Abstract
Liposomes are nowadays a matter of tremendous interest. Due to their amphiphilic character, various substances with different properties can be incorporated into them and they are especially suitable as a model system for controlled transport of bioactive substances and drugs to the final destination in the body; for example, COVID-19 vaccines use liposomes as a carrier of mRNA. Liposomes mimicking composition of various biological membranes can be prepared with a proper choice of the lipids used, which proved to be important tool in the early drug development. This review deals with commonly used methods for the preparation and characterization of liposomes which is essential for their later use. The alternative capillary electrophoresis methods for physico-chemical characterization such as determination of membrane permeability of liposome, its size and charge, and encapsulation efficiency are included. Two different layouts using liposomes to yield more efficient separation of various analytes are also presented, capillary electrochromatography, and liposomal electrokinetic chromatography.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Liposomes are small spherical vesicles formed by phospholipids and they have been greatly studied since their discovery in 1964, because they can be used to deliver large amounts of substances through the organism to the final destination [1,2,3]. Liposomes are formed by amphiphilic molecules of lipids that assemble in an aqueous environment to form vesicles that encapsulate the aqueous phase at their center [4].
The main advantage of liposomes, as drug carriers, is their composition, which makes them biocompatible, biodegradable, non-toxic, and able to encapsulate both, hydrophilic and hydrophobic drugs [2]. Hydrophilic drugs are present in the aqueous compartment inside the liposome, while highly lipophilic drugs are trapped in the lipid bilayer. The encapsulation efficiency of lipophilic drugs is always higher compared to the hydrophilic ones, because lipophilic drugs are strongly repelled by the aqueous environment on both sides of the membrane and thus are very tightly incorporated into the hydrophobic part of the membrane [5].
Liposomes are used as a transport system for many bioactive materials, such as cytostatics, proteins, peptides, enzymes, DNA, or vaccines [6]. By encapsulating the compound into a liposome, the drug is protected from early inactivation and from the enzymatic processes that commonly occur in the body. Encapsulation into liposomes also reduces the exposure of healthy tissues to the drug [2, 7].
Although liposomes can be used to transport a wide variety of substances, their use in practice is less common. The main reasons are their physico-chemical instability due to oxidation and hydrolysis of phospholipids, low solubility in aqueous solutions, short circulation time in the human body caused by rapid detection by the immune system, and leakage of encapsulated drugs [8].
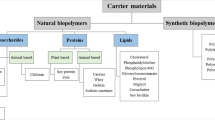
Composition of liposomes
Naturally occurring phospholipids, such as glycerophospholipids, sphingolipids, polysaccharides, sterols, or synthetic lipids, which show higher stability, are most often used in the preparation of liposomes. The hydrophilic part consists of a phosphoric acid residue to which a small organic molecule can be bound. The molecule may be positively charged, negatively charged, or zwitterionic. Liposomes are most often prepared from zwitterionic phospholipids, for example, phosphatidylcholine (PC) and phosphatidylethanolamine (PE), or from negatively charged phospholipids, such as phosphatidylserine (PS), phosphatidylglycerol (PG), phosphatidic acid (PA), and phosphatidylinositol (PI) [4, 9, 10].
Due to the structure of lipids, spontaneous membrane formation occurs in an aqueous medium. The polar parts of phospholipids interact with both external and internal aqueous media, while hydrophobic fatty acid chains interact with each other and their interaction with the aqueous medium is reduced [11, 12].
Classification of liposomes
Size and lamellarity
Liposomes are most often classified according to their size and the number of phospholipid bilayers within the liposome (lamellarity). Based on the number of lamellae, liposomes are divided into unilamellar (single phospholipid bilayer), multilamellar (multiple phospholipid bilayers, diameter greater than 0.5 μm), and multivesicular vesicles (smaller vesicles within the main vesicle, diameter greater than 1 μm). Liposomes with a single phospholipid bilayer are then divided into small unilamellar vesicles (SUVs) with a diameter of 20–200 nm, large unilamellar vesicles (LUVs) with a diameter of 100–1000 nm, and giant unilamellar vesicles (GUVs) with a diameter greater than 1000 nm. Multilamellar vesicles (MLVs) usually contain 5–25 phospholipid bilayers and thus are more suitable for encapsulating hydrophobic drugs. On the other hand, LUVs are more suitable for encapsulating hydrophilic drugs, because they have only one phospholipid bilayer and a much larger volume of aqueous solution within the liposome than SUVs [4, 5, 10, 13, 14].
Composition and use
Based on their composition and use, liposomes can be divided into conventional, cationic, pH-sensitive, long-circulating liposomes, and immunoliposomes [1]. Conventional liposomes, also called the first-generation liposomes, are liposomes containing neutral or negatively charged phospholipids that are used in drug encapsulation studies or as model cell membranes. Their circulation time in the bloodstream is relatively short, because they accumulate in the cells of the immune system [1, 5, 10]. Cationic liposomes composed of positively charged phospholipids are suitable for the transport of negatively charged macromolecules, such as DNA, RNA, or oligonucleotides [1, 5]. pH-sensitive liposomes are destabilized in an acidic environment, which is used for rapid drug release and tumor treatment [15]. Long-circulating liposomes are used to prolong the circulation in the human body, for example by binding a polyethylene glycol (PEG) chain to the phospholipid molecule of liposome. The circulation time can be extended from a few minutes up to several hours, even days in some cases [5, 10]. Finally, immunoliposomes are liposomes, with monoclonal antibodies (or their fragments) bonded to their surface, and thus, they can be detected by cells that have a specific antigen on their surface. Most commonly, long-circulating liposomes are combined with immunoliposomes, where antibodies are bonded to a molecule of PEG [1, 16].
In vivo behavior
Liposomes can be further divided by parameters affecting their in vivo behavior. These parameters include the flowability of the phospholipid bilayer or the surface charge of the liposome. Lipids have a characteristic phase transition temperature Tc. Below this temperature, they are in the gel state, while above this temperature, they are in the fluid state. The flowability of the phospholipid bilayer can be thus affected by using lipids with different Tc values. If lipids with Tc below body temperature are used, the phospholipid bilayer is more fluid, leading to drug leakage from the liposome. On the other hand, liposomes composed of lipids with Tc higher than human body temperature are less fluid, and thus, the drug leakage is suppressed [10, 17].
Another important parameter influencing in vivo behavior of liposomes is the surface charge that may affect the interaction of liposomes with cell membranes. The mechanism of liposome transport into the cells is based on the adsorption to the cell surface and subsequent endocytosis. Negatively charged liposomes are degraded by endocytosis very quickly, while neutral liposomes do not interact with the cells and the drug is thus released extracellularly [17, 18].
Preparation of liposomes
There are many methods for preparing liposomes and the choice of an appropriate method depends on several factors, such as toxicity and concentration of the encapsulated drug, the type of solution used for dispersion of liposomes, size of the liposomes, preparation costs, and finally the encapsulation efficiency of the method [7, 19].
Lipid film hydration method
Hydration of a lipid film is one of the most widely used methods for the preparation of liposomes [20]. To facilitate the formation of the phospholipid bilayer, the temperature of the buffer solution and the temperature during the hydration should be higher than the Tc of the lipid with the highest Tc. However, this temperature should also be taken into consideration in terms of the possible degradation of active substances encapsulated into liposomes. The MLVs of various sizes are produced by intensive shaking and homogenous unilamellar vesicles of uniform size can be formed by sonication or extrusion [21, 22].
Ethanol or ether injection method
Another method of liposome preparation is the ethanol injection method, which is based on rapid injection of the lipid suspension into the aqueous phase. The advantages of this method include the simplicity of the operation and the possibility of preparing a large quantity of liposomes [20, 23, 24]. An alternative to the ethanol injection method is the ether injection method, where lipids are dissolved in diethyl ether and injected into the aqueous phase. Thanks to the higher solubility of lipids in ether, liposomes of higher lipid concentrations can be made using this method [2, 20, 23].
Emulsification method
Finally, liposomes can be prepared by the emulsification method; typically, a technique called reverse-phase evaporation is utilized. This method provides a higher encapsulation efficiency compared to the injection methods [20, 22, 25].
Stability of liposomes
The main difficulty when dealing with liposomes is their low chemical and physical stability. The chemical stability is affected by either oxidation or hydrolysis of phospholipids [26]. They can be protected from oxidation by the addition of antioxidants, by shortening the time of their exposure to the light, or by performing the preparation in a nitrogen or argon atmosphere [22].
The stability of liposomes can also be affected by their size, composition of the phospholipid bilayer, surface charge, or the method of their preparation. Smaller liposomes can pass more easily through the cell membranes; on the other hand, the encapsulation efficiency is decreased and surface energy increased, resulting in lower liposome stability. By the addition of cholesterol (Chol) into the phospholipid bilayer, the stability of the liposome increases due to lower membrane fluidity and lower risk of aggregation, and at the same time, the permeability of the membrane decreases which leads to lower drug leakage [8].
To ensure longer stability, the liposomes are stored in the form of a dry powder obtained by lyophilization, during which cryoprotective agents, such as sucrose, glucose, or trehalose, are added to the liposome preventing the leakage of the encapsulated drug. This method is used for thermolabile drugs which would be degraded by elevated temperature during the heat-drying method [2, 10].
Applications of liposomes
Nowadays liposomes are mainly used for the treatment of cancer, fungal infections, for the transport of analgesics, and in the production of viral vaccines. The first liposome-based product approved by the U.S. Food and Drug Administration in 1995 was Doxil®, which contains encapsulated doxorubicin and is used to treat ovarian and breast cancer [27]. As a result of the COVID-19 pandemic, the research and development activities in the field of liposomes are now globally more intensive than ever. Both Pfizer/BioNTech and Moderna COVID-19 vaccines use cationic liposomes as mRNA carriers into cells, because cationic liposomes and negatively charged mRNA form a stable complex [28]. Liposomes in both vaccines are composed of synthetic cationic or ionizable lipids, distearoyl PC, and Chol. The PEG-2000 is bound to one of the lipids in both vaccines and is believed to be responsible for some allergic reactions, as it is known that human body can develop immunity against PEG [28,29,30].
Analysis and characterization of liposomes
To ensure the proper function of liposomes as carriers for bioactive substances, it is necessary to characterize their properties, such as size, lamellarity, surface charge, quantitative composition, and encapsulation efficiency [31]. Commonly used methods to analyze and characterize liposomes include 31P nuclear magnetic resonance (NMR) [32] which is used for studying the membrane fluidity and thermotropic phase transitions, dynamic light scattering (DLS) [33], atomic force microscopy (AFM) [34], fluorescence spectroscopy [35], high-performance liquid chromatography (HPLC) [36], capillary electrophoresis (CE) [4], and others.
Size and lamellarity
Liposome size is mostly determined by transmission electron microscopy (TEM), DLS, AFM, and size-exclusion chromatography (SEC) [37]. A general disadvantage of the TEM method is that negative staining with osmium oxide or uranyl acetate changes the structure of the liposome [31]. Cryo-TEM represents an alternative that, unlike TEM, does not require the staining and fixation of the samples, which makes it more suitable for size characterization [38].
In the DLS method, the light of a laser beam is scattered depending on the size and shape of the liposomes. By analyzing the fluctuations in light intensity caused by the Brownian motion of liposome particles in solution, the diffusion coefficients can be obtained that are related to the hydrodynamic size of the liposomes [39].
Other methods for liposome size determination are SEC and high-performance SEC. By these methods, liposomes can be separated from free analytes and at the same time divided into groups based on their size [40]. The main disadvantage of SEC is the loss of lipids due to their adsorption in the gel. To overcome this problem, the gel can be saturated with lipids before the analysis using small, sonicated liposomes [40,41,42].
Encapsulation efficiency
Encapsulation efficiency is defined as the ratio of the amount of the encapsulated substance in the liposome to the total weighed substance [43]. To determine the encapsulation efficiency, the free drug is separated from the liposome-encapsulated one by dialysis, gel filtration, or centrifugation. However, these methods can cause liposome destruction and release of the encapsulated drug. Among them, dialysis is the most gentle, but also the most time-consuming and instrumentally challenging one [44, 45]. Gel filtration and centrifugation are thus used more often. After the separation of the encapsulated and free drug, the membrane of the liposome is disrupted and the amount of released encapsulated substance is determined by fluorescence spectroscopy, enzymatic, or electrochemical methods [37].
Quantitative composition
Most of the methods used to determine the quantitative composition, such as the determination of total phosphate content or the amount of Chol in the membrane, are based on the formation of colored products, which can be then determined spectrophotometrically. A method called Bartlett decomposition is used to determine the total phosphate content where the phosphate is transformed to the inorganic form and creates a blue product after reaction with ammonium molybdate [37, 46].
The amount of Chol in liposomes can be determined by enzymatic methods. The hydrolysis of the cholesterol ester produces free Chol, which is then oxidized by cholesterol oxidase to hydrogen peroxide. The hydrogen peroxide reacts with 4-aminoantipyrine and phenol creating a colored product [37].
Proliposomes
Attempts to overcome the above-mentioned disadvantages of liposomes (low physical and chemical stability, leakage of encapsulated substance, hydrolysis, oxidation, and aggregation) led in 1986 to the discovery of proliposomes. In contrast to liposomes, proliposomes exhibit high stability. They are dry, free-flowing particles formed by phospholipids, a porous powder, and the drug [47,48,49]. Upon contact with the aqueous phase or with body fluids, they form a suspension of liposomes. The phospholipids commonly used for proliposome preparation are phosphatidylcholine and phosphatidylglycerol. Proliposomes also contain water-soluble porous carriers such as sorbitol, mannitol, or microcrystalline cellulose [47].
Liposomes and capillary electrophoresis
Capillary electromigration methods are suitable for the study of liposomes, because they exhibit several advantageous features, such as low sample consumption, fast and efficient separations, and a high degree of automation [4, 50]. Capillary electrophoresis is a method suitable for characterizing the drug–liposome interactions, for determination of encapsulation efficiency, for studying the drug leakage from liposomes, as well as for liposomes characterization (e.g., size, surface charge, and permeability of the phospholipid membrane) [4].
Determination of membrane permeability
Permeability of liposome membrane is a key parameter that must be determined when studying liposomes to prevent undesired leakage of encapsulated substances during their circulation in the bloodstream [51]. Tsukagoshi et al. [52] analyzed liposomes composed of dipalmitoyl PC with encapsulated dyes, eosin Y and rhodamine B, by CE with chemiluminescence detection. The dependence of the liposome stability and its membrane permeability on the concentration of encapsulated buffer was monitored by the separation, detection, and quantitation of free and encapsulated dye. Liposomes were dispersed in 10 mM carbonate buffer (pH = 9.0), while within them, eosin Y in carbonate or phosphate buffer of different concentrations was encapsulated. The peak area ratio of free eosin Y to encapsulated eosin Y was then calculated from obtained electropherograms. The higher the ratio, the greater was the permeability of the liposome membrane. The peak area ratio, and thus the permeability, was greater when the concentration of encapsulated carbonate buffer was lower than the concentration of carbonate buffer used to disperse the liposomes. The authors hypothesized that water was released from the liposome to equalize the concentration of carbonate buffer to maintain the osmotic balance. This resulted in shrinkage of liposome with subsequent release of the encapsulated dye.
Franzen et al. [53] used CE to study the effectiveness of oxaliplatin encapsulation and the drug leakage from the PEGylated liposome. The liposomes’ samples were sonicated by a sonication probe to induce faster leakage of the drug and the electropherograms (Fig. 1) showed an increased peak of free oxaliplatin and decreased peak of encapsulated oxaliplatin with increasing sonication time. The authors assumed that the disappearance of the liposome peak was caused by the complete release of encapsulated oxaliplatin rather than the destruction of the liposome. Using DLS, they found that liposome particle size decreased with increasing sonication time.

Reprinted and modified with permission from Ref. [51]
Release of encapsulated oxaliplatin from PEGylated liposome with increasing sonication time.
Determination of size and charge
Although CE is not a widely used method for the determination of liposome size, Duffy et al. [54] used CE with laser-induced fluorescence detection (CE-LIF) to study the properties of liposomes, including their size. To eliminate the electroosmotic flow (EOF) and to reduce the adsorption of the liposomes to the capillary wall, the capillary was coated with poly(acryloylaminopropanol). Liposomes prepared from PC, PS, PE, and Chol were dispersed in 2.5 mM sodium tetraborate (pH = 9.3) and the encapsulated substance was 10 μM fluorescein. They were able to calculate the volume of solution captured in liposomes and thus calculate the radius of the liposome from corrected fluorescence intensity, fluorescein concentration in the liposomes, and detector sensitivity.
Radko et al. [55] measured mobilities of liposomes composed of PC/PG/Chol in various ratios by extrusion and non-extrusion methods leading to the formation of liposomes with the diameter range from 125 to 488 nm. Based on the measurements of free and encapsulated fluorescein in the capillary coated with 3% non-crosslinked polyacrylamide in the Tris–HCl background electrolyte (BGE) of the different ionic strength, they determined that the electrophoretic mobility is size-dependent (Fig. 2).

Reprinted and modified with permission from Ref. [53]
Electropherograms showing the size-dependent separation of liposomes varying in their size in 3% linear polyacrylamide gel matrix. Numbers in ovals show ionic strength of Tris–HCl background electrolyte.
For determination of the liposome charge, Wiedmer et al. [56] used CE with UV/Vis detection at 200 nm to measure the electrophoretic mobility of liposomes and DLS to determine the liposome size. The liposomes were composed of palmitoyloleoyl (PO), PC, and PS in various molar ratios and they were dispersed in 50 mM 2-(N-cyclohexylamino)ethanesulfonic acid (pH = 9.0). The charge was calculated from electrophoretic mobility, size of the liposome, and the known value of buffer viscosity. The results confirmed the presumption that the higher the content of negatively charged lipids in the liposome, the greater the charge of the liposome.
Determination of free and encapsulated drugs
Capillary electrophoresis can also be used to study the liposomes as a drug transport system and to determine the amount of free and encapsulated drug [4]. Liposomes are very often used as carriers for toxic drugs, and it is thus crucial to develop a method for simple and fast determination of encapsulated and free drugs, which could be toxic for the organism. Ansar et al. [57] used CE to separate free and encapsulated doxorubicin in 20 mM phosphate buffer (pH = 6.5) with 10% sucrose as a BGE. Free doxorubicin was determined from the calibration curve by measuring the sample with fluorescein used as an internal standard due to its high stability in phosphate buffer and high absorption coefficient. The total amount of doxorubicin was determined after its release from the liposome using Triton X-100 detergent for membrane disruption.
Another example of the determination of free and encapsulated substances is a study by Chen et al. [58]. They encapsulated oligonucleotides into large neutral or positively charged liposomes, because neutral liposomes do not migrate in the electric field and positively charged liposomes migrate very slowly in the opposite direction than negatively charged oligonucleotides. Free oligonucleotides could thus be separated from the encapsulated ones due to their migration to the anode. To determine total oligonucleotides, liposomes were disrupted by phenol–chloroform extraction, or by Triton X-100 detergent.
Nguyen et al. [59] developed a CE method coupled with MS detection that has a high potential in pharmaceutical quality control and in drug development. They were able to determine the encapsulation efficiency, the stability of liposomes, and the leakage of encapsulated drug from the liposome into the human plasma. The drug release in human plasma was measured before and after incubation of liposome with encapsulated cisplatin (the amount of free and encapsulated cisplatin and total cisplatin were determined in one run), the stability of liposome was measured after incubation at 37 °C, and the triggered release of encapsulated drug into human plasma was measured after sonication.
Capillary electrochromatography and liposomal electrokinetic chromatography
Apart from being analyzed and characterized by CE, liposomes can also be used to facilitate separations. For this purpose, they can be used in two different layouts, capillary electrochromatography (CEC), or liposomal electrokinetic chromatography (LEKC). CEC combines the features of CE and HPLC. Liposomes are used to coat the capillary wall forming thus a stationary phase. By applying voltage, the EOF is generated and it carries the mobile phase with analytes through the capillary. The charged compounds are separated not only by their different electrophoretic mobilities but also due to their distribution between the mobile and the liposomal stationary phases [60,61,62]. To coat the capillary wall with liposomes, the capillary can be simply flushed by them, or the avidin–biotin technique can be used. The latter is based on the strong electrostatic interaction between biotin present on the surface of the liposome and the avidin protein, which is bound to the coated capillary wall (usually coated with agarose) [63]. However, the liposomes with biotin are relatively expensive and bound biotin changes the liposome characteristics. Additionally, the avidin–biotin complex creates a new undesired place where analytes can interact and thus interfere with the drug–lipid interactions in the capillary. Another technique for coating of the capillary wall includes covalent attachment of liposomes after wall activation by 4-nitrophenyl chloroformate [64,65,66]. The main advantages of CEC over HPLC include higher separation efficiency, low sample consumption, and low analysis costs [61].
Godyń et al. [67] used CEC for studying the blood–brain barrier permeability of different compounds. Prior to the analysis of 25 drug compounds, the capillary was coated with POPC/PS (80:20 mol%) liposomes representing the natural composition of the phospholipid bilayer of the blood–brain barrier. They coated the capillary by flushing it 10 min with 0.5 M HCl, 15 min with water, and then 10 min with liposomes and based on the EOF marker measurements found out that the EOF in the coated capillary was suppressed. They compared the data from CEC to parallel artificial membrane permeability assay as a widely used method. Based on their research and in vivo data of the studied compounds, they concluded that CEC as a relatively fast and inexpensive method could be used as an alternative screening method in early drug development.
In the case of LEKC, the liposomes are added directly to BGE creating a pseudo-stationary phase [68]. This method is based on the same principle as micellar electrokinetic chromatography. The separation of the analytes occurs due to their distribution between the aqueous mobile phase and the liposomal pseudo-stationary phase [69, 70]. Nakamura et al. [71] successfully used the LEKC to separate hydrophobic neutral analytes, namely, biphenyl and naphthalene. Liposomes added to the BGE were composed of dimyristoyl PC and dimyristoyl PG in 10 mM Tris–HCl buffer with 50 mM NaCl (pH = 7.0). Without liposomes in the BGE, both analytes migrated together with EOF and thus were not separated. After the addition of the liposomes to the BGE, the analytes were baseline separated based on their distribution between the two phases.
Wiedmer et al. [72] used LEKC to separate neutral steroid hormones using BGE containing negatively charged liposomes composed of POPC, PS, and Chol of different ratios creating the pseudo-stationary phase. They used bare fused silica capillary despite acknowledging that some quantity of liposomes may be adsorbed to the capillary wall and thus act as a stationary phase, which results in a combination of LEKC and CEC techniques. They also used polyacrylamide coated capillary with suppressed EOF with the same BGEs to avoid liposome adsorption to the wall and faster separation of more hydrophobic steroids. The differences in the interactions between steroids and liposomes with increasing amount of cholesterol were observed.
The main asset of the LEKC is the possibility to simulate and study the interactions of drugs with cell membranes, since liposomes are structurally very similar to them [73]. Lipophilicity plays a significant role when formulating a drug, allowing the drug to pass through the phospholipid bilayer of the membrane. The octanol–water partition coefficient Pow is widely used to quantify the lipophilicity of drugs. However, this parameter is not suitable for the prediction of the drug–membrane interactions. Charged drugs interact with membranes due to both, the hydrophobic and electrostatic interactions. Their Pow value can thus be rather low, but they can still relatively strongly interact with liposomes due to the electrostatic interactions. LEKC proved to be a suitable method for studying the complex interactions between drugs and cell membranes simulated by liposome membranes [74, 75]. Carozzino and Khaledi [73] investigated the influence of the type and concentration of the buffer, its ionic strength, and liposome composition on separation of neutral (phenol) and positively charged (drugs including tetracaine and lidocaine) compounds by LEKC using negatively charged liposomes. They found out that none of the parameters mentioned above affected the partition coefficients of the neutral analytes. On the other hand, the partition coefficients of the positively charged analytes decreased with increasing ionic strength, because the electrostatic interactions between analytes and the liposomes were screened by their interactions with the higher number of counter-ions in the solution. At the same time, the Pow partition coefficient increased with the increasing content of negatively charged lipids present in liposomes, because the electrostatic interaction between positively charged liposomes and negatively charged liposomes increased. All liposomes used to study the effect of liposome composition were prepared with the same concentration of Chol (30% of total lipid concentration) and different combinations of other phospholipids such as dipalmitoyl PC, dipalmitoyl PG, dipalmitoyl PS, dipalmitoyl PE, phosphatidylinositol, and sphingomyelin.
Burns and Khaledi [68] developed a fast LEKC method for determination of liposome–water partition coefficient Klw, which better corresponds with cell membranes, as the composition and structure of liposomes are closer to cell membranes than to octanol. The method utilizes the fact that LEKC retention factors calculated from migration times are directly proportional to liposome–water partition coefficient. Studying drug–membrane interactions by LEKC takes only few minutes in opposite to conventional methods, which can take up to days. To validate the method, the authors calculated Klw values from two quantitative structure–partition relationship models and showed great agreement between the experimentally obtained and predicted values. One of the two models was based on the relationship between Klw and Pow and the other was the linear solvation energy relationship (LSER). The strong correlation between the Klw values for uncharged aromatic compounds obtained from LEKC measurements and from LSER prediction is shown in Fig. 3.

Reprinted and modified with permission from Ref. [66]
Correlation between the Klw values of uncharged aromatic compounds obtained from LEKC and predicted by LSER.
Ruokonen et al. [76] studied the effect of temperature (at 25, 37, and 42 °C) on distribution constants Klw of local anesthetics by LEKC using liposomes of three different compositions as pseudo-stationary phase. One type of the liposomes was formed by lipids from human red blood cells for better correspondence with the natural composition of cell membranes. No correlation between temperature and distribution constant of anesthetics was found for any of the tested liposomes; however, the Klw values slightly increased with elevated temperature in most cases. On the other hand, they determined that the Klw values are dependent on the amount of Chol and charged lipids, and surprisingly, the data obtained when using LEKC with red blood cells liposomes showed up to three times lower Klw constants than when using liposomes composed of POPC/POPG or POPC/POPG/Chol, indicating that selection of liposomes for LEKC plays a significant role when conclusions for the in vivo interactions of drugs with cell membranes are to be drawn.
Conclusion
The properties of liposomes, such as their composition, size, and preparation technology, determine their overall stability, their behavior in the body, as well as their utility as drug carriers. These parameters are crucial in the early drug development and quality control of new products. Capillary electrophoresis methods proved to be promising alternative to the commonly used ones. The main advantages of CE include the possibility of studying the liposome–drug interactions directly inside the separation capillary, which combined with the high degree of automation, several detection techniques available, and short analysis times, make CE a versatile tool for comprehensive analysis and characterization of liposomes. The low sample and buffer consumption, along with the scarce use of organic solvents, results in low operational costs and environmental friendliness of CE methods. Based on the above-mentioned, further development and increasing number of CE applications can be expected, especially in the area of LEKC modeling of drug–cell membrane interactions and LEKC investigation of controlled drug release.
References
Storm G, Crommelin DJA (1998) Pharm Sci Technol Today 1:19
Akbarzadeh A, Rezaei-Sadabady R, Davaran S, Joo SW, Zarghami N, Hanifehpour Y, Samiei M, Kouhi M, Nejati-Koshki K (2013) Nanoscale Res Lett 8:102
Daraee H, Etemadi A, Kouhi M, Alimirzalu S, Akbarzadeh A (2016) Artif Cells Nanomed Biotechnol 44:381
Franzen U, Østergaard J (2012) J Chromatogr A 1267:32
Has C, Sunthar P (2020) J Liposome Res 30:336
Carugo D, Bottaro E, Owen J, Stride E, Nastruzzi C (2016) Sci Rep 6:25876
Bozzuto G, Molinari A (2015) Int J Nanomed 10:975
Nakhaei P, Margiana R, Bokov DO, Abdelbasset WK, Jadidi Kouhbanani MA, Varma RS, Marofi F, Jarahian M, Beheshtkhoo N (2021) Front Bioeng Biotechnol 9:705886
Large DE, Abdelmessih RG, Fink EA, Auguste DT (2021) Adv Drug Deliv Rev 176:113851
Guimarães D, Cavaco-Paulo A, Nogueira E (2021) Int J Pharm 601:120571
Roberts MA, Locascio-Brown L, Maccrehan WA, Durst RA (1996) Anal Chem 68:3434
Isalomboto Nkanga C, Murhimalika Bapolisi A, Ikemefuna Okafor N, Werner Maçedo Krause R (2019) Liposomes—advances and perspectives. IntechOpen, London
Farooque F, Wasi M, Mughees MM (2021) J Drug Deliv Ther 11:149
Giuliano CB, Cvjetan N, Ayache J, Walde P (2021) ChemSystemsChem 3:202000049
Paliwal SR, Paliwal R, Vyas SP (2015) Drug Deliv 22:231
Eloy JO, Petrilli R, Trevizan LNF, Chorilli M (2017) Colloids Surf B 159:454
Sharma A (1997) Int J Pharm 154:123
Miller CR, Bondurant B, McLean SD, McGovern KA, O’Brien DF (1998) Biochemistry 37:12875
Gonzalez Gomez A, Hosseinidoust Z (2020) ACS Infect Dis 6:896
Šturm L, Poklar Ulrih N (2021) Int J Mol Sci 22:6547
Lasic DD (2019) Liposomes in gene delivery. CRC Press, Boca Raton
Vemuri S, Rhodes CT (1995) Pharm Acta Helv 70:95
Kanda H, Katsube T, Wahyudiono, Goto M (2021) Foods 10:1789
Gouda A, Sakr OS, Nasr M, Sammour O (2021) J Drug Deliv Sci Technol 61:10217
Cortesi R, Esposito E, Gambarin S, Telloli P, Menegatti E, Nastruzzi C (1999) J Microencapsul 16:251
Grit M, Crommelin DJA (1993) Chem Phys Lipids 64:3
Bulbake U, Doppalapudi S, Kommineni N, Khan W (2017) Pharmaceutics 9:12
Attia MA, Essa EA, Elebyary TT, Faheem AM, Elkordy AA (2021) Pharmaceuticals 14:1173
Gregoriadis G (2021) Med Drug Discov 12:100104
Schoenmaker L, Witzigmann D, Kulkarni JA, Verbeke R, Kersten G, Jiskoot W, Crommelin DJA (2021) Int J Pharm 601:120586
Chen C, Zhu S, Huang T, Wang S, Yan X (2013) Anal Methods 5:2150
Doyen C, Larquet E, Coureux PD, Frances O, Herman F, Sablé S, Burnouf JP, Sizun Ch, Lescop E (2021) Mol Pharm 18:2521
Ruf H, Georgalis Y, Grell E (1989) Dynamic laser light scattering to determine size distributions of vesicles. Elsevier, Amsterdam
Liang X, Mao G, Ng KYS (2004) J Colloid Interface Sci 278:53
Metso AJ, Mattila JP, Kinnunen PK (2004) Biochim Biophys Acta 1663:222
Oswald M, Platscher M, Geissler S, Goepferich A (2016) Int J Pharm 497:293
Edwards KA, Baeumner AJ (2006) Talanta 68:1432
Almgren M, Edwards K, Karlsson G (2000) Colloids Surf A Physicochem Eng Asp 174:3
Stetefeld J, McKenna SA, Patel TR (2016) Biophys Rev 8:409
Grabielle-Madelmont C, Lesieur S, Ollivon M (2003) J Biochem Biophys Methods 56:189
Sun Y, Shi QH, Zhang L, Zhao GF, Liu FF (2011) Comprehensive biotechnology, 2nd edn. Elsevier, Amsterdam
Ruysschaert T, Marque A, Duteyrat JL, Lesieur S, Winterhalter M, Fournier D (2005) BMC Biotechnol 5:11
Zhang XM, Patel AB, de Graaf RA, Behar KL (2004) Chem Phys Lipids 127:113
Zhang G, Sun J (2021) Int J Nanomed 16:7391
Ohnishi N, Yamamoto E, Tomida H, Hyodo K, Ishihara H, Kikuchi H, Tahara K, Takeuchi H (2013) Int J Pharm 441:67
Kanásová M, Nesměrák K (2017) Monatsh Chem 148:1581
Singh N, Kushwaha P, Ahmad U, Abdullah M (2019) Ars Pharm 60:231
Muneer S, Masood Z, Butt S, Anjum S, Zainab H, Anwar N, Ahmad N (2017) J Nanomed Nanotechnol 8:3
Manjula D, Shabaraya A, Somashekar S (2014) Int J Pharm Sci Invent 3:6
Wiedmer SK, Shimmo R (2009) Electrophoresis 30:240
Nasr G, Greige-Gerges H, Elaissari A, Khreich N (2020) Int J Pharm 580:119198
Tsukagoshi K, Okumura Y, Nakajima R (1998) J Chromatogr A 813:402
Franzen U, Nguyen TT, Vermehren C, Gammelgaard B, Østergaard J (2011) J Pharm Biomed Anal 55:16
Duffy CF, Gafoor S, Richards DP, Admadzadeh H, O’Kennedy R, Arriaga EA (2001) Anal Chem 73:1855
Radko SP, Stastna M, Chrambach A (2000) Anal Chem 72:5955
Wiedmer SK, Hautala J, Holopainen JM, Kinnunen PK, Riekkola ML (2001) Electrophoresis 22:1305
Ansar SM, Jiang W, Mudalige T (2018) Int J Pharm 549:109
Chen D, Cole DL, Srivatsa GS (2000) J Pharm Biomed Anal 22:791
Nguyen TT, Østergaard J, Stürup S, Gammelgaard B (2013) Int J Pharm 449:95
Bilek G, Kremser L, Blaas D, Kenndler E (2006) J Chromatogr B 841:38
Colón LA, Reynolds KJ, Alicea-Maldonado R, Fermier AM (1997) Electrophoresis 18:2162
Yan C, Xue Y, Wang Y (2018) Capillary electromigration separation methods. Elsevier, Amsterdam
Wiedmer SK, Riekkola ML, Jussila MS (2004) Trends Anal Chem 23:562
Lokajová J, Tiala H, Viitala T, Riekkola ML, Wiedmer SK (2011) Soft Matter 7:6041
Mao X, Kong L, Li X, Guo B, Zou H (2003) Anal Bioanal Chem 375:550
Örnskov E, Ullsten S, Söderberg L, Markides KE, Folestad S (2002) Electrophoresis 23:3381
Godyń J, Gucwa D, Kobrlova T, Novak M, Soukup O, Malawska B, Bajda M (2020) Talanta 217:121023
Burns ST, Khaledi MG (2002) J Pharm Sci 91:1601
Wang Y, Sun J, Liu H, Liu J, Zhang L, Liu K, He Z (2009) Analyst 134:267
Terabe S, Kim JB (2005) Encyclopedia of analytical science, 2nd edn. Elsevier, Amsterdam
Nakamura H, Sugiyama I, Sano A (1996) Anal Sci 12:973
Wiedmer SK, Jussila MS, Holopainen JM, Alakoskela J, Kinnunen PKJ, Riekkola M (2002) J Sep Sci 25:427
Carrozzino JM, Khaledi MG (2004) Pharm Res 21:2327
Liu Z, Wang S, Hu M (2009) Developing solid oral dosage forms. Elsevier, Amsterdam
Liu X, Testa B, Fahr A (2011) Pharm Res 28:962
Ruokonen SK, Duša F, Rantamäki AH, Robciuc A, Holma P, Holopainen JM, Abdel-Rehim M, Wiedmer SK (2017) J Chromatogr A 1479:194
Acknowledgements
The authors are grateful for the financial support provided by the Grant Agency of Charles University (No. 386122). This review was also supported in part by the Charles University project SVV260560 and Central European Exchange Program for University Studies, network RO-0010-16-2122—Teaching and Learning Bioanalysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tomnikova, A., Orgonikova, A. & Krizek, T. Liposomes: preparation and characterization with a special focus on the application of capillary electrophoresis. Monatsh Chem 153, 687–695 (2022). https://doi.org/10.1007/s00706-022-02966-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00706-022-02966-0