rollè L, Giordano M, Santoniccolo F, Trombetta T (2020) Prenatal attachment and perinatal depression: a systematic review. Int J Environ Res Public Health 17:2644. https://doi.org/10.3390/ijerph17082644
Rutkowski L, Svetina D, Liaw Y-L (2019) Collapsing categorical variables and measurement invariance. Struct Equ Model Multidiscip J 0:1–13. https://doi.org/10.1080/10705511.2018.1547640
Sheper-Hughes N (1992) Death without weeping: the violence of everyday life in Brazil. University of California Press, Berkeley, Los Angeles, Oxford
Svetina D, Rutkowski L, Rutkowski D (2020) Multiple-group invariance with categorical outcomes using updated guidelines: an illustration using Mplus and the lavaan/semTools packages. Struct Equ Model Multidiscip J 27:111–130. https://doi.org/10.1080/10705511.2019.1602776
Tichelman E, Westerneng M, Witteveen AB, Van Baar AL, Van Der Horst HE, De Jonge A, Berger MY, Schellevis FG, Burger H, Peters LL (2019) Correlates of prenatal and postnatal mother to-infant bonding quality: a systematic review. PLoS One 14:e0222998. https://doi.org/10.1371/journal.pone.0222998
UN General Assembly, Transforming our world : the 2030 agenda for sustainable development, 21 October 2015, A/RES/70/1, available at: https://www.refworld.org/docid/57b6e3e44.html. Accessed 24 Sept 2020
Valdebenito S, Murray AL, Hughes C, Baban A, Asvini D et al (2020) Evidence for Better Lives Study: A comparative birth-cohort study on child exposure to violence and other adversities in eight low- and middle-income countries – Foundational Research. BMJ Open 10:e034986.
van den Bergh B, Simons A (2009) A review of scales to measure the mother-foetus relationship. J Reprod Infant Psychol 27:114–126. https://doi.org/10.1080/02646830802007480
Vidyasagar D (2006) Global notes: the 10/90 gap disparities in global health research. J Perinatol 26:55–56. https://doi.org/10.1038/sj.jp.7211402
Walsh J (2010) Definitions matter: if maternal-fetal relationships are not attachment, what are they? Arch Womens Ment Health 13:449–451. https://doi.org/10.1007/s00737-010-0152-8
Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG (2017) A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord 219:86–92. https://doi.org/10.1016/j.jad.2017.05.003
Yarcheski A, Mahon N, Yarcheski T, Hanks M, Cannella B (2009) A meta-analytic study of predictors of maternal-fetal attachment. Int J Nurs Stud 46:708–715. https://doi.org/10.1016/j.ijnurstu.2008.10.013
Zhang RJ (2020) Social trust and satisfaction with life: a cross-lagged panel analysis based on representative samples from 18 societies. Soc Sci Med 251:112901. https://doi.org/10.1016/j.socscimed.2020.112901
Funding
The work of the Evidence for Better Lives Study was supported by the Jacobs Foundation, UBS Optimus Foundation, Fondation Botnar, the Consuelo Zobel Alger Foundation, the British Academy, the Cambridge Humanities Research Grants Scheme, the ESRC Impact Acceleration Account Programme, a Queensland University of Technology Postgraduate Research Award, Higher Degree Research Student Supplementary Research Funding from Queensland University of Technology, the University of Edinburgh College Office for the College of Arts, the Humanities and Social Sciences SFC ODA Global Challenges Internal Fund, the University of Cambridge GCRF Quality Research Fund and the Wolfson Professor of Criminology Discretionary Fund. The first author was funded by an Economic and Social Research Council Post-Doctoral Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Disclaimer
The content of this paper is the responsibility of the authors and does not reflect official views of these funding bodies.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The names of the authors were incorrect.
1. Bao-Yen Luong-Thanh appears twice – please remove Yen Lương Thanh Bảo
2. Replace Yen Lương Thanh Bảo with Thang Van Vo
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Foley, S., Hughes, C., Murray, A.L. et al. Prenatal attachment: using measurement invariance to test the validity of comparisons across eight culturally diverse countries. Arch Womens Ment Health 24, 619–625 (2021). https://doi.org/10.1007/s00737-021-01105-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-021-01105-8