Abstract
Tics are rapid, recurrent, non-rhythmic movements or emitted sounds. Tics are the hallmark of Tourette syndrome (TS); however, a number of other disorders may be associated with tics, so-called secondary tic disorders (STD). We assessed clinical history and performed blinded evaluations of video-recordings from patients with TS and STD in order to identify features that may differentiate tics associated with TS vs STD. There were 156 patients with TS and 38 with STD, 21 of whom had functional (psychogenic) tics. Patients with TS were more frequently male and had a younger age at onset. Tics in TS tend to involve muscles in the cranial-cervical area more often and have greater severity and complexity than those in patients with STD. Similar findings were observed when contrasting patients with TS with patients with functional tics only. Simple phonic tics showed the greatest diagnostic accuracy for TS, compared with STD, but marked overlap in the types of tics and comorbidities was observed between patients with TS and STD. Patients with TS were more likely males, had a younger age at onset, phonic tics and motor tics affecting predominantly the head and neck area, and had a greater complexity and severity of tics than those with STD. When these features are absent a consideration should be given to the possibility of a tic disorder other than TS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tics are sudden, rapid, recurrent, non-rhythmic purposeless movements or emitted sounds. Tourette syndrome (TS), a childhood onset neuro-behavioral disorder, is the most common diagnosis in patients with motor and phonic tics (Johnson et al. 2022). However, some patients may present with a tic disorder that does not fulfill the diagnostic criteria for TS or have a clear temporal relationship with a traumatic brain injury, drug exposure, encephalitis, or an autoimmune or a degenerative disorder, so called secondary tic disorders (STD) (Johnson et al. 2022). An increasingly recognized observation is that a large proportion of patients with tics have a functional (previously known as psychogenic) etiology (Baizabal-Carvallo and Jankovic 2014). This became especially relevant during the COVID-19 pandemic (Hull et al. 2021; Pringsheim et al. 2021). Patients with STD are categorized in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), as “Other Specified Tic Disorders” (American Psychiatric Association 2013). Similar to TS-related tics, STD cause distress or impairment in social, educational/occupational or other vital area functioning, according to the DSM-5 criteria.
Patients with TS have been studied in large cohorts, they have a mean age at onset of 6.4 years, with a clear male predominance over females: 3–4:1 (Freeman et al. 2000). Patients with TS develop simple and complex motor and phonic tics in a rostro-caudal sequence, usually preceded by a premonitory sensation from which awareness increases with age (Kwak et al. 2003). About 90% of TS patients report an associated neuropsychiatric comorbidity, mostly attention-deficit/hyperactivity disorder (ADHD) in 60% of cases and obsessive–compulsive disorder (OCD) in a quarter of cases (Freeman et al. 2000). On the other hand, patients with STD are usually described in single case reports or small case series without direct comparison with TS-related tics. An older age at onset (after 18 year of age), lack of family history of tics, absence of premonitory sensations, lack of the typical neuropsychiatric comorbidities observed in TS and temporal or comorbid association with a brain insult or another neurological disorder suggests a STD. In this study, we aimed to contrast the clinical features of tics in the setting of TS vs STD in order to gain insights into clinical phenomenology and diagnostic clues between both groups of disorders.
Materials and methods
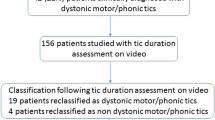
Video-recordings of consecutive patients with tics were assessed during a 3-year period at the Parkinson’s Disease Center and Movement Disorders Clinic, Baylor College of Medicine, Houston, Texas. The video rater was blinded to the etiologic diagnosis in the subjects. The evaluator was a movement disorders specialist with expertise in TS. All patients were recorded from 10 to 15 min to capture their tics. We then reviewed medical records and classified the patients as TS or STD according to the DSM-5 (American Psychiatric Association 2013). The diagnosis of STD was also supported by a clear temporal association with the offending event or a clear pathophysiological association with another disorder, for example tics in the context of Sydenham’s chorea or Huntington’s disease. A functional etiology was diagnosed according to the Fahn and Williams criteria, which require, in addition to other features such as sudden onset and distractibility, that the observed movements are incongruent or inconsistent with typical organic movement disorders (Fahn and Williams 1998). Depending on the presence of the various clinical features patients were assigned to one of four categories of increasing diagnostic certainty: possible, probable, clinically established and documented. Accordingly, patients with functional tics were diagnosed with a clinically established functional neurological disorder. After reviewing clinical history and video-recordings, we eliminated 14 patients, due to uncertainty about comorbid TS (n = 6), no tics were observed on video-recordings (n = 6), or patients had another movement disorder, rather than tics (n = 2).
We assessed the type of tics (motor or phonic), their phenomenology (simple or complex), and distribution of tics (Johnson et al. 2022). The latter was performed with a semi-quantitative scale, assigning 1 point to each affected body part (face, neck, phonic, arms, trunk/abdomen and legs) with a score range of 1–6 points, after adding the points from every body part where tics were observed in the recordings or reported by the patient. The severity of tics was rated based on review of video-recordings and classified into six categories, analogous to other studies, based on the Global Severity Rating and Rush Video-Based Tic Rating Scales as previously described (Goetz et al. 1999). The following categories were included: 0: None; 1: very mild (tics rarely observed on video); 2: mild (tics are noticeable but not disruptive); 3: medium (tics are frequent but mildly disruptive); 4: marked (tics are severe and disruptive); 5: severe (tics are very severe and disruptive); 6: very severe (tics are extremely disruptive). Comorbid (ADHD) and obsessive–compulsive disorder (OCD) were diagnosed based on review of the medical records according to the DSM-5 criteria (American Psychiatric Association 2013). We evaluated the diagnostic performance of variables showing statistically significance between groups.
Patients or a close family member provided written informed consent for videotaping and publishing in a scientific journal approved by the Baylor College of Medicine Institutional Review Board for Human Research and Sante Research Board.
Statistics
We summarized data in percentages, means and standard deviations. The chi-square (χ2) and the Fisher’s exact tests were performed to compare proportions between groups. Odds ratios (OR) and confidence intervals (CI) at 95% were used to assess risk for variables of interest. The t test for independent samples test was used to compare means between groups. We calculated sensitivity and specificity for variables showing statistically significance difference between patients with TS and STD. The Youden’s J statistics (J = sensitivity + specificity − 1) was used to assess the performance of a diagnostic variable. All statistic evaluations were carried out by means of SPSS version 22; a P value < 0.05 was considered significant.
Results
TS vs non-TS
There were 156 patients with TS and 38 patients with STD. Presumed etiologies of tics in the STD group are presented in Table 1. Patients with TS were more commonly male (78.2 vs. 57.8%, P = 0.010) and significantly younger at age of onset and evaluation (P < 0.001). Patients with TS showed a broader body distribution of tics compared with STD patients with more affected body parts for the former group (P = 0.003).
A caudocephalic anatomic distribution gradient was observed in patients with both TS and STD. However, some cranial tics were statistically significantly more common in patients with TS, such as excessive eye-blinking, eye-rolling tics, jaw tics; head jerks were also more common in patients with TS (Table 2). Patients with TS showed greater overall severity of tics and a significantly higher frequency of simple phonic tics and complex motor and phonic tics (Table 2). Patients with TS also had a greater frequency of comorbid ADHD and OCD.
TS vs. functional tics
Most patients with STD (n = 21, 55.26%) were diagnosed with a functional tic. Premonitory sensation was reported in 4 (19%) patients with functional tics and 1 patient with post-stroke tics. When TS was compared with functional tics only, patients with TS were more frequently males (P = 0.010), had a younger age at onset and evaluation (P < 0.001), had a greater frequency of facial tics (P = 0.018), including eye-blinking (P = 0.002) and jaw tics (P = 0.004); however, facial grimacing and eye-rolling did not show statistically significant differences. Although patients with TS had a greater number of affected body parts, no differences in severity was observed (P = 0.096). Complex motor and simple phonic tics were more common in patients with TS (P < 0.001, for both variables); but complex phonic tics were equally observed between groups. Comorbid ADHD and OCD were statistically more common in patients with TS (P = 0.010 and 0.003, respectively) (Table 2).
Diagnostic performance
After testing sensitivity, specificity and diagnostic performance (J value) of contrasting features between TS and STD or functional tics; simple phonic tics showed the highest diagnostic accuracy to differentiate between TS and STD or TS and functional tics (J = 0.62 and 0.61, respectively). Complex tics had the highest sensitivity for the diagnosis of TS (0.95); whereas oromandibular tics had the greatest specificity (0.97) for the diagnosis of TS when compared with STD (Table 3).
Discussion
In this study, we found that patients with TS have a distinct motor/phonic tic syndrome compared with patients with STD. Patients with TS were more frequently male and had a younger age at onset. Furthermore, tics in TS tend to involve muscles in the cranial-cervical area more frequently and have greater severity and complexity of their tics than those observed in patients with STD. Indeed, some tics such as eye-blinking, jaw tics and head jerks were markedly more common in patients with TS as compared to those with STD. Eye tics have been deemed as a core feature of TS and seem to support this diagnosis in patients with tics (Martino et al. 2012; Baizabal-Carvallo and Jankovic 2022). Despite these differences, there does not seem to be a single feature that has an absolute accuracy to discriminate between patients with TS and STD. We tested the diagnostic accuracy of individual clinical features for the diagnosis of TS. Simple phonic tics had the greatest diagnostic accuracy for TS. However, oromandibular tics showed a high specificity for TS diagnosis, when compared with all STD or functional tics only (Fig. 1). Oromandibular tics have shown to be markers of greater TS severity (Baizabal-Carvallo et al. 2023). These findings should tested in further studies.
Although tics may be observed in a number of other disorders besides TS, it is likely that the underlying pathophysiology varies among etiologies. Experimental studies in animals have shown that, disinhibition of the cortico-striato-thalamo-cortical circuits as a result of GABAergic deficiency leads to tic-like movements (Pogorelov et al. 2015). Furthermore, various imaging and neurophysiologic studies have suggested that the dorsal anterior insula may be part of the urge-tic network and could influence the urge- and tic-related cortico-striato-thalamic regions in TS (Jackson et al. 2020). Disturbance of cortical-basal ganglia-cerebellar networks probably underlies the pathophysiology of tics irrespective of underlying etiology.
Several clinical and pathophysiological differences have been proposed between patients with TS and functional tics. From a biochemical standpoint, patients with TS have evidence of increased dopaminergic activity in basal ganglia as dopamine receptor blockers consistently improve motor and phonic tics (Maia and Conceição 2018); moreover, pathological and neuroimaging evidence of impairment in the inhibitory neuro-transmitter GABA provides a biochemical basis for decreased inhibition in patients with TS (Lerner et al. 2012). However, a consistent abnormality in neurotransmitters has not been identified in patients with functional movement disorders, including functional tics, and these patients do not show improvement with pharmacological manipulation of inhibitory or excitatory neurotransmitters (Baizabal-Carvallo et al. 2019).
Our study has some limitations. For example, patients with STD may have fragments of other movements (i.e. chorea) besides tics and most have functional tics (Baizabal-Carvallo 2021). Our study did not include the so called “TikTok tics”, a form of functional neurological disorder that characterizes by rapid-onset of exaggerated tic-like behaviors that follows exposure to a social media personality (Hull and Parnes 2021). We are not aware of this kind of exposure in our patients. An analysis of most viewed videos from that social network showed several atypical features such as unusually frequent coprolalia, strong environmental influence, aggression, object throwing, self-injurious behavior and uttering long phrases (Zea Vera et al. 2022). Moreover, when compared with patients with TS, these individuals showed a greater severity on tic-scale (Pringsheim et al. 2021). In our study, we compared TS patients with patients with non-TikTok functional tics. Another limitation is that we did not assess systematically premonitory sensations. This premonitory sensory phenomenon has been consistently reported in over 90% of patients with TS (Kwak et al. 2003) and were reported only in 19% of patients with functional tics and in only 13.15% in patients with STD in our study, pointing to diverse mechanisms underlying tics between groups.
Conclusions
In summary, patients with TS are more likely males, have a wider anatomic distribution of tics, and greater severity and complexity of tics than those with STD. Despite some overlap in clinical features, the two forms of tics can be differentiated not only etiologically but also phenomenologically.
Availability of data and material
Available under reason request.
Code availability
Not applicable.
References
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. Author, Arlington, VA
Baizabal-Carvallo JF, Jankovic J (2014) The clinical features of psychogenic movement disorders resembling tics. J Neurol Neurosurg Psychiatry 85:573–575
Baizabal-Carvallo JF, Jankovic J (2021) Beyond tics: movement disorders in patients with Tourette syndrome. J Neural Transm (vienna) 128:1177–1183
Baizabal-Carvallo JF, Jankovic J (2022) The clinical phenomenology and correlations of oculogyric tics. Acta Neurol Belg 122:925–930
Baizabal-Carvallo JF, Hallett M, Jankovic J (2019) Pathogenesis and pathophysiology of functional (psychogenic) movement disorders. Neurobiol Dis 127:32–44
Baizabal-Carvallo JF, Alonso-Juarez M, Jankovic J (2023) Oromandibular tics associated with Tourette syndrome. J Neurol. https://doi.org/10.1007/s00415-023-11583-8
Fahn S, Williams DT (1998) Psychogenic dystonia. Adv Neurol 50:431–455
Freeman RD, Fast DK, Burd L, Kerbeshian J, Robertson MM, Sandor P (2000) An international perspective on Tourette syndrome: selected findings from 3,500 individuals in 22 countries. Dev Med Child Neurol 42:436–447
Goetz CG, Pappert EJ, Louis ED, Raman R, Leurgans S (1999) Advantages of a modified scoring method for the rush video-based tic rating scale. Mov Disord 14:502–506
Hull M, Parnes M (2021) Tics and TikTok: functional tics spread through social media. Mov Disord Clin Pract 8:1248–1252
Hull M, Parnes M, Jankovic J (2021) Increased incidence of functional (psychogenic) movement disorders in children and adults amid the COVID-19 pandemic: a cross-sectional study. Neurol Clin Pract 11:e686–e690
Jackson SR, Loayza J, Crighton M, Sigurdsson HP, Dyke K, Jackson GM (2020) The role of the insula in the generation of motor tics and the experience of the premonitory urge-to-tic in Tourette syndrome. Cortex 126:119–133
Johnson KA, Worbe Y, Foote KD, Butson CR, Gunduz A, Okun MS (2022) Tourette syndrome: clinical features, pathophysiology, and treatment. Lancet Neurol S1474–4422(22):00303–00309
Kwak C, Dat Vuong K, Jankovic J (2003) Premonitory sensory phenomenon in Tourette’s syndrome. Mov Disord 18:1530–1533
Lerner A, Bagic A, Simmons JM et al (2012) Widespread abnormality of the γ-aminobutyric acid-ergic system in Tourette syndrome. Brain 135:1926–1936
Maia TV, Conceição VA (2018) Dopaminergic disturbances in Tourette Syndrome: an integrative account. Biol Psychiatry 84:332–344
Martino D, Cavanna AE, Robertson MM, Orth M (2012) Prevalence and phenomenology of eye tics in Gilles de la Tourette syndrome. J Neurol 259:2137–2140
Pogorelov V, Xu M, Smith HR, Buchanan GF, Pittenger C (2015) Corticostriatal interactions in the generation of tic-like behaviors after local striatal disinhibition. Exp Neurol 265:122–128
Pringsheim T, Ganos C, McGuire JF, Hedderly T, Woods D, Gilbert DL, Piacentini J, Dale RC, Martino D (2021) Rapid onset functional tic-like behaviors in young females during the COVID-19 pandemic. Mov Disord 36:2707–2713
Zea Vera A, Bruce A, Garris J, Tochen L, Bhatia P, Lehman RK, Lopez W, Wu SW, Gilbert DL (2022) The phenomenology of tics and tic-Like behavior in TikTok. Pediatr Neurol 130:14–20
Funding
None.
Author information
Authors and Affiliations
Contributions
JFB-C: gather and analysis of data, made the statistical analysis, conceptualized, wrote the first draft, and reviewed the manuscript; MA-J: gathered and analyzed data; JJ: gathered the data, conceptualized and reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None for all authors.
Ethics approval
The Baylor College of Medicine Internal Review Board provided consent for case publications after written approval by patients or family members.
Consent to participate
Patients provided written informed consent to participate in scientific research.
Consent for publication
Patients provided written informed consent for publication in a scientific journal.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baizabal-Carvallo, J.F., Alonso-Juarez, M. & Jankovic, J. Contrasting features between Tourette syndrome and secondary tic disorders. J Neural Transm 130, 931–936 (2023). https://doi.org/10.1007/s00702-023-02642-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-023-02642-5