Abstract
Mass methanol poisonings present a serious problem for health systems worldwide, with poor outcome associated with delayed treatment. Positive pre-hospital serum ethanol concentration may have predictive value as the prognostic factor of the treatment outcome. We studied the effect of positive serum ethanol level on admission to hospital on survival in patients treated during the Czech methanol outbreak during 2012–2014. Cross-sectional cohort study was performed in 100 hospitalized patients with confirmed methanol poisoning. Pre-hospital ethanol was administered in 42 patients (by paramedic/medical staff to 30 patients and self-administered by 12 patients before admission); 58 patients did not receive pre-hospital ethanol. Forty-two patients had detectable serum ethanol concentration on admission to hospital [median 18.3 (IQR 6.6–32.2) mmol dm−3]. Pre-hospital ethanol administration by paramedic/medical staff had a significant effect on survival without visual and CNS sequelae when adjusted for arterial blood pH on admission (OR 8.73; 95 % CI 3.57–21.34; p < 0.001). No patients receiving pre-hospital ethanol died compared with 21 not receiving (p < 0.001). Positive serum ethanol concentration on admission to hospital was a predictor for survival without health sequelae when adjusted for arterial blood pH (OR 8.10; 95 % CI 2.85–23.02; p < 0.001). The probability of visual and CNS sequelae in survivors reduced with increasing serum ethanol concentration on admission.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mass and cluster acute methanol poisonings due to the consumption of illicit alcohol occur frequently throughout the world [1–4]. Sporadic methanol poisonings occur either intentionally through the abuse of methanol-containing fluids or attempted suicide or unintentionally through the misuse or occupational accident with products containing methanol as a solvent [5–7]. In the absence of protective ethanol concentration in blood serum, methanol is metabolized by hepatic alcohol dehydrogenase enzyme (cytosolic ADH1) to the highly toxic formic acid, which inhibits mitochondrial respiration [8, 9]. The accumulation of formic acid leads to the metabolic acidosis with anion gap increase, optic nerve and retinal nerve fibers damage, and necrosis of basal ganglia [10–13]. Ethanol as an antidote prevents the toxic metabolite formation by competitive blocking the ADH; therefore, its timely administration is important for successful treatment [14].
Ethanol has 10–12 times higher affinity for ADH than methanol and its serum concentration of 22–33 mmol dm−3 is sufficient to completely block the metabolism of methanol to formaldehyde, and on the second step to formate [15, 16]. In hospitals, the indications for ethanol administration are either a documented plasma methanol concentration of more than 6.2 mmol dm−3, a high osmolal gap with documented the recent history of ingesting toxic amounts of methanol, or a metabolic acidosis with history or strong clinical suspicion of poisoning [17, 18].
To prevent high morbidity and mortality of methanol poisoning, ethanol should be administered as soon as possible after methanol ingestion [14, 19]. Its wide availability in the community makes it suitable antidote for a pre-hospital ‘first aid’ in the cases of suspicious toxic alcohol ingestion. We addressed this question during a recent methanol mass poisoning in the Czech Republic [20, 21]. In this study, we aimed to evaluate serum ethanol concentration on admission to hospital as the factor predictive of treatment outcome in patients with acute methanol poisoning during a methanol epidemic.
Results and discussion
During the Czech mass methanol poisoning outbreak in 2012–2014, 137 patients were poisoned and 106 of them were treated in hospitals. Of them, blood samples for serum ethanol measurement were not taken before hospital antidote treatment with intravenous ethanol, in six patients. Since serum ethanol concentration on admission before hospital treatment was the key variable for the study, these six patients were excluded from further analysis. The patients who died outside hospital (n = 31) were excluded from the study. Thus, 100 patients with median age 54 (interquartile range, IQR 38–61) years, 79 males and 21 females, were included in the study.
The administration of pre-hospital ethanol was identified in detailed histories taken on admission by research staff (corroborated by the laboratory analysis). Thirty patients received pre-hospital ethanol from medical or paramedical staff and twelve patients self-administered ethanol shortly before admission to hospital. The remaining 58 patients did not receive pre-hospital ethanol from any sources before presentation.
Demographic and laboratory admission data are presented in Table 1, separated according to outcome. Severity of metabolic acidosis in the patients on admission to hospital is characterized by arterial blood pH, pCO2, HCO3−, base deficit (BD), anion gap (AG), and serum lactate (Table 2). Data are presented as medians with IQR, because serum methanol, ethanol (EtOH), and osmolal gap (OG) in all groups, pH and lactate in Group I, and pCO2 and AG in Group III were not normally distributed. Forty-two patients had detectable ethanol before hospital antidote treatment, with a median concentration of 18.3 mmol dm−3 (IQR 6.6–32.2 mmol dm−3). The median serum ethanol on admission in the patients with pre-hospital administration by paramedics/medical staff was 18.3 mmol dm−3 (IQR 7.1–28.1 mmol dm−3). The median serum ethanol on admission in the patients with pre-hospital self-administration was higher: 30.6 mmol dm−3 (6.4–81.9 mmol dm−3). The serum methanol concentration on admission in EtOH-positive patients did not statistically differ from that in EtOH-negative patients; however, they were less acidotic and had lower serum glucose concentration on admission.
Clinical features on admission included visual and gastrointestinal disturbances, dyspnea, chest pain, and coma in most severely poisoned patients (Table 3). Other features included fatigue, headache, dizziness, somnolence, anxiety, alcoholic delirium, tremor, seizures, and cardiac and respiratory arrest. The median ethanol concentration was higher in patients without clinical symptoms on admission [10.9 mmol dm−3 (1.1–29.8 mmol dm−3)] than in those with clinical features [0 mmol dm−3 (0–5 mmol dm−3); p = 0.014]. Detailed information about the post-admission treatment given in hospitals is presented in Table 4.
Outcome and prognosis
EtOH-positive patients had a lower rate of mortality and a higher rate of survival without visual and CNS sequelae than EtOH-negative patients (all p < 0.001; Table 5).
A strong positive correlation was found between the pre-hospital ethanol administration by paramedics/medical staff and serum ethanol concentration on admission (r = 0.713, p < 0.001). Furthermore, strong positive correlations were found between the serum ethanol on admission and:
-
(a)
survival versus death (r = 0.418, p < 0.001);
-
(b)
survival without sequelae versus poor outcome (death or survival with sequelae; r = 0.711, p < 0.001); and
-
(c)
survival without sequelae versus survival with sequelae versus death (r = 0.693, p < 0.001).
These correlations were strong and significant for the variable “pre-hospital ethanol administration by paramedics/medical staff” for all three variants of outcome division as well (r = 0.338; r = 0.537; and r = 0.531, respectively; all p < 0.001). In spite of the fact that there was no difference in the state-of-consciousness on the arrival of paramedics/medical staff, most of the patients with Glasgow coma scale (GCS) under 10 were not administered ethanol. Even after excluding the patients with low GCS (under 10) from the analyzed data set, the association remained significant:
-
(a)
survival versus death (r = 0.355; p = 0.001);
-
(b)
survival without sequelae versus poor outcome (death or survival with sequelae; r = 0.689, p < 0.001); and
-
(c)
survival without sequelae versus survival with sequelae versus death (r = 0.681; p < 0.001).
In the univariate analysis, both serum ethanol concentration on admission and pre-hospital ethanol administration by paramedics/medical staff were significant variables for survival without sequelae (Table 6). In the bivariate regression models, the combinations of either variable, “serum ethanol on admission”, and “pre-hospital ethanol administration” with the variable “arterial blood pH on admission” explained 55.4 and 48.9 % of dispersion in treatment outcomes, respectively (Table 7).
The patients with positive serum ethanol on admission had the odds ratio of survival without sequelae versus poor outcome (death or sequelae) of 8.10 (2.85–23.02 95 % CI; p < 0.001) when adjusted on the degree of acidemia (arterial blood pH on admission).
Furthermore, the patients with pre-hospital ethanol administration by paramedics/medical staff had the odds ratio of survival without sequelae versus poor outcome (death or sequelae) of 8.73 (3.57–21.34 95 % CI; p < 0.001) when adjusted on arterial blood pH on admission. Inclusion of any other independent variable in the logistic regression model did not lead to further increase of its ability to explain the dispersion in treatment outcomes.
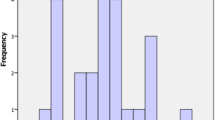
The univariate and bivariate regression models for three variants of treatment outcome analyzed separately (survival without sequelae versus survival with sequelae versus death) are presented on Fig. 1. Serum ethanol concentration on admission, severity of metabolic acidosis, and pre-hospital ethanol administration (“first aid”) are the most significant variables for the outcome of treatment.
Percents of explained dispersion in univariate and bivariate ordinal multinomial models for three categories of treatment outcomes (survival without sequelae versus survival with sequelae versus death). For the univariate models, see parameters and per cents inside the circles; for bivariate models, see per cents on the lines connecting parameters. S-EtOH, serum ethanol concentration on admission; pH, arterial blood pH on admission; HCO3−, arterial blood bicarbonate on admission; “First aid”, pre-hospital ethanol administration by paramedics/medical staff; GCS, Glasgow coma scale; S-Lactate, serum lactate on admission; Time, time span between methanol ingestion and the treatment; S-MetOH, serum methanol on admission; Antidote (EtOH), hospital administration of ethanol; Antidote (Fomepizole), hospital administration of fomepizole
The logistic regression of probability of death or survival with sequelae versus concentration of serum ethanol and arterial blood pH on admission is shown in Fig. 2. The probability of death decreased exponentially with the increase of arterial blood pH. All who died had negative serum ethanol on admission; however, the probability of developing sequelae among the survivors was dependent not only on the degree of acidemia, but also on the serum ethanol concentration on admission, with a significant leftward shift of the peak of the curve. This implies that an increasing ethanol concentration was protective against visual and CNS damage given the same arterial blood pH. For example, the patients with arterial blood pH 7.0: the probability of developing sequelae was 59 % (negative serum ethanol) versus 41 % (serum ethanol <11 mmol dm−3) versus 16 % (serum ethanol >11 mmol dm−3).
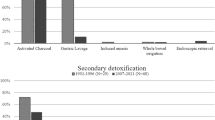
The logistic regression of probability of poor outcome (death or sequelae) in the patients with pre-hospital ethanol administration by the paramedics/medical staff versus probability in the patients without pre-hospital ethanol administration is shown in Fig. 3.
Serum ethanol on admission and prognostic parameters of treatment outcome
The poor outcome in methanol poisonings is primarily associated with the late diagnosis and delayed initiation of treatment with antidote, be it fomepizole or ethanol [22–24]. Severity of metabolic acidosis on admission is known prognostic parameter of poor outcome (death or long-term visual and/or central nervous system sequelae) in acute methanol poisoning [25–28]. Timely correction of acidemia and the elimination of formic acid by hemodialysis are one of the crucial issues for successful treatment [29–33].
In our study, the EtOH-positive patients were less acidotic on admission to hospitals with significantly higher arterial blood pH and bicarbonate, and lower lactate, base deficit, and anion gap, with no difference in time to presentation or serum methanol on admission as compared with the EtOH-negative patients. This indicates an effective blocking of the ADH enzyme in the pre-treated patients. The pre-hospital ethanol group was still able to hyperventilate adequately in spite of the ethanol treatment indicating that a modest administration of ethanol itself does not alter the patients’ ability to hyperventilate, and thus not removing this important compensatory mechanism [34, 35].
There were significantly more asymptomatic patients on admission to hospitals in the EtOH-positive group. In Group I (survivors without sequelae), there were also fewer patients with dyspnea and symptoms of visual toxicity at presentation among the EtOH-positive patients comparing the EtOH-negative patients. Only one patient administered pre-hospital ethanol with GCS 10 fell into a coma on admission to the hospital; this patient had severe acidemia on admission to hospital with high serum lactate and low methanol, suggesting that most of it had already been metabolized to toxic formic acid. In other patients who received pre-hospital ethanol administration, no deterioration of the state-of-consciousness was registered after admission.
The significant association was found between the outcome of treatment and both serum ethanol concentration on admission and pre-hospital ethanol administration by paramedics/medical staff in our study. The positive association remained strong after the elimination of patients with GCS ≤10 on the first presentation. Logistic regression analysis demonstrated that serum ethanol concentration on admission was significant variable for the treatment outcome when adjusted for the degree of acidemia and the state-of-consciousness on admission.
The probability of poor outcome (death or sequelae) decreased exponentially with increasing arterial blood pH, but the rate of decrease was higher in the patients with pre-hospital ethanol administration. Finally, the probability of survival with visual and/or CNS sequelae depended on the serum ethanol concentration.
In summary, the present data document the significant association between positive serum ethanol concentration on admission to hospital and better treatment outcome in acute methanol poisoning. This fact supports the recommendation on the potential benefit of the pre-hospital administration of ethanol on outcome during an on-going outbreak of methanol poisoning [21]: given a standard regimen, a worst-case scenario would mean that a certain number of patients will be given a limited amount of ethanol unnecessarily, which can be considered acceptable from a risk–benefit point of view.
Strength and limitations
The limitations of this study can be attributed to certain confounders, as it was not a randomized controlled trial, leaving the possibility of inherent bias during the comparisons. The numbers of the patients in both groups were relatively small (even if by far the largest of its kind), and most of the patients in both groups were the so-called “late-presenters”. Despite the limitations and confounders, the study provides important data on the effect of positive serum ethanol concentration on admission to hospital on the outcome of treatment during a large methanol outbreak. The essential clinical and laboratory data on admission were collected during admission to hospital using standardized forms. The groups of patients were also comparable by age, circumstances of poisoning, latency period, and size.
Conclusion
In our study, positive serum ethanol concentration on admission to hospital was associated with survival and better treatment outcome of poisoned patients during the Czech mass methanol outbreak. Our data, therefore, strongly support a recommendation that ethanol can be administered pre-hospital by paramedics/medical staff to conscious patients suspected to be poisoned with methanol before laboratory data are available and diagnosis confirmed.
Experimental
Patients
Among 137 cases of methanol poisoning in the Czech Republic from the 3 September 2012 until the 31 August 2014, 106 patients were treated in hospitals. The discharge reports of all hospitalized patients with a confirmed diagnosis and the results of neurological and ophthalmological examinations on admission, during hospitalization, and on discharge were collected and analyzed in the TIC. A detailed history of the poisoning, and of the onset and dynamics of ocular and systemic toxicity, was obtained in a prospective manner directly from the patients or from relatives of critically ill patients upon admission to the secondary hospital.
Laboratory analyses were performed on admission. Diagnosis was established when (1) a history of recent ingestion of illicit spirits was available and serum methanol was higher than 6.2 mmol dm−3 and/or an osmolal gap (OG) ≥20 mOsm (kg H2O)−1 was found, or (2) there was a history/clinical suspicion of methanol poisoning, and serum methanol was above the limit of detection with at least two of the following: pH < 7.3, serum bicarbonate <20 mmol dm−3, and anion gap (AG) ≥20 mmol dm−3 [36, 37].
The clinical examination protocol included complete ocular examination with the standard ophthalmologic tests (visual acuity, color vision, contrast sensitivity, perimeter, and fundus), cerebral computed tomography (CT) or magnetic resonance imaging (MRI) of the brain, and standard neurological examination. The patients were considered to have visual sequelae of acute methanol poisoning if the symptoms of toxic neuropathy of the optic nerve were documented on admission/during hospitalization, with pathologic findings on visual acuity, visual fields, color vision, contrast sensitivity, and persisting lesions on fundoscopy with other symptoms of visual damage being found on discharge from the hospitals. The patients were considered as having CNS sequelae of poisoning if symmetrical necrosis and hemorrhages of basal ganglia were present on CT or MRI of the brain.
The hospitalized patients were retrospectively divided into three groups according to their outcome: Group I: Patients who survived without sequelae; Group II: patients who survived with visual and/or CNS sequelae; and Group III: patients who died. These groups were then further divided into two subgroups ‘with pre-hospital ethanol administration by paramedics/medical staff (EtOH-positive)’ and ‘without pre-hospital ethanol administration by paramedics/medical staff (EtOH-negative)’. Within the latter subgroup, the data from patients who self-administered ethanol shortly before presentation to hospitals were analyzed separately.
Treatment
All patients were treated in accordance to the American Association of Clinical Toxicology and the European Association of Poison Centres and Clinical Toxicologists (AACT/EAPCCT) practice guidelines on the treatment of methanol poisoning [14]. Bicarbonate 8.4 or 4.2 % solution was given intravenously as a buffer to the patients with metabolic acidosis. Fomepizole or ethanol were administered as antidotes to block ADH enzyme. Folates were administered to substitute the endogenous pool.
Enhanced elimination was performed if the patients met any of the following criteria: serum methanol higher than 15.6 mmol dm−3, metabolic acidosis with arterial blood pH < 7.30, or had the signs of visual toxicity. The choice of modality of enhanced elimination was based on several factors, such as the hemodynamic stability of a patient on admission, or the severity of poisoning, and availability of dialysis equipment.
Laboratory investigations
Methanol was measured by a gas chromatographic method with flame ionization detection and a direct injection with an internal standard, limit of detection 1.9 mmol dm−3, and day-to-day coefficient of variation 2.5–5.4 %. Formate was measured enzymatically using formate dehydrogenase and nicotinamide adenine dinucleotide, according to a previously published method [38, 39]. Day-to-day coefficient of variation was 5.6 %, and the upper reference limit was 0.44 mmol dm−3. Serum ethanol was analyzed by gas chromatography with flame ionization detection and direct injection with an internal standard. The limit of detection was 0.87 mmol dm−3, and the day-to-day coefficient of variation was 3.8–7.1 %. Osmolality was measured by the freezing point depression method on a Fiske one-ten osmometer. The reference range for the osmolal gap was −9 to 19 mOsm (kg H2O)−1 [40]. The osmolal contribution from ethanol was subtracted from the measured osmolality.
Statistical analyses
The laboratory and clinical data were compared using two-sample assuming unequal variances, two-sample F test for variances, bias test, and two-sample Kolmogorov–Smirnov test. The data were expressed as medians with interquartile ranges (IQR). Spearman’s rank correlation, exploratory factor analysis, and Chi-square tests were used to analyze the association between different variables and the outcomes of treatment. Statistically significant parameters were subsequently used in the regression models of ordinal multinomic logistic regression based on likelihood ratio estimation. Probabilistic analysis of predictive ability of significant parameters for the poor outcome of treatment was applied using Hosmer–Lemeshow likelihood ratio R 2. All statistical calculations were carried out on the level of significance α = 0.05.
Ethics
The study was approved by the General University Hospital Ethics Committee in Prague, Czech Republic.
References
Hovda KE, Hunderi OH, Tafjord AB, Dunlop O, Rudberg N, Jacobsen D (2005) J Intern Med 258:181
Paasma R, Hovda KE, Tikkerberi A, Jacobsen D (2007) Clin Toxicol 45:152
Hassanian-Moghaddam H, Nikfarjam A, Mirafzal A, Saberinia A, Nasehi AA, Asl HM, Memaryan N (2015) J Public Health 37:354
Rostrup M, Edwards JK, Abukalish M, Ezzabi M, Some D, Ritter H, Menge T, Abdelrahman A, Rootwelt R, Janssens B, Lind K, Paasma R, Hovda KE (2016) Plos One 11:e0152676
Zakharov S, Navratil T, Pelclova D (2013) Basic Clin Pharmacol Toxicol 112:425
Zakharov S, Navratil T, Pelclova D (2013) Psychiatry Res 210:302
Zakharov S, Csomor J, Urbanek P, Pelclova D (2016) Basic Clin Pharmacol Toxicol 118:87
Liesivuori J, Savolainen H (1991) Pharmacol Toxicol 69:157
Jacobsen D, McMartin KE (1986) Med Toxicol 1:309
Zakharov S, Navratil T, Pelclova D (2015) Monatsh Chem 146:787
Zakharov S, Nurieva O, Kotikova K, Urban P, Navratil T, Pelclova D (2016) Monatsh Chem 147:251
Nurieva O, Kotikova K, Urban P, Pelclova D, Petrik V, Navratil T, Zakharov S (2016) Monatsh Chem 147:239
Zakharov S, Kotikova K, Vaneckova M, Seidl Z, Nurieva O, Navratil T, Caganova B, Pelclova D (2016) Basic Clin Pharmacol Toxicol 119:228
Barceloux DG, Bond GR, Krenzelok EP, Cooper H, Vale JA (2002) J Toxicol-Clin Toxicol 40:415
Jacobsen D, Jansen H, Wiik-Larsen E, Bredesen JE, Halvorsen S (1982) Acta Med Scand 212:5
Hantson P, Wittebole X, Haufroid V (2002) Eur J Emerg Med 9:278
Bergeron R, Cardinal J, Geadah D (1982) N Engl J Med 307:1528
Kraut JA (2016) Am J Kidney Dis 68:161
Kraut JA, Kurtz I (2008) Clin J Am Soc Nephrol 3:208
Zakharov S, Pelclova D, Urban P, Navratil T, Diblik P, Kuthan P, Hubacek JA, Miovsky M, Klempir J, Vaneckova M, Seidl Z, Pilin A, Fenclova Z, Petrik V, Kotikova K, Nurieva O, Ridzon P, Hovda KE (2014) Clin Toxicol 52:1013
Zakharov S, Pelclova D, Urban P, Navratil T, Nurieva O, Kotikova K, Diblik P, Kurcova I, Belacek J, Komarc M, Eddleston M, Hovda KE (2016) Ann Emerg Med 68:52
Megarbane B (2010) Open Access Emergency Medicine 2
Zakharov S, Navratil T, Pelclova D (2014) Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 158:641
Zakharov S, Pelclova D, Navratil T, Belacek J, Komarc M, Edleston M, Hovda KE (2015) Clin Toxicol 53:797
Paasma R, Hovda KE, Hassanian-Moghaddam H, Brahmi N, Afshari R, Sandvik L, Jacobsen D (2012) Clin Toxicol 50:823
Bezdicek O, Klempir J, Liskova I, Michalec J, Vaneckova M, Seidl Z, Janikova B, Miovsky M, Hubacek JA, Diblik P, Kuthan P, Pilin A, Kurcova I, Fenclova Z, Petrik V, Navratil T, Pelclova D, Ruzicka E, Zakharov S (2014) Cesk Slov Neurol N 77/110:320
Zakharov S, Pelclova D, Diblik P, Urban P, Kuthan P, Nurieva O, Kotikova K, Navratil T, Komarc M, Belacek J, Seidl Z, Vaneckova M, Hubacek JA, Bezdicek O, Klempir J, Yurchenko M, Ruzicka E, Miovsky M, Janikova B, Hovda KE (2015) Clin Toxicol 53:884
Hubacek JA, Pelclova D, Seidl Z, Vaneckova M, Klempir J, Ruzicka E, Ridzon P, Urban P, Fenclova Z, Petrik V, Diblik P, Kuthan P, Miovsky M, Janikova B, Adamkova V, Zakharov S (2014) Basic Clin Pharmacol Toxicol 116:168
Zakharov S, Pelclova D, Navratil T, Belacek J, Kurcova I, Komzak O, Salek T, Latta J, Turek R, Bocek R, Kucera C, Hubacek JA, Fenclova Z, Petrik V, Cermak M, Hovda KE (2014) Kidney Int 86:199
Vaneckova M, Zakharov S, Klempir J, Ruzicka E, Bezdicek O, Brozova H, Diblik P, Miovsky M, Hubacek JA, Urban P, Ridzon P, Pelclova D, Burgetova A, Masek M, Kotikova K, Peterova K, Liskova I, Hamplova L, Seidl Z (2015) Neuroendocrinol Lett 36:737
Zakharov S, Nurieva O, Navratil T, Diblik P, Kuthan P, Pelclova D (2014) J Appl Biomed 12:309
Vaněčková M, Zakharov S, Klempíř J, Růžička E, Bezdíček O, Lišková I, Diblík P, Miovský M, Hubáček JA, Urban P, Ridzoň P, Pelclová D, Burgetová A, Mašek M, Seidl Z (2014) Cesk Slov Neurol 77/110:235
Urban P, Zakharov S, Diblík P, Pelclová D, Ridzoň P (2016) Int J Occup Med Environ Health 29:471
McMartin K, Jacobsen D, Hovda KE (2016) Br J Clin Pharmacol 81:505
Zakharov S, Navratil T, Salek T, Kurcova I, Pelclova D (2015) Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 159:666
Brent J, McMartin K, Phillips S, Aaron C, Kulig K (2001) N Engl J Med 344:424
Hovda KE, Urdal P, Jacobsen D (2005) J Anal Toxicol 29:586
Zakharov S, Kurcova I, Navratil T, Salek T, Komarc M, Pelclova D (2015) Basic Clin Pharmacol Toxicol 116:445
Schaller KH, Triebig GT (1984) Formate determination with formate dehydrogenase. In: Bergmeyer HU (ed) Methods of enzymatic analysis. Verlag Chemie, Weinheim, p 668
Aabakken L, Johansen KS, Rydningen EB, Bredesen JE, Ovrebo S, Jacobsen D (1994) Hum Exp Toxicol 13:131
Acknowledgments
Supported by the Ministry of Health of the Czech Republic (AZV), Grant No. 16-27075A, Charles University in Prague projects P25/1LF/2, P28/1LF/6, the Project of the Ministry of Health of the Czech Republic 43/16/RPZP, and by J. Heyrovský Institute of Physical Chemistry of the AS CR, v.v.i.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s00706-017-1921-0.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made.
The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
To view a copy of this licence, visit https://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zakharov, S., Nurieva, O., Kotikova, K. et al. Positive serum ethanol concentration on admission to hospital as the factor predictive of treatment outcome in acute methanol poisoning. Monatsh Chem 148, 409–419 (2017). https://doi.org/10.1007/s00706-016-1846-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00706-016-1846-z