Abstract
To prevent the progression of type 2 diabetes mellitus (T2DM), early detection and intervention are important. Several studies have already shown that the serum adiponectin level could be useful for evaluating the future risk of T2DM. Recently, plasma free amino acid (PFAA) concentrations have also emerged as potential biomarkers that predict the future onset of T2DM. In this study, we aimed to further characterise PFAA profiles by elucidating the association with the serum high molecular weight (HMW) adiponectin level in this cross-sectional study. A total of 1000 Japanese subjects who underwent medical check-ups were enrolled, and their plasma concentrations of 21 amino acids and clinical parameters were measured. The subjects without T2DM were divided into quartiles (Q1-4) by serum HMW adiponectin level, and the association with between PFAA concentrations was analysed. Concentrations of glutamate, alanine, proline, tyrosine, histidine, methionine, lysine, branched-chain amino acids (BCAAs) and tryptophan varied significantly according to the adiponectin quartile. Furthermore, serum adiponectin levels showed significant inverse correlations with these amino acids. The change in the PFAA profile in the group with the lowest adiponectin concentrations (Q1) was similar to that of T2DM patients. Although both adiponectin levels and PFAA concentrations are known to be altered by the accumulation of visceral fat and insulin resistance, the levels of glutamate, BCAA, lysine and tryptophan remain significantly associated with adiponectin level after adjustment for age, body mass index and homeostasis model assessment of insulin resistance, showing the direct association between PFAA concentrations and the serum HMW adiponectin level. Registration number: University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) UMIN000029920, registered on Nov 13th 2017 (prospectively registered).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metabolic syndrome, which is mainly caused by the accumulation of visceral fat, is a pathophysiological state that causes type 2 diabetes mellitus (T2DM). T2DM has become a major health issue worldwide, including in Asian regions, since constant high blood glucose levels can damage both the large and small blood vessels of various organs, which leads to macrovascular/microvascular complications, including cardiovascular disease, ischaemic heart disease and dysfunction in the eyes, kidneys, feet and nerves (Orasanu and Plutzky 2009). These health problems have a negative impact on not only patients’ quality of life but also medical costs; they require continuous clinical care and management that consume significant health-care resources. To prevent T2DM and the progression of these complications, it is critically important to detect the risk in the early phase of metabolic syndrome and for patients to change their lifestyles.
Previous studies have found that adipose tissue is an endocrine organ that produces and secretes various bioactive substances, referred to as adipocytokines (Scherer et al. 1995; Maeda et al. 1996). Adiponectin, an adipocytokine, is known to work as an insulin sensitiser and modify glucose homeostasis (Kadowaki et al. 2006). The concentration of adiponectin in blood shows a strong inverse association with the progression of insulin resistance and T2DM (Ziemke and Mantzoros 2010; Li et al. 2009). Furthermore, some previous longitudinal studies have shown that the circulating adiponectin level predicts subsequent changes in insulin resistance and the incidence of T2DM within several years (Choi et al. 2004; Yamamoto et al. 2004), suggesting that the adiponectin level could be useful as a biomarker that reflects the future risk of T2DM onset.
Several recent studies have shown that plasma free amino acid (PFAA) profiles are altered prior to the development of T2DM or cardiovascular events. In prospective cohort studies such as the Framingham Offspring Study, PFAA levels, particularly the levels of branched-chain amino acids (BCAAs) and aromatic amino acids, were significantly associated with a future diagnosis of T2DM (Wang et al. 2011) and cardiovascular diseases (Magnusson et al. 2013). Other studies also revealed that several amino acids were significantly altered in Japanese people with high visceral obesity independent of their body mass index (BMI) and that a specific formula incorporating some PFAA concentrations correlated with visceral fat area was able to predict the four-year risk of developing new-onset lifestyle-related diseases, including T2DM, metabolic syndrome and dyslipidaemia (Yamakado et al. 2015). All these data suggest that PFAAs could be another novel potential biomarker for predicting the future risk of T2DM and other lifestyle-related diseases.
Although these previous reports suggest that both adiponectin and PFAAs could be useful for the early detection of future T2DM risk, the potential of PFAAs as biomarkers has not been fully elucidated compared with that of the serum adiponectin level, which has been widely regarded as a surrogate marker for metabolic status in the body. To the best of our knowledge, few studies have investigated the relationship between adiponectin and PFAAs. A previous study showed that the levels of several amino acids were highly correlated with adiponectin and insulin-related markers in T2DM patients (Nakamura et al. 2014). Another study reported a significant correlation of the high molecular weight (HMW) adiponectin level with amino acid levels, but this observation is limited for BCAAs (Katagiri et al. 2018). In this cross-sectional study, we investigated the alteration of PFAA profiles, i.e., 21 amino acids, according to circulating HMW adiponectin levels and clarified their association in a large healthy Japanese population undergoing health check-ups at our hospital. Through this analysis, we attempted to characterise PFAA profiles as potential biomarkers.
Materials and methods
Ethics statement
This study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Faculty of Medicine Research Ethics Committee at Kyorin University and the ethics committees of Ajinomoto Co., Inc. All the subjects gave their written informed consent for inclusion before they participated in the study. All the data were analysed anonymously throughout the study. The study was registered in the University Hospital Medical Information Network Clinical Trials Registry (UMIN-CTR) UMIN000029920.
Subjects
This study was a cross-sectional evaluation of the relationship between the adiponectin level and levels of glucose-, insulin- and lipid-related variables obtained with clinical laboratory tests. From December 2017 to March 2019, a total of 1000 individuals utilised the Ningen Dock comprehensive medical check-up system at Kyorin University Hospital and gave their informed consent for participation in this study.
Measurement of metabolic variables and quantification of PFAAs
Blood samples were taken from the subjects after overnight (> 8 h) fasting. Fasting plasma glucose (FPG) was measured with the hexokinase method, and haemoglobin A1c (HbA1c) and serum HMW adiponectin were quantified using the latex agglutination immunoassay. Serum insulin levels were measured immunologically. Serum concentrations of triglycerides were measured using an enzymatic colorimetric assay (Sekisui Medical, Tokyo, Japan), and low-density lipoprotein (LDL) cholesterol and high-density lipoprotein (HDL) cholesterol were measured using direct methods (Sekisui Medical). All clinical laboratory tests were performed by SRL (Tokyo, Japan). The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated using the following equation: HOMA-IR = Fasting insulin level (μU ml−1) × Fasting plasma glucose level (mg dl−1)/405.
For the amino acid analyses, blood samples (5 ml) were collected from a forearm vein into tubes containing disodium ethylenediaminetetraacetate after overnight fasting and were immediately placed on ice. The plasma was isolated by centrifugation and then stored at − 80 °C until analysis. The plasma samples were deproteinised with acetonitrile at a final concentration of 80% before measurement. The plasma amino acid concentrations were measured by high-performance liquid chromatography–electrospray ionization mass spectrometry followed by precolumn derivatization as previously described (Shimbo et al. 2009a, 2009b). The following 21 amino acids were measured: alpha aminobutyric acid (aABA), alanine (Ala), arginine (Arg), asparagine (Asn), citrulline (Cit), glutamine (Gln), glutamate (Glu), glycine (Gly), histidine (His), isoleucine (Ile), leucine (Leu), lysine (Lys), methionine (Met), ornithine (Orn), phenylalanine (Phe), proline (Pro), serine (Ser), threonine (Thr), tryptophan (Trp), tyrosine (Tyr), and valine (Val).
Statistical analysis
Among the 1000 participants, those who had missing data (n = 2) and/or had been diagnosed with type 2 diabetes (medical history and/or FPG ≥ 126 mg/dL, HbA1c ≥ 6.5%) (n = 96) were excluded. Participants were divided into quartiles according to HMW adiponectin levels (Q1-4). Differences in participant characteristics among the quartiles were tested using analysis of variance for continuous variables. For multivariate analysis, the adiponectin level and HOMA-IR were log-transformed. Statistical and multivariate analyses were performed with the JMP 12.2.0 program (SAS Institute Inc., Cary, NC, USA). The data in the tables are expressed as the mean ± SD. The datasets generated during and/or analysed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author on reasonable request.
Result
The subjects without T2DM were classified according to their serum HMW adiponectin quartiles. Since sex is also known to be a strong factor that influences both plasma amino acid concentrations and serum adiponectin levels, we also stratified them by sex. Table 1 shows the subject’s basic characteristics, including diabetes-related markers. As previous studies have indicated (Katagiri et al. 2018), subjects in the lowest HMW adiponectin quartile (Q1) showed higher BMI, HOMA-IR, and triglyceride values and lower HDL cholesterol values for both men and women. On the other hand, there were no associations between the adiponectin quartiles and blood glucose-related parameters such as FPG and HbA1c. Subjects with T2DM showed remarkably higher HOMA-IR, FPG and HbA1c values for both sexes.
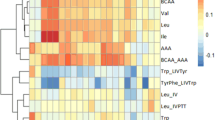
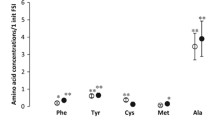
Table 2 shows PFAA profiles according to HMW adiponectin quartiles. Concentrations of Glu, Ala, Pro, Tyr, His, Met, Lys, Val, Leu, Ile and Trp varied significantly according to the adiponectin quartiles in both men and women. Concentrations of all these amino acids in the lowest adiponectin quartile (Q1) were the highest in the all quartiles, although women in the Q2 group showed the highest values of Ala, Pro, His and Lys. Among men, Gly and Cit values were the lowest in the Q1 group.
The radar charts in Fig. 1 show the relative value of each PFAA among subjects in the lowest adiponectin quartile (Q1) and in T2DM subjects compared with those in the highest adiponectin quartile (Q4). Concentrations of Glu, Ala, Pro, Tyr, Val, Met, Lys Ile, Leu and Trp in Q1 were significantly higher than those in Q4; in particular, Glu, Pro and BCAA levels were increased by 20–60% and 10–40% in men and women, respectively. The PFAA alterations in the Q1 quartile showed a similar pattern to those in T2DM for both men and women, although aABA and Orn levels were significantly increased only in T2DM patients.
Alterations in PFAA concentrations in the lowest HMW adiponectin quartile and T2DM patients. Radar charts show relative values of 21 plasma amino acid concentrations in the lowest HMW adiponectin quartile (Q1) (red line) and T2DM patients (blue line) compared with those in the highest HMW adiponectin quartile (Q4) for men (A) and women (B). Statistical differences were evaluated by ANOVA followed by Dunnett’s test. *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001 between Q1 and Q4. †P < 0.05, ††P < 0.01, †††P < 0.001 and ††††P < 0.0001 between T2DM and Q4
Pearson’s correlation coefficients between PFAA levels and clinical variables for non-T2DM subjects are shown in Table 3. Consistent with the results of Table 2, the HMW adiponectin level showed significant negative correlations with BMI, HOMA-IR and various PFAAs. Among the PFAAs, the adiponectin level was significantly correlated with Glu (r = − 0.4126 and − 0.3268 for men and women, respectively), Val (r = − 0.4035 and − 0.3318), Ile (r = − 0.3899 and − 0.3614) and Leu (r = − 0.4259 and − 0.3674). Although these amino acids were also significantly associated with HOMA-IR, there were no or weak correlations with FPG and HbA1c. Similar relationships were also observed for men with T2DM; Glu and BCAA levels were significantly and inversely associated with adiponectin (supplementary table 1).
Since significant correlations between PFAA concentrations and BMI or HOMA-IR were observed, PFAA concentrations were adjusted for age, BMI and HOMA-IR by multivariate analysis to remove their confounding effect on the relationship between the levels of adiponectin and PFAAs (Table 4). The results showed that significant associations between the adiponectin level and Glu, BCAA, Lys or Trp concentrations were still observed after adjustment for age, BMI and HOMA-IR for both men and women.
Discussion
In the current cross-sectional study, we investigated the association between serum HMW adiponectin levels and PFAA concentrations in a large number of Japanese people who underwent medical check-ups. The results showed that the HMW adiponectin level in nondiabetic subjects was significantly and inversely correlated with BCAA, Glu, Lys and Trp concentrations, and this association remained even after adjustment for age, BMI and HOMA-IR, suggesting that their relationship could be independent of fat mass or insulin resistance.
Although a previous study has already shown that plasma BCAA concentrations are significantly associated with adipokine levels, including both total and HMW adiponectin and leptin, in a Japanese population without diabetes (Maeda et al. 1996), to our knowledge, this is the first study to investigate their association with levels of 21 amino acids. Consistent with a previous report, our study also showed the strongest correlation among the level of each BCAA, HMW adiponectin levels and HOMA-IR, which is generally recognised as a marker of insulin resistance. To date, many studies have shown that plasma BCAA levels correlate with insulin resistance (White and Newgard 2019). One of the mechanisms for the elevation of plasma BCAA levels associated with insulin resistance was thought to be a decrease in BCAA catabolism. A decrease in both insulin action and utilization of amino acids in muscle causes a lower uptake of BCAAs into muscle (Pozefsky et al. 1969). In addition, subjects with insulin resistance showed decreased concentrations of branched-chain keto acids and α-ketoglutarate and increased acylcarnitine concentrations in muscle (Lerin et al. 2016), which suggests low activity of BCAA aminotransferase, the first enzyme to catalyse reversible transamination of all BCAAs to branched-chain keto acids. Other studies revealed that BCAAs are also metabolised in visceral adipose tissues, and insulin resistance causes a decrease in the expression levels of adipose tissue BCAA-catabolizing enzymes (Herman et al. 2010; Lackey et al. 2013). In our study, however, the association between the adiponectin level and BCAA concentrations was significant even after adjustment for BMI and HOMA-IR, suggesting a direct connection between them. Another study using mice showed that adiponectin rectifies elevated BCAA levels in blood induced by a high-fat diet (Liu et al. 2013; Lian et al. 2015), which suggests that alteration of BCAA concentrations might be directly reflected by a change in adiponectin level. Further investigation is needed to more precisely clarify the mechanism for the relationship among adiponectin, BCAAs and insulin resistance.
The plasma Glu concentration was also highly and negatively correlated with adiponectin levels. The Glu concentration in plasma is known to change drastically depending on the handling of blood samples. For instance, its concentration in whole blood left at room temperature for only 10 min is increased by more than 20% due to the action of glutaminase, which converts Gln into Glu (Takehana et al. 2016), meaning that strict sample management is required for the accurate quantification of Glu. In this study, we cooled whole blood samples immediately (i.e., less than 1 min) after blood collection, and this procedure enabled us to reveal the precise associations between the plasma Glu level and other variables. It has been reported that the Glu level in plasma is correlated more highly with visceral fat area than with subcutaneous fat area (Yamakado et al. 2012). Since the visceral fat area has been thought to be related to insulin resistance or decreased levels of adiponectin, our results are consistent with the report. A recent study has shown that the abundance of Bacteroides thetaiotaomicron in stool samples, a glutamate-fermenting commensal, is markedly decreased in obese individuals and is inversely correlated with the Glu concentration in serum. Furthermore, gavage with B. thetaiotaomicron reduced the plasma glutamate concentration and alleviated diet-induced body weight gain and adiposity in mice (Liu et al. 2017). The authors also reported that the relative abundance of B. thetaiotaomicron was positively correlated with circulating adiponectin levels and negatively correlated with circulating leptin levels. All these results suggest that the gut microbiome might play a central role in the mechanism underlying the strong relationship between Glu and adiponectin levels.
A significant change in Trp levels according to serum adiponectin quartiles was also observed. The Trp concentration in plasma has been known to be correlated with the status of protein nutrition, since Trp binds to albumin in blood. The current study also showed a significant correlation between Trp and albumin levels (data not shown). On the other hand, the albumin level was not changed among the adiponectin quartiles, suggesting that the relationship between Trp and adiponectin levels observed in the current study is not the result of a difference in protein nutrition. Although alteration of Trp levels caused by insulin resistance and T2DM is controversial (Oxenkrug 2015; Herrera et al. 2003; Chen et al. 2016), Trp metabolism is known to be highly associated with insulin resistance and T2DM (Le Floc’h et al. 2011; Oxenkrug 2013). The expression of indoleamine-2,3-dioxygenase (IDO), which is a rate-limiting enzyme of the Trp-kynurenine pathway, was enhanced, and metabolites in this pathway, such as kynurenine, were shown to be increased in obese people (Favennec et al. 2015). Since the kynurenine pathway and its metabolites are related to inflammation, further investigation will be needed to clarify the impact of inflammation associated with insulin resistance or adiponectin action on the plasma Trp level.
A previous study revealed a correlation between PFAA profiles (Glu, Ala, Trp and BCAAs) and adiponectin levels in T2DM patients (Nakamura et al. 2014). In the current study, we also obtained similar results: Glu and BCAA levels, which showed a significant correlation with the adiponectin level in non-T2DM subjects, were also negatively associated with adiponectin levels in T2DM men, although this result was not observed for T2DM women, probably due to the small number of subjects. This suggests that their correlation could be maintained independent of the onset of T2DM. Since T2DM patients might take antidiabetic drugs before the time of blood collection (the proportion is unclear in the present study), glucose-related parameters would not be suitable for monitoring the metabolic states in the body. PFAA concentrations and the adiponectin level could be potential indicators that cannot be estimated by circulating blood glucose levels independent of the onset of T2DM.
In the current study, subjects without T2DM in the lowest HMW adiponectin quartile (Q1) showed a similar change in the PFAA profile as that in T2DM subjects when compared with subjects in the Q4 quartile. Daimon et al. conducted 5-year follow-up examinations and showed that decreased serum adiponectin levels were an independent risk factor for the progression to T2DM in a Japanese population (Daimon et al. 2012), suggesting that subjects in Q1 were more likely to develop T2DM than those in Q4. Likewise, several studies have reported that changes in PFAA profiles occur before the onset of T2DM. The Framingham Offspring Study revealed that PFAA levels, particularly the levels of BCAAs and aromatic amino acids such as Phe and Tyr, were significantly associated with a future diagnosis of T2DM and cardiovascular diseases (Wang et al. 2011). In addition, a study that enrolled Japanese subjects showed that levels of several amino acids and a PFAA index (constructed to model the relationships between the PFAA profiles and the visceral fat area by multiple linear regression) showed good capabilities to predict future risk of developing new-onset lifestyle-related diseases. These results indicate that the PFAA profile and adiponectin level are potential biomarkers for predicting the future risk of T2DM. In fact, the technology has been applied to a risk screening test named “AminoIndexTM Life Style Risk Screening” in Japan, which predicts the risk of developing T2DM within 4 years based on PFAA profiles (Nagao and Kimura 2020). Furthermore, both markers are known to be normalised by various types of interventions. Reduction of ~ 10–20% body weight in obese subjects or a specific diet, such as a low-fat diet, daily supplementation with fish or omega 3 fatty acids, and fibre supplementation, significantly increased the concentration of adiponectin in serum (Salas-Salvadó et al. 2006; Kasim-Karakas et al. 2006; He et al. 2004; Nelson et al. 2007; Micallef and Garg 2009; Grunberger et al. 2007). Weight loss induced by the diet and exercise intervention normalised the circulating levels of PFAAs (Tochikubo et al. 2016). These results suggest that both markers could be useful for not only detecting the risks of developing lifestyle-related diseases in the future but also monitoring improvements in physiological conditions.
The current study has several limitations. First, this is a cross-sectional study, which makes it difficult for us to confirm the direct or causal relationship between plasma amino acid profiles and the serum HMW adiponectin level. Although we adjusted it with some potential confounding factors such as BMI and HOMA-IR, the possibility that other confounding factors might exist cannot be eliminated. In addition, the value of BMI cannot provide accurate data for visceral adiposity which is more closely linked to metabolic syndrome, since BMI itself cannot differentiate between lean mass and fat mass. More suitable parameters should be taken into account for further analysis. Second, we did not assess dietary habits among subjects in this study. Indispensable amino acids including BCAAs, Lys and Trp cannot be synthesized in the body and their homeostasis partially depends on the intake from diet, which suggests that the amount of dietary intake of these amino acids could be reflected on their plasma concentrations. A previous study has shown that the contribution of lifestyle factors including dietary BCAA intake to plasma BCAA concentrations is much less than that of BMI (Hamaya et al. 2022), suggesting that dietary patterns would have little impact on our results. However, subjects enrolled in the previous study showed much higher BMI than those in this study conduted in Japan, which could make the contribution of BMI relatively larger. Further investigations will be needed to clarify the precise association between plasma amino acid profiles and the metabolic state in the body.
In conclusion, this study clarified the significant association between PFAA concentrations and the serum HMW adiponectin level. In addition to the serum adiponectin level which has been widely recognised as a useful biomarker for the detection of T2DM risk, PFAA concentrations could be used as a potential biomarker. Further longitudinal studies are needed to confirm and compare their performance as an efficient biomarker of the future T2DM risk and identify the underlying mechanism of this association.
Data Availability
The datasets generated during and/or analysed during the current study are not publicly available due to ethical restrictions but are available from the corresponding author on reasonable request.
References
Chen T, Zheng X, Ma X, Bao Y, Ni Y, Hu C, Rajani C, Huang F, Zhao A, Jia W, Jia W (2016) Tryptophan predicts the risk for future type 2 diabetes. PLoS ONE 11(9):e0162192. https://doi.org/10.1371/journal.pone.0162192
Choi KM, Lee J, Lee KW, Seo JA, Oh JH, Kim SG, Kim NH, Choi DS, Baik SH (2004) Serum adiponectin concentrations predict the developments of type 2 diabetes and the metabolic syndrome in elderly Koreans. Clin Endocrinol 61(1):75–80. https://doi.org/10.1111/j.1365-2265.2004.02063.x
Daimon M, Oizumi T, Kato T (2012) Decreased serum levels of adiponectin as a risk for development of type 2 diabetes, and impaired glucose tolerance as a risk for stroke–the Funagata study. Nihon Rinsho Jpn J Clin Med 70(Suppl 3):256–259
Favennec M, Hennart B, Caiazzo R, Leloire A, Yengo L, Verbanck M, Arredouani A, Marre M, Pigeyre M, Bessede A, Guillemin GJ, Chinetti G, Staels B, Pattou F, Balkau B, Allorge D, Froguel P, Poulain-Godefroy O (2015) The kynurenine pathway is activated in human obesity and shifted toward kynurenine monooxygenase activation. Obesity (silver Spring, Md) 23(10):2066–2074. https://doi.org/10.1002/oby.21199
Grunberger G, Jen KL, Artiss JD (2007) The benefits of early intervention in obese diabetic patients with FBCx: a new dietary fibre. Diabetes Metab Res Rev 23(1):56–62. https://doi.org/10.1002/dmrr.687
Hamaya R, Mora S, Lawler PR, Cook NR, Buring JE, Lee IM, Manson JE, Tobias DK (2022) Association of Modifiable Lifestyle Factors with Plasma Branched-Chain Amino Acid Metabolites in Women. J Nutr 152(6) 1515-1524 https://doi.org/10.1093/jn/nxac056
He K, Hu FB, Colditz GA, Manson JE, Willett WC, Liu S (2004) Changes in intake of fruits and vegetables in relation to risk of obesity and weight gain among middle-aged women. Int J Obes Relat Metab Dis 28(12):1569–1574. https://doi.org/10.1038/sj.ijo.0802795
Herman MA, She P, Peroni OD, Lynch CJ, Kahn BB (2010) Adipose tissue branched chain amino acid (BCAA) metabolism modulates circulating BCAA levels. J Biol Chem 285(15):11348–11356. https://doi.org/10.1074/jbc.M109.075184
Herrera R, Manjarrez G, Nishimura E, Hernandez J (2003) Serotonin-related tryptophan in children with insulin-dependent diabetes. Pediatr Neurol 28(1):20–23. https://doi.org/10.1016/s0887-8994(02)00462-9
Kadowaki T, Yamauchi T, Kubota N, Hara K, Ueki K, Tobe K (2006) Adiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndrome. J Clin Investig 116(7):1784–1792. https://doi.org/10.1172/jci29126
Kasim-Karakas SE, Tsodikov A, Singh U, Jialal I (2006) Responses of inflammatory markers to a low-fat, high-carbohydrate diet: effects of energy intake. Am J Clin Nutr 83(4):774–779. https://doi.org/10.1093/ajcn/83.4.774
Katagiri R, Goto A, Budhathoki S, Yamaji T, Yamamoto H, Kato Y, Iwasaki M, Tsugane S (2018) Association between plasma concentrations of branched-chain amino acids and adipokines in Japanese adults without diabetes. Sci Rep 8(1):1043. https://doi.org/10.1038/s41598-018-19388-w
Lackey DE, Lynch CJ, Olson KC, Mostaedi R, Ali M, Smith WH, Karpe F, Humphreys S, Bedinger DH, Dunn TN, Thomas AP, Oort PJ, Kieffer DA, Amin R, Bettaieb A, Haj FG, Permana P, Anthony TG, Adams SH (2013) Regulation of adipose branched-chain amino acid catabolism enzyme expression and cross-adipose amino acid flux in human obesity. Am J Physiol Endocrinol Metab 304(11):E1175-1187. https://doi.org/10.1152/ajpendo.00630.2012
Le Floc’h N, Otten W, Merlot E (2011) Tryptophan metabolism, from nutrition to potential therapeutic applications. Amino Acids 41(5):1195–1205. https://doi.org/10.1007/s00726-010-0752-7
Lerin C, Goldfine AB, Boes T, Liu M, Kasif S, Dreyfuss JM, De Sousa-Coelho AL, Daher G, Manoli I, Sysol JR, Isganaitis E, Jessen N, Goodyear LJ, Beebe K, Gall W, Venditti CP, Patti ME (2016) Defects in muscle branched-chain amino acid oxidation contribute to impaired lipid metabolism. Mol Metab 5(10):926–936. https://doi.org/10.1016/j.molmet.2016.08.001
Li S, Shin HJ, Ding EL, van Dam RM (2009) Adiponectin levels and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA 302(2):179–188. https://doi.org/10.1001/jama.2009.976
Lian K, Du C, Liu Y, Zhu D, Yan W, Zhang H, Hong Z, Liu P, Zhang L, Pei H, Zhang J, Gao C, Xin C, Cheng H, Xiong L, Tao L (2015) Impaired adiponectin signaling contributes to disturbed catabolism of branched-chain amino acids in diabetic mice. Diabetes 64(1):49–59. https://doi.org/10.2337/db14-0312
Liu Y, Turdi S, Park T, Morris NJ, Deshaies Y, Xu A, Sweeney G (2013) Adiponectin corrects high-fat diet-induced disturbances in muscle metabolomic profile and whole-body glucose homeostasis. Diabetes 62(3):743–752. https://doi.org/10.2337/db12-0687
Liu R, Hong J, Xu X, Feng Q, Zhang D, Gu Y, Shi J, Zhao S, Liu W, Wang X, Xia H, Liu Z, Cui B, Liang P, Xi L, Jin J, Ying X, Wang X, Zhao X, Li W, Jia H, Lan Z, Li F, Wang R, Sun Y, Yang M, Shen Y, Jie Z, Li J, Chen X, Zhong H, Xie H, Zhang Y, Gu W, Deng X, Shen B, Xu X, Yang H, Xu G, Bi Y, Lai S, Wang J, Qi L, Madsen L, Wang J, Ning G, Kristiansen K, Wang W (2017) Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Nat Med 23(7):859–868. https://doi.org/10.1038/nm.4358
Maeda K, Okubo K, Shimomura I, Funahashi T, Matsuzawa Y, Matsubara K (1996) cDNA cloning and expression of a novel adipose specific collagen-like factor, apM1 (AdiPose Most abundant Gene transcript 1). Biochem Biophys Res Commun 221(2):286–289. https://doi.org/10.1006/bbrc.1996.0587
Magnusson M, Lewis GD, Ericson U, Orho-Melander M, Hedblad B, Engström G, Ostling G, Clish C, Wang TJ, Gerszten RE, Melander O (2013) A diabetes-predictive amino acid score and future cardiovascular disease. Eur Heart J 34(26):1982–1989. https://doi.org/10.1093/eurheartj/ehs424
Micallef MA, Garg ML (2009) Anti-inflammatory and cardioprotective effects of n-3 polyunsaturated fatty acids and plant sterols in hyper lipidemic individuals. Atherosclerosis 204(2):476–482. https://doi.org/10.1016/j.atherosclerosis.2008.09.020
Nagao K, Kimura T (2020) Use of plasma-free amino acids as biomarkers for detecting and predicting disease risk. Nutr Rev 78(12 Suppl 2):79–85. https://doi.org/10.1093/nutrit/nuaa086
Nakamura H, Jinzu H, Nagao K, Noguchi Y, Shimba N, Miyano H, Watanabe T, Iseki K (2014) Plasma amino acid profiles are associated with insulin, C-peptide and adiponectin levels in type 2 diabetic patients. Nutr Diabetes 4(9):e133. https://doi.org/10.1038/nutd.2014.32
Nelson TL, Stevens JR, Hickey MS (2007) Adiponectin levels are reduced, independent of polymorphisms in the adiponectin gene, after supplementation with alpha-linolenic acid among healthy adults. Metabolism 56(9):1209–1215. https://doi.org/10.1016/j.metabol.2007.04.017
Orasanu G, Plutzky J (2009) The pathologic continuum of diabetic vascular disease. J Am Coll Cardiol 53(5 Suppl):S35-42. https://doi.org/10.1016/j.jacc.2008.09.055
Oxenkrug G (2013) Insulin resistance and dysregulation of tryptophan-kynurenine and kynurenine-nicotinamide adenine dinucleotide metabolic pathways. Mol Neurobiol 48(2):294–301. https://doi.org/10.1007/s12035-013-8497-4
Oxenkrug GF (2015) Increased plasma levels of xanthurenic and kynurenic acids in type 2 diabetes. Mol Neurobiol 52(2):805–810. https://doi.org/10.1007/s12035-015-9232-0
Pozefsky T, Felig P, Tobin JD, Soeldner JS, Cahill GF Jr (1969) Amino acid balance across tissues of the forearm in postabsorptive man effects of insulin at two dose levels. J Clin Investig 48(12):2273–2282. https://doi.org/10.1172/jci106193
Salas-Salvadó J, Bulló M, García-Lorda P, Figueredo R, Del Castillo D, Bonada A, Balanzà R (2006) Subcutaneous adipose tissue cytokine production is not responsible for the restoration of systemic inflammation markers during weight loss. Int J Obes 30(12):1714–1720. https://doi.org/10.1038/sj.ijo.0803348
Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF (1995) A novel serum protein similar to C1q, produced exclusively in adipocytes. J Biol Chem 270(45):26746–26749. https://doi.org/10.1074/jbc.270.45.26746
Shimbo K, Oonuki T, Yahashi A, Hirayama K, Miyano H (2009a) Precolumn derivatization reagents for high-speed analysis of amines and amino acids in biological fluid using liquid chromatography/electrospray ionization tandem mass spectrometry. Rapid Commun Mass Spectrom 23(10):1483–1492. https://doi.org/10.1002/rcm.4026
Shimbo K, Yahashi A, Hirayama K, Nakazawa M, Miyano H (2009b) Multifunctional and highly sensitive precolumn reagents for amino acids in liquid chromatography/tandem mass spectrometry. Anal Chem 81(13):5172–5179. https://doi.org/10.1021/ac900470w
Takehana S, Yoshida H, Ozawa S, Yamazaki J, Shimbo K, Nakayama A, Mizukoshi T, Miyano H (2016) The effects of pre-analysis sample handling on human plasma amino acid concentrations. Clin Chimica Acta 455:68–74. https://doi.org/10.1016/j.cca.2016.01.026
Tochikubo O, Nakamura H, Jinzu H, Nagao K, Yoshida H, Kageyama N, Miyano H (2016) Weight loss is associated with plasma free amino acid alterations in subjects with metabolic syndrome. Nutr Diabetes 6(2):e197. https://doi.org/10.1038/nutd.2016.5
Wang TJ, Larson MG, Vasan RS, Cheng S, Rhee EP, McCabe E, Lewis GD, Fox CS, Jacques PF, Fernandez C, O’Donnell CJ, Carr SA, Mootha VK, Florez JC, Souza A, Melander O, Clish CB, Gerszten RE (2011) Metabolite profiles and the risk of developing diabetes. Nat Med 17(4):448–453. https://doi.org/10.1038/nm.2307
White PJ, Newgard CB (2019) Branched-chain amino acids in disease. Sci (new York, NY) 363(6427):582–583. https://doi.org/10.1126/science.aav0558
Yamakado M, Tanaka T, Nagao K, Ishizaka Y, Mitushima T, Tani M, Toda A, Toda E, Okada M, Miyano H, Yamamoto H (2012) Plasma amino acid profile is associated with visceral fat accumulation in obese Japanese subjects. Clin Obes 2(1–2):29–40. https://doi.org/10.1111/j.1758-8111.2012.00039.x
Yamakado M, Nagao K, Imaizumi A, Tani M, Toda A, Tanaka T, Jinzu H, Miyano H, Yamamoto H, Daimon T, Horimoto K, Ishizaka Y (2015) Plasma free amino acid profiles predict four-year risk of developing diabetes, metabolic syndrome, dyslipidemia, and hypertension in Japanese population. Sci Rep 5:11918. https://doi.org/10.1038/srep11918
Yamamoto Y, Hirose H, Saito I, Nishikai K, Saruta T (2004) Adiponectin, an adipocyte-derived protein, predicts future insulin resistance: two-year follow-up study in Japanese population. J Clin Endocrinol Metab 89(1):87–90. https://doi.org/10.1210/jc.2003-031163
Ziemke F, Mantzoros CS (2010) Adiponectin in insulin resistance: lessons from translational research. Am J Clin Nutr 91(1):258S-261S. https://doi.org/10.3945/ajcn.2009.28449C
Acknowledgements
All the financial source was provided by Ajinomoto Co., Inc., Tokyo. We are grateful to Kumiko Sekiguchi, Noriko Asano, and Takashi Oyamada for their excellent technical support for blood collection and preservation.
Author information
Authors and Affiliations
Contributions
KT, HN, ST, HO, TH and SO designed the research; KT, YI, SM, RY, HO and SO conducted the research. HN and ST analysed the data; YK analysed the amino acid concentrations; HN, ST, KT, MS and SO wrote the paper; and SO had the primary responsibility for the final content. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
KT, YI, SM, HO, HT and SO received research grants from Ajinomoto Co., Inc. HN, ST and YK are employees of Ajinomoto Co., Inc. No other potential conflicts of interest relevant to this article are declared.
Additional information
Handling editor: S. Broeer.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tokunaga, K., Nakamura, H., Toue, S. et al. Plasma free amino acid profiles are associated with serum high molecular weight adiponectin levels in Japanese medical check-up population without type 2 diabetes mellitus. Amino Acids 55, 639–649 (2023). https://doi.org/10.1007/s00726-023-03257-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-023-03257-6