Abstract
Pump-guided intrajejunal levodopa administration is one of the indispensable forms of therapy in advanced Parkinson's syndrome, along with deep brain stimulation and subcutaneous apomorphine injection. The standard application of levodopa gel via a JET-PEG, i.e. a percutaneous endoscopic gastrostomy (PEG) with an inserted internal catheter into the jejunum, has not been unproblematic due to the restricted absorption area of the drug in the region of the flexura duodenojejunalis and especially due to the sometimes considerable accumulated complication rates of a JET-PEG. Causes of complications are mainly a non-optimal application technique of PEG and internal catheter as well as the often missing adequate follow-up care. This article presents the details of a—compared to the conventional technique—modified and optimised application technique, which has been clinically proven successfully for years. However, many details derived from anatomical, physiological, surgical and endoscopic aspects must be strictly observed during the application to reduce or avoid minor and major complications. Local infections and buried bumper syndrome cause particular problems. The relatively frequent dislocations of the internal catheter (which can ultimately be avoided by clip-fixing the catheter tip) also prove to be particularly troublesome. Finally, using the Hybrid technique, a new combination of an endoscopically controlled gastropexy with 3 sutures and subsequent central thread pull-through (TPT) of the PEG tube, the complication rate can be dramatically reduced and thus a decisive improvement achieved for patients. The aspects discussed here are highly relevant for all those involved in the therapy of advanced Parkinson's syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Levodopa is still the most important drug therapy for Parkinson's syndrome. However, experience shows that levodopa has to be administered more and more frequently during the course of the disease and that end-of-dose dyskinesias (hypo- and hyperkinesias) occur despite precisely timed oral dosing, forcing the use of alternative therapies (Salat and Tolosa 2013).
For such advanced stages of the disease, deep brain stimulation (DBS), subcutaneous apomorphine application by pump or intrajejunal levodopa application by pump are possible options (AWMF 2016).
The background for this therapeutically difficult situation is, in addition to the loss of dopaminergic neurons and the decrease in dopamine storage capacity (Jost et al. 2022), on the one hand the very short half-life/duration of action of levodopa and, on the other hand, the early involvement of the gastrointestinal tract in the symptoms of idiopathic Parkinson's syndrome (iPS) in the sense of a transit disorder. With subtle diagnostics, intestinal motility disorders are often detectable very early in the course of the disease (Jost 2010). In addition to swallowing and transport problems in the oesophagus, gastroparesis, i.e. impaired motility of the stomach with slowed, uncoordinated or absent gastric emptying, is decisive, especially in advanced iPS (Warnecke et al. 2022). In the further course, this leads to a difficult, hardly or unpredictable transport of the drug into the duodenum or jejunum. Often the tablets get stuck in the oesophagus or do not reach their site of action in the proximal jejunum. This has correspondingly profound consequences for levodopa plasma levels in terms of fluctuations and pronounced ON/OFF problems.
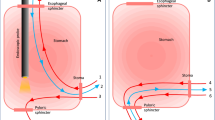
Another fundamental problem of oral levodopa medication is the absorption of the active substance almost exclusively in the proximal jejunum. The local accuracy of the application (= topographical precision) is complicated by a restricted absorption area (10–20 cm) immediately after the flexura duodeno-jejunalis (see schematic drawing Fig. 1). Overview in (Warnecke et al. 2022).
Possibilities of drug application into the proximal jejunum (red marking: access site). A Anatomical situation: restricted absorption area for levodopa: only in the first centimetres of the jejunum at the flexura duodenojejunalis. B transnasal (nasoenteric) tube, tip in target area. C JET-PEG: internal catheter through a PEG placed in the stomach, catheter tip in the target area. D EPJ = D-PEJ, direct puncture and probe insertion into the small intestine, inner retaining plate in the target area
This topographical factor—in addition to gastroparesis—makes oral therapy difficult to control and complicates gastral/jejunal administration of levodopa by tube.
Clinical experience shows that the problem awareness of the effects of gastroparesis and the limited absorption area should be deepened among neurological and gastroenterological colleagues.
In principle, the administration of drugs into the intestine is possible through a nasoenteric tube (NES) or through various percutaneous endoscopic gastrostomy (PEG) procedures (Fig. 1).
For the intrajejunal levodopa application discussed here—which is considered one of the three standard therapies for advanced Parkinson's syndrome—temporary (e.g. for testing levodopa administration), a nasoenteric tube can be inserted, but usually a PEG with an internal catheter, a so-called JET-PEG, is inserted for permanent therapy (Dam-Larsen et al. 2015; Lex et al. 2018; Gheorghe et al. 2019).
In principle, any PEG placement can be associated with complications (Grund and Zipfel 2016), which is why, on the one hand, acceptance is limited for some patients, and, on the other hand, high burdens arise for the patient and the healthcare system in the event of a complication. Interestingly, in recent LCIG studies, complications from the JET-PEG itself, tube and pump have been demonstrated in 60–100% of patients (Fernandez and Vanagunas 2013; Jost 2014; Nyholm and Stepien 2014).
In the relatively complex invasive procedure of a JET-PEG, problems should be avoided as far as possible from the outset to prevent complications by ensuring that all players have carefully and comprehensively undergone a hands-on training on the correct method in advance (Grund and Zipfel 2019).
The aim of this paper is to address the hitherto under-publicised problems of the conventional technique and to present and discuss the resulting alternatives.
The route of application via a JET-PEG, i.e. an internal catheter extending to the duodenal/jejunal region through a present PEG, which has so far been accepted as a given by the neurological side, must be discussed anew and critically from a surgical and endoscopic point of view—even now that there is an application procedure in the form of the Hybrid-PEG, which apparently involves considerably fewer complications than the conventional PEG techniques.
Methods
Conventional delivery techniques as presented in the literature and in guidelines (Loser et al. 2005) have changed little in the 40 years since the inauguration of the method and have various weaknesses that have been shown to be the cause of the very high complication rates of PEG. In the literature, complication rates are usually only reported in a differentiated manner (Hucl and Spicak 2016; Boeykens and Duysburgh 2021), but in cumulation they are 40–75% (Rabast et al. 2008; Kratt et al. 2010; Schwartz and Ziegler 2022). These facts have led to the development of alternative techniques (Grund et al. 2006a; Grund and Zipfel 2016; Grund et al. 2021), which are based on (patho-) anatomical and (patho-) physiological facts as well as surgical considerations. With strict attention to the details described, this has led to a dramatic reduction in complication rates (cumulative complication rate dropped from 46 to 13%, early complications from 23 to 3%, late complications from 22 to 10% (Grund pers. comm. 2006)).
Results/critical presentation of the conventional technique
As a result of the research in literature and guidelines as well as numerous hospitalizations and more than 100 PEG courses with several 1000 participants, it is clear that the conventional technique carries numerous possible sources of problems, which are presented here first:
Transnasal tubes (TNT)
In the case of transnasal tube, frequent problems include relatively untargeted, inconsistently controlled tube insertion using the OTW/BTS technique, no targeted local anaesthesia but merely the application of anaesthetic lubricant to the tube, as well as incorrect ante- or reclination of the head during tube insertion. In principle, tube application beyond the flexura duodenojejunalis is also often difficult if the corresponding technical requirements are not respected (Grund and Ingenpaß 2007; Grund and Zipfel 2016).
PEG in thread pull-through technique (TPT)
Complications during the insertion of a PEG in thread pull-through technique (TPT) are more frequent if the insertion is not prepared in a standardised manner (e.g. standardised instrument table), if diaphany and local anaesthesia are performed relatively untargeted and unsystematically in an aspiration technique, if the anaesthetic needle is not fixed in the gastric lumen, and if the insertion of the scalpel and thread trocar is performed without a support technique and without internal fixation.
Grasping the thread is often difficult in the gastric secretions, and there is a risk of losing the thread when it is pulled out of the mouth.
If the traction force is not well controlled when pulling the thread with the PEG tube through the abdominal wall, there is on the one hand the danger of injury to the base of the tongue by the thread and on the other hand the development of a pneumoperitoneum is programmed.
Serious complications are mainly triggered by the fact that the decisive adequate contact pressure until the peritoneal sheets are firmly connected (decisive safety factor in every PEG) is not controlled or not permanently guaranteed (Duckworth-Mothes et al. 2022).
JET-PEG
Positioning the internal catheter in the optimal location in the flexura duodenojejunalis (Fig. 1) is often problematic due to technical problems with a normal gastroscope and insufficient BTS technique. Frequent dislocations of the internal catheter cause repeated follow-up interventions.
Direct puncture
In this technique (better known as trocar puncture), 2 gastropexy sutures should be applied first (although 3 sutures are more favourable for topographical reasons alone). The subsequent puncture with the extremely pointed and sharp-edged trocar in the way specified in the instructions for use and literature carries the real risk of a faulty puncture of the posterior wall of the stomach, which can have life-threatening consequences due to the location of the aorta and pancreas in this area.
Simple measures can be taken to optimise the apposition area on the one hand and to eliminate the risk of malpuncture on the other (Grund et al. 2006a; Grund and Zipfel 2016; Duckworth-Mothes et al. 2022).
This method is not yet suitable for intrajejunal levodopa application via JET-PEG because the device does not allow for the insertion of a thinner internal catheter into the balloon catheter.
Discussion/consequences for practice
The described deficiencies (see Chapter 3) of the conventional technique—in addition to problems with follow-up care (Farrag et al. 2019)—are undoubtedly to be regarded as the main causes of the high complication rates (Grund et al. 2006a, b; Grund and Ingenpass 2007). Recommendations for an alternative technique resulting from this deficit analysis have now been successfully applied to high numbers of patients (Grund et al. 2021; Kishta et al. 2021; Schumacher et al. 2022).
The decisive steps of these new developments are presented and discussed here, particularly with regard to the indication of levodopa application.
Transnasal tubes, in this case nasoenteric tubes
In principle, such tubes are suitable for intrajejunal levodopa application (Fig. 1). However, their use for this indication is limited to a test phase (whether and how the local levodopa application works), since in the long-term course the inconvenience to the patient caused by the tube is usually not tolerated (Table 1).
FDZ-PEG
Standardised and careful preparation of the patient, team and instruments are obligatory prerequisites after clear indication, information and consent of the patient ((Grund et al. 2006b) as well as Table 2).
It is generally important for the proper technique to be applied:
To reduce the complication rate, necessary technical details must be intensively brought to the attention of the doctor and assistant and carefully observed. This is indispensable for all types of PEG placement, but especially for critical cases, which undoubtedly include levodopa application in iPS. For these patients, a complication of any kind is particularly serious.
Local anaesthesia must be administered in a targeted and deliberate manner according to defined, layer-specific guidelines (Fig. 2).
Initial steps for PEG placement. A Diaphany and marking. B Horizontal injection of local anaesthetic, superficial subcutaneous in a fan technique. Red dot: injection site of local anaesthetic, green dot: planned later insertion site of PEG. Note: hand position and support technique. C Vertical injection in support technique until the anaesthesia-needle has safely reached the stomach. D and E Here in the stomach the anaesthesia-needle is fixed close to the wall with endoscopic forceps
For the following puncture, it is not sufficient to "… just poke it where it shines brightly", an exact localisation of the puncture site and a correct puncture direction must be ensured. If a JET-PEG is planned, the direction of the puncture should be slightly in the direction of the pylorus to prevent looping of the internal catheter.
The aspiration test (Ponsky 1998) often recommended in the literature to exclude intestinal interposition is uncertain in principle for several reasons (Grund et al. 2006b); in dubio, a sonographic check of the initial anatomical position should definitely be performed.
After insertion, immediate fixation of the anaesthetic needle in the stomach with endoscopic forceps is an essential detail to prevent complication-prone displacement of the wall layers against each other (Fig. 2). The trocar cannula should also be fixed internally until the suture is inserted into the stomach (Fig. 3 D).
Scalpel incision and thread-trocar incision. A Converging puncture in support technique. Correct width of the stitch channel by No. 11 scalpel with 7.5 mm base width. B Insertion of the thread-trocar in identical manner, anaesthesia-needle and attached syringe serve as aiming aid. C Insertion of the thread. D and E Grasping the thread and securing it by pulling the forceps into the endoscope for a short distance
The puncture incision (obligatory for several reasons with a No.11 scalpel, see Fig. 3A) and insertion of the suture trocar in a support technique follow the laws of trigonometry (Fig. 3A, B).
When passing the suture and the PEG tube from intragastral to external (Fig. 4), the base of the tongue must be protected with the finger to avoid bleeding (Fig. 4B).
Further steps until the PEG tube is passed through the abdominal wall. A Endoscope together with forceps and thread is withdrawn orally. B The thread-loop and the PEG tube are connected in front of the mouth, then the tube is pulled outwards through the abdominal wall by the abdominal thread using short-stroke wrapping movements. Protect the base of the tongue with your finger. C Immediately after the tube has passed through, it is held under slight tension (prophylaxis of a pneumoperitoneum, thereby increasing diagnostic certainty in the event of the occurrence of abdominal pain after the PEG: If, despite this pneumoperitoneum prophylaxis, a pneumoperitoneum can be detected postinterventionally, this indicates a complication that should be taken seriously and often needs for surgical intervention). D Fixation of the external retaining plate under the same defined traction and dressing. E Correctly retracted retaining plate; it lies smoothly against the stomach wall. F Retaining plate too loose, risk of peritonitis and infection. G Retaining plate too tight, risk of buried bumper syndrome (BBS)
There is a simple, easy-to-perform prophylaxis for easily avoiding pneumoperitoneum and thus diagnostic uncertainty (Fig. 4C).
The tightening force should be approx. 200 p (weight of 2 bars of chocolate) (Grund et al. 2006b) and neither fall below (risk of peritonitis and infection) nor exceed (risk of buried bumper syndrome (BBS)) (Table 3).
HYBRID PEG
The technique of thread pull-through PEG (FDZ-PEG) just described can be decisively improved by combining it with gastropexy (endoscopic suturing of the anterior gastric wall to the abdominal wall) (Hybrid-PEG) (Grund et al. 2021; Kishta et al. 2021; Duckworth-Mothes et al. 2022).
In general, the decisive factor for low complication rate of a PEG is the secure and immediate adhesion as well as permanent adhesion and sealing of the two serosa surfaces (peritoneum of the anterior abdominal wall and outer surface of the stomach) (Fig. 5).
Decisive local situation for the safety of a PEG. A It is well known that the stomach and the anterior abdominal wall must remain fixed in direct contact for many hours so that first fibrin adhesion and then connective tissue organisation can take place (red arrows) 1: Abdominal wall 2: Free abdominal cavity 3: Stomach B With a normal TPT: this is only possible directly under the holding plate (3) and with a prolonged optimal pressure force, which is difficult to guarantee in practice. C The solution to the problem lies in a primary endoscopically controlled gastropexy with three sutures. This results in a large contact area and optimal safety due to a large-area with immediate and also permanent apposition of the serosa layers (3). D Hybrid PEG: A normal TPT PEG is placed in the centre of the three gastropexy sutures, which can be loosely attached to the stomach wall here. Peritonitis, infection or BBS are safely avoided. Inset: Inner retaining plate with the three gastropexy sutures (yellow asterisks)
The combination of a primary gastropexy with subsequent TPT PEG in the centre of the 3 obligatory pexy sutures in the form of a Hybrid-PEG (Fig. 5) shows very good results with significantly lower complication rates than with conventional techniques (Kishta et al. 2021; Schumacher et al. 2022; Bojarski pers. comm.). Even if direct head-to-head RC-studies (which may be ethically problematic regarding the clear benefits of Hybrid-PEG) are missing, the plausibility of the method and the cited clinical results are convincing.
Hybrid PEG certainly has the potential to become the future standard for PEG systems (Kishta et al. 2021).
Few but crucial details apply to the placement of gastropexy sutures (Fig. 6, Table 4). The important ones are (Grund et al. 2006a; Grund et al. 2021; Duckworth-Mothes et al. 2022):
-
Control and correct handling of the pexy device with regular application of at least 3 sutures.
-
Adequate knotting technique for safe apposition of the wall layers (6 knots in opposite directions).
-
Consistent use of mini ball swabs (so-called "fipses") to underlay the knots to protect the skin, reduce pain and facilitate suture removal. (Fig. 6E, F).
Details for gastropexy: A Insertion of the gastropexy device under support technique. B after the double needle appears in the lumen, the catcher snare is advanced (blue arrow) and the thread from the second needle is inserted through the catcher snare (yellow arrow). C by closing the catcher snare, the thread is clamped at the needle. D after removing the suturing device, the sutures appearing on the abdominal wall can be knotted. E an instrumental knot is recommended for this (3 double knots in opposite directions, a mini ball swab ("Fips") is included under the knot. F After completion of 3 (!!!) gastropexy sutures, an TPT is placed in the centre, during which the retaining plates can be adapted loosely
JET-PEG
The placement of an inner catheter into a PEG (so-called JET-PEG) (Fig. 7) has been associated with a high rate of dislocations (Fig. 8, Table 5), which is particularly undesirable for the indication "levodopa application".
JET-PEG: an internal catheter is advanced through the PEG and inserted into the proximal jejunum. A Inner catheter tip appears in the gastric lumen (green arrow: prepared grasping forceps). B Tube tip grasped. C The inner catheter is brought into the proximal jejunum using the dragging technique (BTS). D Optimally positioned inner catheter
Primary and secondary dislocation can often be avoided by:
-
For primary insertion, direction of insertion towards the pylorus.
-
Safe mastery of OTW and BTS techniques (Grund and Ingenpaß 2007) for correct positioning of the inner catheter tip.
-
Avoiding tube portions that are too short or too long in the stomach.
-
Avoiding tube disjunction in the area of the Y-piece.
-
Fixation of the tube tip to the intestinal wall using haemostatic clips in case of recurrent dislocation (Fig. 9).
In case of recurrent dislocation, prophylactic clip fixation of the inner catheter tip to the jejunal wall. A–C: Fixation with 2 haemostatic clips. D–F: radiological control of fixation exactly in the target area at the first jejunal loop, close to the flexura duodenojejunalis (see D). Yellow/blue arrows: Clips
Direct puncture = trocar puncture
The puncture of the extremely sharp, high-calibre steel trocar requires special technical precautions (Grund et al. 2006a):
To avoid serious complications, it is essential to observe:
-
During the puncture, a strong counter-traction is required upwards on the 3 pexy-sutures left longer.
-
A correct pulsed puncture technique under obligatory endoscopic view is essential.
EPJ = D-PEJ
Direct puncture of the small intestine is a recent development of PEG techniques (Fig. 10) (Mellert et al. 1994; Grund et al. 2006b) and is relevant as a substitute for a PEG in the case of a stomach that is no longer present or inaccessible in the surgical and intensive care context. The technique is quite critical and requires a decided and standardised procedure as an absolute prerequisite for similar success rates as with "normal" PEG. Defined prerequisites are (Grund et al. 2006a; Duckworth-Mothes et al. 2022):
-
Very exact diaphany and precise marking of the puncture site.
-
Obligatory application of spasmolytic drugs.
-
Internal fixation of anaesthetic needle and suture trocar without exception.
-
Particularly careful thread passage.
EPJ = D-PEJ; here the small intestine is punctured directly using the FDZ technique, thus creating direct access to the jejunum. A Fixation of the anaesthesia-needle. B Parallel insertion of the trocar (blue). C Internal fixation of the trocar and then grasping of the inserted thread. D Internal retaining plate in ideal position on the small intestine wall. E radiological control with contrast medium: EPJ lies correctly in the first jejunal loop. F CT check: correct position
In principle, an EPJ/D-PEJ would be ideal as a form of administration for intrajejunal levodopa administration, as the first jejunal loop is usually punctured just behind the flexura duodenojejunalis and thus the ideal resorption site for levodopa can largely be optimally hit.
However, the relatively demanding puncture technique, which requires a very experienced endoscopist, as well as concerns about complications with an TPT-only technique at this site (see above) have so far prevented larger numbers of PD patients from receiving an EPJ.
Newly developed puncture devices under development/trial could bring about a change here and establish the EPJ/D-PEJ in Hybrid technique as the optimal form of application for levodopa intrajejunal.
Another advantage of the EPJ technique would be the very short distance that the levodopa gel has to pass in the relatively narrow tube lumen (a few centimetres from the abdominal surface to the jejunum in contrast to > 60 cm with a JET-PEG) (see “Hydrodynamics of tubing systems”).
Hydrodynamics of tubing systems
So far, (too) little attention has been paid to the physics of flow in (narrow) tubes for levodopa application. Here, Hagen–Poiseuille's law (1839) plays an important role. It states that the inner diameter of the tube, which affects the 4th power, is the decisive factor for the volume flow or the required pressure. This has considerable consequences for small-calibre tube systems when applying the relatively highly viscous LCIG/LECIG gel into the intestinal lumen and represents a relatively frequent source of complications. These physical facts should also be given more attention in the context of medical technology.
Pumps
Pumps also appear to be frequent sources of complications (personal communication). Recent developments in mechatronics and accumulator technology (LiPo, LiFePo) have brought significant advances in the field of technology for portable pumps through increasing miniaturisation and extended running times, which above all makes outpatient care much easier. Unfortunately, the connecting pieces of the tubes are still different and incompatible in some cases.
Summary
Intrajejunal pump-controlled administration of levodopa is a standard form of therapy for advanced Parkinson's syndrome. It is realised via a so-called JET-PEG, i.e. a PEG with an inserted internal catheter into the jejunum.
In view of the high complication rates, a critical analysis reveals an urgent need for improvement of the JET-PEG, especially by optimising the insertion technique. To achieve this, numerous modifications and optimisations of the conventional technique and strict adherence to the developed technical details are goal-oriented. In addition, new developments such as the Hybrid-PEG (combination of 3 gastropexy sutures with subsequent central thread pull-through technique of the PEG tube) contribute to a dramatic reduction in the complication rate. Further developments, especially with regard to application devices, are needed to make intrajejunal levodopa application even safer and more effective for the critical patient group with advanced iPS.
Considerations for practice
All physicians and assistants who care for patients with advanced iPS should be informed about the possibilities and problems of intrajejunal targeted levodopa application and work together to ensure that the multiple possibilities of avoiding complications can be realised through an optimised application technique when applying a JET-PEG. In principle, such patients should be treated in centres with appropriate experience and optimal follow-up care should be ensured.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BBS:
-
Buried bumper syndrome
- BTS:
-
Beneath the scope
- DBS:
-
Deep brain stimulation
- D-PEJ:
-
Direct percutaneous endoscopic jejunostomy = EPJ; Note: D-PEJ and EPJ are different names for the same procedure.
- EPJ:
-
Endoscopic percutaneous jejunostomy = D-PEJ
- TPT:
-
Thread pull-through
- IPS:
-
Idiopathic Parkinson's syndrome
- JET-PEG:
-
Jejunal tube through PEG
- LCIG:
-
Levodopa-carbidopa gastrointestinal gel
- NES:
-
Nasoenteric tube
- OTW:
-
Over the wire
- PEG:
-
Percutaneous endoscopic gastrostomy
- TNT:
-
Transnasal tube
References
AWMF (2016) S3-Leitlinie Idiopathisches Parkinson-Syndrom. AWMF Register-Nummer 030-01047
Boeykens K, Duysburgh I (2021) Prevention and management of major complications in percutaneous endoscopic gastrostomy. BMJ Open Gastroenterol 8(1):e000628
Dam-Larsen S, Darkahi B et al (2015) Best practice in placement of percutaneous endoscopic gastrostomy with jejunal extension tube for continuous infusion of levodopa carbidopa intestinal gel in the treatment of selected patients with Parkinson’s disease in the Nordic region. Scand J Gastroenterol 50(12):1500–1507
Duckworth-Mothes B, Zipfel A et al (2022) Perkutane Enterostomie: Schritt für Schritt. Teil 1: Perkutane Gastrostomien. Gastroenterologie up2date 17:209–223
Farrag K, Shastri YM et al (2019) Percutaneous endoscopic gastrostomy (PEG): a practical approach for long term management. BMJ 364:k5311
Fernandez HH, Vanagunas A et al (2013) Levodopa-carbidopa intestinal gel in advanced Parkinson’s disease open-label study: interim results. Parkinsonism Relat Disord 19(3):339–345
Gheorghe C, Dumitru E et al (2019) Percutaneous endoscopic gastrostomy with jejunal extension tube for the delivery of levodopa carbidopa intestinal gel: clinical practice guidelines of the Romanian Society of Digestive Endoscopy. J Gastrointestin Liver Dis 28(3):349–354
Grund KE (2006) personal communication
Grund KE, Ingenpaß R (2007) Endoskopisch gelegte Ernährungssonden: Technische Tipps und Tricks. Teil 4: Nasogastrale und nasoenterale Sonden zur Ernährung. Endo Heute 20(164–172):164
Grund KE, Zipfel A (2016) Komplikationen bei perkutaner endoskopischer Gastrostomie (PEG). Allgemein- Und Viszeralchirurgie up2date 10(02):89–104
Grund KE, Zipfel A (2019) Flexible Endoskopie – Ausbildung und Training speziell für Chirurgen. Allgemein- und Viszeralchirurgie up2date; 13:403–416. https://doi.org/10.1055/a-0756-6137
Grund KE, Ingenpass R et al (2006a) Endoskopisch gelegte Ernährungssonden: Technische Tipps und Tricks. Teil 2: JET-PEG und Direktpunktion. Endo Heute 19:158–164
Grund KE, Königsrainer I et al (2006b) Endoskopisch gelegte Ernährungssonden: Technische Tipps und Tricks; Teil 1: PEG und EPJ in Fadendurchzugsmethode. Endo Heute 19:98–105
Grund KE, Zipfel A et al (2021) Sonden und PEGs zur Ernährung und Dekompression. Allgemein- Und Viszeralchirurgie up2date 15(02):127–148
Hucl T, Spicak J (2016) Complications of percutaneous endoscopic gastrostomy. Best Pract Res Clin Gastroenterol 30(5):769–781
Jost WH (2010) Gastrointestinal dysfunction in Parkinson’s disease. J. Neurol. Sci. 289:69–73
Jost WH (2014) Unwanted effects and interaction of intrajejunal levodopa/carbidopa administration. Expert Opin Drug Saf 13(4):447–458
Jost WH, Buhmann C et al (2022) Stellenwert der COMT-Hemmer in der Therapie motorischer Fluktuationen. Nervenarzt 93(10):1035–1045
Kishta J, Reich V et al (2021) Hybrid-PEG – Erfahrungen nach über 300 Hybrid-PEGs an der Charité. Endo-Praxis 37(02):95–99
Kratt T, Stüker D et al (2010) Evaluation of complications after PEG-placement without prophylactic antibiotics. Z Gastroenterol 48(08):P033
Lex KM, Kundt FS et al (2018) Using tube feeding and levodopa-carbidopa intestinal gel application in advanced Parkinson’s disease. Br J Nurs 27(5):259–262
Loser C, Aschl G et al (2005) ESPEN guidelines on artificial enteral nutrition–percutaneous endoscopic gastrostomy (PEG). Clin Nutr 24(5):848–861
Mellert J, Naruhn MB et al (1994) Direct endoscopic percutaneous jejunostomy (EPJ). Clinical results. Surg Endosc 8(8):867–869 (discussion 869–870)
Nyholm D, Stepien V (2014) Levodopa fractionation in Parkinson’s disease. J Parkinsons Dis 4(1):89–96
Ponsky JL (1998) Transilluminating percutaneous endoscopic gastrostomy. Endoscopy 30(7):656
Rabast U, Krause J et al (2008) Indikationen, Frühkomplikationen und Überlebensraten bei 444 konsekutiven PEG-Patienten unter enteraler Ernährung. Aktuelle Ernährungsmedizin 33(04):189–194
Salat D, Tolosa E (2013) Levodopa in the treatment of Parkinson’s disease: current status and new developments. J Parkinsons Dis 3(3):255–269
Schumacher L, Bojarski C et al (2022) Complication rates of direct puncture and pull-through techniques for percutaneous endoscopic gastrostomy - results from a large multicenter cohort. Endosc Int Open. https://doi.org/10.1055/a-1924-3525
Schwartz B, Ziegler P et al (2022) Complications of percutaneous endoscopic gastrostomy (PEG) tube placement by provider Training: a retrospective analysis. San Diego, DDW
Warnecke T, Schafer KH et al (2022) Gastrointestinal involvement in Parkinson’s disease: pathophysiology, diagnosis, and management. NPJ Parkinsons Dis 8(1):31
Acknowledgements
The authors would like to thank Dr. Jasmine Fokkens and Prof. Dr. Christian Bojarski for their help in preparing the manuscript and Mrs. Elena Niedermayer for her help with the graphics.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Grund, K.E., Zipfel, A., Duckworth-Mothes, B. et al. Optimised endoscopic access for intrajejunal levodopa application in idiopathic Parkinson's syndrome. J Neural Transm 130, 1383–1394 (2023). https://doi.org/10.1007/s00702-023-02601-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-023-02601-0