Abstract
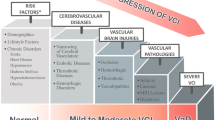
The regulation of cerebral blood flow (CBF) is a complex and tightly controlled function ensuring delivery of oxygen and nutrients and removal of metabolic wastes from brain tissue. Cerebral vasoreactivity (CVR) refers to the ability of the nervous system to regulate CBF according to metabolic demands or changes in the microenvironment. This can be assessed through a variety of nuclear medicine and imaging techniques and protocols. Several studies have investigated the association of CVR with physiological and pathological conditions, with particular reference to the relationship with cognitive impairment and cerebrovascular disorders (CVD). A better understanding of the interaction between CVR and cognitive dysfunction in chronic and particularly acute CVD could help improving treatment and rehabilitation strategies in these patients. In this paper, we reviewed current knowledge on CVR alterations in the context of acute and chronic CVD and cognitive dysfunction. Alterations in CVR and hemodynamics have been described in patients with both neurodegenerative and vascular cognitive impairment, and the severity of these alterations seems to correlate with CVR derailment. Furthermore, an increased risk of cognitive impairment progression has been associated with alterations in CVR parameters and hemodynamics. Few studies have investigated these associations in acute cerebrovascular disorders and the results are inconsistent; thus, further research on this topic is encouraged.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebral circulation delivers oxygen and nutrients and removes metabolic products from the brain tissue to ensure neuronal health and brain function. The high metabolic needs of the brain require a large volume of blood flow, comprising almost 20% of the total cardiac output. Therefore, the regulation of cerebral blood flow (CBF) is a complex and tightly controlled function (Aaslid 2006; Wolf 2015; Ashby and Mack 2021). The main mechanisms modulating cerebral hemodynamics, with the aim of adapting CBF to the metabolic demand of the brain, are cerebral autoregulation, vasomotor reactivity and neurovascular coupling (Claassen et al. 2021).
Cerebral autoregulation refers to the intrinsic ability of blood vessels to maintain CBF relatively constant within a wide range of values of systolic blood pressure (50–150 mmHg). Beyond these boundaries, CBF depends passively on perfusion pressure, thus entailing potentially harmful hypo- or hyperperfusion of cerebral tissue (Paulson et al. 1990). Cerebral autoregulation is accomplished through interactions and overlap of three different mechanisms (Wolf 2015): metabolic regulation, mediated by the release of vasoactive substances when oxygen is needed; myogenic regulation, mediated by adaptation of vascular tone to transmural blood pressure; and neurogenic regulation, mediated by sympathetic innervation of the vascular smooth cells. Interactions among these three components have been recently incorporated into the concept of neurovascular unit (NVU), a complex multi-cellular and extra-cellular structure consisting of endothelial cells, neurons, glia, smooth muscle cells, pericytes and extra-cellular matrix. NVU is involved in CBF regulation, blood–brain barrier functioning, immunological surveillance, trophic support and homeostatic cerebral balance. Neurovascular coupling adapts perfusion to increased metabolic demand in response to local changes in neural activity (Kugler et al. 2021) and several studies suggest its key role in signaling, metabolism and brain homeostasis. Impaired autoregulation has been identified in stroke and other neurovascular diseases (Immink et al. 2005), and functional MRI (fMRI) and positron emission tomography (PET) studies contributed at showing the derangement of NVU in patients with hypertension, ischemic stroke and chronic cerebrovascular disease (Wolf 2015).
Cerebral vasoreactivity
Cerebral vasoreactivity (CVR) refers to the ability of the nervous system to regulate CBF according to the metabolic requirements or chemical variations of the microenvironment (Wolf 2015; Claassen et al. 2021).
The evaluation of CVR is of great interest as an index of "hemodynamic reserve"(HR) in patients with cerebrovascular disease. The HR consists of potential residual vasodilatory capacity plus the possibility of increasing the rate of oxygen extraction from the blood compartment in critical CBF conditions (i.e., cerebral oligemia/ischemia) (Sette et al. 1989). The evaluation of vasoreactivity in a subject is obtained by provoking a transient vasodilatory stimulus and by measuring the variation of CBF. In the presence of a condition of 'maximal vasodilation' (i.e., severe hypoperfusion/oligemia), the flow variation obtained will be minimal or near to zero. Under physiological conditions, the variations in flow obtained are an indication of the entire vasomotor capacity of the subject's hemodynamic reserve.
Arterial pCO2 represents a powerful vasomotor stimulus for the resistance arteries of the cerebral circulation. CBF rises in response to increased pCO2 and decreased pH, whereas pO2 has opposite effects (Smoliński and Członkowska 2016). Small arterioles are extremely sensitive to the vasodilator effect of elevated arterial pCO2, with sigmoidal relationship, i.e., linear coupling for pCO2 values between 40 and 60 mmHg and non-linear relationship for values outside these limits (Wolf 2015). In particular, the maximal value of vasoreactivity index occurs for pCO2 values of 48 mmHg (Claassen 2007) and increases of 1 mmHg of blood pCO2 are accompanied by 2.5–5% increased flow rate values in the middle cerebral artery (MCA) compared to basal values (Ide et al. 2003).
Several nuclear medicine and imaging techniques are currently used to measure cerebral hemodynamics and test the response of cerebral vessels to vasoactive stimuli. PET allows direct measuring of CBF and is considered the gold standard to investigate CVR. However, other tools are available, such as near-infrared spectroscopy (NIRS), single photon emission computed tomography (SPECT), fMRI, computerized tomography (CT) with xenon-enhancement, and transcranial doppler sonography (TCD) (Herzig et al. 2008; Rijbroek et al. 2009; Herrera et al. 2016). Despite limited anatomical definition, blood-oxygen-level-dependent (BOLD) fMRI imaging allows rather precise regional specificity, displaying increased signal as the consequence of reduced deoxyhemoglobin concentration (Herrera et al. 2016). TCD is a sufficiently reliable, inexpensive, widely available and non-invasive technique for measuring hemodynamic parameters of main intracranial arteries (Herrera et al. 2016) such as peak systolic velocity (PSV), diastolic velocity (EDV), mean velocity (MV), and pulsatility index (PI) (Bishop et al. 1986; Lindegaard et al. 1987; Valdueza et al. 1999). Despite some intrinsic limitations, TCD with transient vasodilator stimuli has been widely used in clinical practice to assess CVR, reduction of MV indicating decreased global or regional CBF, and high PI pointing on increased microvascular resistance (Chen et al. 2022). Thus, CVR can be estimated by measuring changes of flow velocities in response to vasodilator stimuli in the main cerebral arteries as an indirect indication of changes in CBF (Poulin and Robbins 1996; Bathala et al. 2013). Several studies demonstrated the reliability of TCD in estimating cerebral hemodynamics and CBF variations compared with nuclear and functional imaging (Valdueza et al. 1997; Herrera et al. 2016), but only few reports compared blood flow velocities measured by TCD with CBF measured by PET in patients with symptomatic carotid artery stenosis, with rather variable results (Rijbroek et al. 2009).
In clinical practice, several tests are available to evaluate CVR. The CO2 reactivity test measures cerebral vasomotor response after approximately 90-s inhalation of CO2 mixtures (3–7%), allowing a simple, non-invasive, reliable and reproducible method (Ringelstein et al. 1992), which requires rather sophisticated technological setting. Acetazolamide test requires intravenous infusion of 500–2000 mg of the carbonic anhydrase inhibitor, acetazolamide, which causes transient, marked, cerebral acidosis and vasodilation (Wolf 2015). This test is widely used for its simplicity and the lack of need of patient’s collaboration; however, it is less accurate and reproducible compared to the former, and it is not devoid of undesirable side-effects such as arterial hypertension, headache, nausea and perioral dysesthesia. Moreover, acetazolamide injection may induce counterproductive hyperventilation, partially neutralizing the vasodilator effect of the drug (Ringelstein et al. 1992; Wolf 2015). Furthermore, standardized examination protocols are lacking for both CO2 inhalation and acetazolamide administration. Finally, breath-holding test (BHT) exploits hypercapnia generated by 30-s apnea to calculate a response index defined as breath-holding index (BHI). BHI is a non-invasive, easy to perform, well-tolerated and widely accepted test (Markus and Harrison 1992; Kidwell et al. 2001), despite the limited change of pCO2 (approximately 3–4 mmHg), the need for patient collaboration and the reduced reproducibility of this approach.
Alterations of CVR in aging and neurological disease
Aging is physiologically accompanied by changes of cerebral autoregulation mechanisms with the decrease of CBF and blood volume flow and the reduction of elasticity of small intracranial arteries (Zavoreo et al. 2010). This phenomenon has been associated with vascular changes depending on age-related atherosclerotic processes, which reduce arterial wall flexibility. Moreover, other cardiovascular risk factors such as hypertension, hyperlipemia, diabetes, coronary heart disease and smoking may contribute at reducing capability of cerebral vessels to react at vasodilator stimuli or increased metabolic demand (Gröschel et al. 2007; Staszewski et al. 2021).
Data from the literature show the impairment of CVR in several neurological disorders. Although the role of CVR impairment in the pathogenesis of neurodegenerative disorders has not been defined at present, one can hypothesize that reduced cerebrovascular reserve might further contribute at deteriorating disease progression (Smoliński and Członkowska 2016; Marcic et al. 2021).
In this narrative review, we focused on the impact of CVR on cerebrovascular diseases and cognitive impact. To this end, papers published in English, without publication date limit, were searched in Pubmed and Web of Science databases, using keywords related to: (i) brain circulation (e.g., “cerebral vasoreactivity”, “brain hemodynamics”, “cerebral blood flow”); (ii) cerebrovascular diseases (e.g., “cerebrovascular disease”, “stroke”, “carotid stenosis”, “small vessel disease”, etc.) (iii) cognitive impairement (e.g., “cognitive impairement”, “cognitive decline”, “dementia”, “MCI”, etc.). Search strategy included a combination of keywords, using the Boolean operators “AND” and “OR”. Search fields were restricted to the abstract, title, and keywords. Included papers were original peer-reviewed scientific journal articles, editorials, case studies, letters or reviews. Studies not examining the correlation between CVR, cognitive functions and CVD were excluded. Two independent reviewers [MS and GS] screened the titles and abstracts of all studies to identify potentially relevant articles. Duplicates were manually removed. Full texts of all included studies were then obtained and reviewed. The following 5 parameters were reviewed from the retrieved articles by two independent reviewers: (1) study characteristics; (2) participant characteristics; (3) tools for measuring CVR; (4) measure of cognitive function; and (5) main findings. Quantitative analysis and assessment of the risk of bias were not performed due to the narrative design of the study. The quality assessment was appraised by two independent reviewers (MS, EB); disagreements between evaluators were resolved through discussion.
CVR and cognitive impairment
Several studies demonstrated the correlation between alteration of brain vessel reactivity and impaired cognitive functions in patients with cognitive derangement. Arteriolosclerosis, amyloid angiopathy, atherosclerosis and lipohyalinosis have been associated with impaired cerebral hemodynamic and cognitive impairment (Chen et al. 2022). Alterations of cerebral vessel resistance using TCD, in particular the PI, and evaluation of CVR to hypercapnia using BHI have been consistently associated with cognitive decline and are indicative of cognitive impairment in Alzheimer’s disease (AD) and vascular dementia (VaD) (Keage et al. 2012). Several authors investigated the possible correlation between altered cerebral hemodynamic and cognitive functions in mild cognitive impairment (MCI) or AD. In general, low intracranial arterial MVF, increased vascular resistance (PI) and reduced vasoreactivity have been identified in these pathological conditions with respect to healthy subjects (Silvestrini et al. 2006; Lim et al. 2018; Cipollini et al. 2019; Chen et al. 2022). Moreover, it has been suggested that TCD may predict clinical progression of cognitive decline, higher PI and lower BHI in the middle cerebral artery being associated with stronger risk of conversion to dementia in subjects with MCI, with significant correlation between decreased BHI and reduced MoCA score (Silvestrini et al. 2006; Lim et al. 2018). Eventually, TCD may help differentiating individuals with MCI from healthy subjects (Zavoreo et al. 2010; Chung et al. 2017). Taken together, these data suggest that early cerebral microvascular abnormalities in the brain may anticipate the occurrence of significant cognitive impairment, and possibly precede the development of structural brain lesions identifiable on conventional imaging (Chen et al. 2022).
Several other factors have been shown to play a role along with CVR impairment in cognitive decline, including aging, altered brain energy demand, and hypoperfusion. Detailed analysis of these factors is beyond the scope of this work, exhaustive reviews on the relationships between hypoperfusion, brain energy demand and cognitive decline being available in the recent literature (Popa-Wagner et al. 2014, 2015; Ciacciarelli et al. 2020).
CVR in cerebrovascular diseases
Most studies investigating the relationships between impaired cerebral hemodynamic, CVR and cognitive impairment were carried out on subjects affected by cerebrovascular disorders. Research focused on presymptomatic subjects (carotid stenosis) (Silvestrini et al. 1996; Silvestrini et al. 2000; Markus and Cullinane 2001; Cheng et al. 2012; Zavoreo et al. 2013; Viticchi et al. 2021), acute ischemic stroke (Alvarez et al. 2004; Uzuner et al. 2013; Salinet et al. 2015, 2019; Altmann et al. 2016; Chi et al. 2020) and chronic cerebrovascular disorders (Provinciali et al. 1990; Matteis et al. 1998; Kidwell et al. 2001; Shiogai et al. 2002; Sabayan et al. 2012; Turk et al. 2016; Kisler et al. 2017; Bian et al. 2019; Staszewski et al. 2021).
Carotid stenosis
Cerebral perfusion is rather variable in subjects affected by carotid occlusive disease, and appears related to the degree of collateral blood supply rather than severity of stenosis (Silvestrini et al. 2000). Many subjects with steno-occlusive carotid disease develop compensatory vasodilation of ipsilateral arteries together with collateral circulation, and patients with high grade carotid stenosis display reduced CBF in the ipsilateral brain hemisphere, particularly in MCA borderline regions, that may revert towards normal values after revascularization therapy (Schroder et al. 2019). In these subjects, further vasodilator stimulus by hypercapnia will produce absent or markedly reduced vasodilator response (Silvestrini et al. 1996). The reduction of CVR is associated with increased risk of ipsilateral stroke or TIA in patients with carotid occlusion and, to a lesser extent, asymptomatic carotid stenosis (Viticchi et al. 2021). This suggests that assessment of CVR may help identifying high-risk patients who may benefit from revascularization.
There is also clear evidence for the association between carotid stenosis and the onset and progression of cognitive impairment, even in subjects with severe asymptomatic carotid stenosis (Cheng et al. 2012; Zavoreo et al. 2013; Viticchi et al. 2021), as if carotid stenosis might facilitate cognitive dysfunction through the combination of increased incidence of acute cerebrovascular lesions, microembolization, chronic hypoperfusion, and impairment of CVR (Viticchi et al. 2021). Indeed, impaired cerebral hemodynamics may lead to altered regional functional connectivity, particularly in the fronto-parietal network, in turn inducing cognitive dysfunction (Cheng et al. 2012).
Consequently, revascularization procedures have been hypothesized recently as a way to restore hemodynamically induced cognitive impairment. Further randomized clinical trials on large cohorts are required, however, to define the effectiveness and timing of medical and surgical/endovascular approaches to this issue (Viticchi et al. 2021).
Acute ischemic stroke
Cerebral hemodynamic impairment plays a significant pathophysiological role in the acute phase of cerebral ischemia, and somehow predicts stroke severity, progression and long-term outcome. The correlation between impairment of CVR and the occurrence of acute ischemic stroke in patients with severe internal carotid artery stenosis has been convincingly confirmed (Gur et al. 1996; Silvestrini et al. 1996, 2000; Markus and Cullinane 2001; Cheng et al. 2012; Viticchi et al. 2021). However, the role of altered CVR in patients with acute ischemic stroke without significant carotid stenosis has not been clarified at present.
Hemodynamic factors and cerebral hemodynamic reserve have been related to the final infarct volume, unfavorable long-term outcome and most neurologic complications after acute stroke (Alvarez et al. 2004). Thus, cerebral hemodynamic parameters are progressively compromised according to stroke severity: moderate and severe stroke are accompanied by greater CBF asymmetries between the affected and unaffected hemisphere, derangement of autoregulation mechanisms in the affected hemisphere, and bilateral NVU impairment (Salinet et al. 2019). Furthermore, studies demonstrated depressed CBF response to neural activation and CO2 (Salinet et al. 2015), and impaired vasoreactivity appears coupled with poorer functional outcome (Salinet et al. 2019). Other reports showed the association between cerebral hemodynamic alterations and cognitive performances in patients with acute cerebral ischemia. In the case of lacunar infarcts, the increase in PI has been correlated to impairment of executive functions (Sivakumar et al. 2017). The increase of PI measured proximally to the blood vessels reflects the increased distal vascular resistance and consequent reduction of diastolic flow that may depend on alterations of microcirculation secondary to subcortical ischemic events (Uzuner et al. 2013). With this respect, studies on animal models showed the dysfunction of capillary pericytes as the consequence of oxygen radical production in ischemia (Yemisci et al. 2009). This may lead to vascular contraction and hypoperfusion, in turn causing functional alterations of connectivity within associative networks (Chi et al. 2020). A recent pilot study, however, did not support such hypothesis, and suggested that hemodynamic alterations may contribute at worsening cognitive performances transiently, during the first 3–6 months following acute subcortical ischemia (Suministrado et al. 2017).
Eventually, animal studies and neuropathological findings in humans confirm that relevant angiogenesis occurs in post-stroke brain tissue (Buga et al. 2014). The impact of post-stroke angiogenesis on CVR has not been defined completely at present, despite the theoretical observation of partial increase of the cerebrovascular bed. Future studies are advised to identify whether these newly generated vessels develop normal response to stimuli modulating CVR.
Chronic cerebrovascular disorders
A conspicuous body of research focused on the association between impaired CVR and cerebral small vessel disease (SVD). Microangiopathy represents a prominent cause of lacunar stroke and vascular dementia (VaD) (Staszewski et al. 2021). SVD is a dynamic and progressive pathology involving several components of the NVU, generating dysfunction of signaling pathways that may be responsible for CBF deregulation in VaD (Kisler et al. 2017). TCD with BHI showed the reduction of CVR in patients with SVD with respect to control subjects (Staszewski et al. 2021). Moreover, the results of meta-analyses demonstrated that alteration of cerebral hemodynamic in VD patients is more pronounced that AD (Sabayan et al. 2012). Thus, patients with SVD and chronic cerebrovascular pathology display increased rate of blood flow and higher PI in the larger intracranial arteries, which correlate with the severity of cognitive impairment, the vascular Hachinski scale score, and the degree of leukoaraiosis at MRI (Kidwell et al. 2001; Turk et al. 2016). Kindwell and collaborators (2001) also showed that the PI is an independent predictor of SVD, with specificity and sensitivity values of 89% and 86% for periventricular hyperintensities and 70% and 73% for deep matter hyperintensities. In addition, other studies showed the association between multi-infarct leukoencephalopathy and CVR alteration as measured by acetazolamide test (Shiogai et al. 2002) or in response to apnea (Provinciali et al. 1990; Matteis et al. 1998). In particular, reduction of CVR as measured by BHI seems directly associated with the severity of leukoaraiosis, and patients with lower BHI and moderate-to-severe SVD (grade 2–3 at the Fazekas scale) display lower performances at the MoCA as well as other tests measuring executive functions (Turk et al. 2016; Bian et al. 2019). BHI might, therefore, be helpful for evaluating the alterations of CVR in subjects suffering from leukoaraiosis, and represent an indicator of cognitive dysfunction in these patients.
Obstructive sleep apnea syndrome (OSAS) is a frequent disease in aging and a well-described condition associated with CVR impairment. OSAS is a disorder characterized by recurring episodes of obstruction and partial or complete collapse of the rhino‐oropharynx during sleep. These are caused by anatomical upper airway alteration combined with impaired ventilatory control or alteration of neurofunctional control of rhino- and oropharyngeal muscles. The episodes lead to intermittent oxygen desaturation and are associated with sleep fragmentation, cerebrovascular and cardiovascular disease, excessive daytime sleepiness and cognitive dysfunction. A comprehensive review by Beaudin et al. (2017) addressed the impact of OSA on cardiovascular and cerebrovascular regulation. A more recent comparative study carried out by our group (Piraino et al. 2019) on 40 patients suffering from moderate-to-severe OSAS (AHI ≥ 15) showed the tendency to increased BHI and the significant reduction of IMT after continuous positive airway pressure (CPAP) treatment, therefore suggesting that CPAP treatment may improve CVR and reduce endothelial inflammation.
Association between CVR and brain regions and functions
In recent years, evidence has accumulated on the association between impaired cerebral hemodynamics and cognitive functions in patients suffering from neurological disorders, in particular cerebrovascular diseases, as if reduction of cerebral blood flow and brain perfusion may contribute to cognitive derangement (Mori et al. 1994; Firbank et al. 2011). Dementia associated with CVD is rather common, affecting 25–30% of elderly stroke survivors as post-stroke dementia (PSD), which frequently meets criteria for VaD (Allan et al. 2011). Cognitive impairment in VaD is frequently sustained by damage of the frontal–subcortical circuits (Kalaria and Ihara 2013). The frontal lobe is particularly vulnerable to vascular-based pathology (Jobson et al. 2021), and previous studies reported that 50% of stroke survivors display deficits of executive functions, regardless the severity or subtype of cerebrovascular event. A further potential link for developing PSD is the preferential location in the frontal lobe of white matter vascular pathology supported by astrogliosis or clasmatodendritic changes in microvessel with irreversible astrocyte injury, disruption of gliovascular interactions and blood–brain barrier (Chen et al. 2016). Previous studies showed that medullary arteries and the telencephalic white matter of the frontal lobe are particularly susceptible to cerebral hemodynamic disturbance (Ihara et al. 2010), and that a correlation exists between reduced cerebral blood flow and these pathological changes, as if cerebral hypoperfusion might represent a direct cause of vascular pathology (Qin et al. 2010) in particular in elderly subjects. Indeed, there is evidence that clasmatodendrosis occurs acutely after induction of cerebral hypoperfusion in non-human primates (Chen et al. 2016), and that impairment of cognitive performances within the first three months post-stroke might predict future recovery (Park et al. 2015).
Executive functions are essential for regulating goal-oriented behaviors and responding to new and novel settings, by combining working memory, planning, orientation problem-solving, self-monitoring and error correcting. Recent studies suggest that executive dysfunction in stroke patients produces reduced performances in both basic and complex activities of daily living and compromises rehabilitation outcomes (Zinn et al. 2007; Chung et al. 2013). Therefore, one can speculate that stroke outcome and post-rehabilitation improvement might benefit from precocious identification and management of executive dysfunction as well as by rapid therapeutic management by compensatory and stimulating approaches (Zinn et al. 2007).
Conclusions and perspectives
Table 1 summarizes the main characteristics of cerebral vasomotor reactivity in aging, cerebrovascular disease and cognitive impairment. In conclusion, the relationship between impaired cerebral hemodynamics, in particular CVR, and executive functions has been clearly defined in chronic cerebrovascular disease subjects but is rather limited in acute stroke patients. Future research in this field should be focused on defining the interactions between impaired cerebral hemodynamic parameters and executive functions in the acute phase of cerebral ischemia, and the potential predictive role of these changes on long-term functional outcomes after acute ischemic stroke. Thus, cerebral hemodynamic should be monitored over time following acute ischemic stroke to investigate its possible predictive role on response to neurorehabilitation and long-term functional outcome. Eventually, differences in cerebral hemodynamic changes should be investigated with respect to location and severity of acute stroke, to plan personalized therapeutic strategies, and the relationships between impaired hemodynamic parameters and other cardiovascular risk factors on cognitive outcome should be defined. This would allow the results of experimental and human studies to be translated into clinical practice and help select the best parameters to identify high-risk patients, predict functional outcome, and monitor patients over time.
Abbreviations
- AD:
-
Alzheimer’s disease
- BHI:
-
Breath-holding index
- BHT:
-
Breath-holding test
- CBF:
-
Cerebral blood flow
- CT:
-
Computerized tomography
- CVD:
-
Cerebrovascular disorders
- CVR:
-
Cerebral vasoreactivity
- EDV:
-
End diastolic velocity
- fMRI:
-
Functional MRI
- MCA:
-
Middle cerebral artery
- MCI:
-
Mild cognitive impairment
- MVF:
-
Mean velocity flow
- NIRS:
-
Near-infrared spectroscopy
- NVU:
-
Neurovascular unit
- OSAS:
-
Obstructive sleep apnea syndrome
- PET:
-
Positron emission tomography
- PI:
-
Pulsatility index
- PSD:
-
Post-stroke dementia
- PSV:
-
Peak systolic velocity
- PECT:
-
Photon emission computed tomography
- SVD:
-
Small vessel disease
- TCD:
-
Transcranial Doppler
- VD:
-
Vascular dementia
References
Aaslid R (2006) Cerebral autoregulation and vasomotor reactivity. Front Neurol Neurosci 21:216–228. https://doi.org/10.1159/000092434
Allan LM, Rowan EN, Firbank MJ et al (2011) Long term incidence of dementia, predictors of mortality and pathological diagnosis in older stroke survivors. Brain 134:3716–3727. https://doi.org/10.1093/brain/awr273
Altmann M, Thommessen B, Rønning OM et al (2016) Middle cerebral artery pulsatility index is associated with cognitive impairment in lacunar stroke. J Neuroimaging 26:431–435. https://doi.org/10.1111/jon.12335
Alvarez FJ, Segura T, Castellanos M et al (2004) Cerebral hemodynamic reserve and early neurologic deterioration in acute ischemic stroke. J Cereb Blood Flow Metab 24:1267–1271. https://doi.org/10.1097/01.WCB.0000139370.93203.4A
Ashby JW, Mack JJ (2021) Endothelial control of cerebral blood flow. Am J Pathol 191:1906–1916. https://doi.org/10.1016/j.ajpath.2021.02.023
Bathala L, Mehndiratta MM, Sharma VK (2013) Transcranial Doppler: technique and common findings (Part 1). Ann Indian Acad Neurol 16:174–179. https://doi.org/10.4103/0972-2327.112460
Beaudin AE, Waltz X, Hanly PJ, Poulin MJ (2017) Impact of obstructive sleep apnoea and intermittent hypoxia on cardiovascular and cerebrovascular regulation. Exp Physiol 102(7):743–763. https://doi.org/10.1113/EP086051
Bian Y, Wang J-C, Sun F et al (2019) Assessment of cerebrovascular reserve impairment using the breath-holding index in patients with leukoaraiosis. Neural Regen Res 14:1412–1418. https://doi.org/10.4103/1673-5374.251332
Bishop CC, Powell S, Rutt D, Browse NL (1986) Transcranial Doppler measurement of middle cerebral artery blood flow velocity: a validation study. Stroke 17:913–915. https://doi.org/10.1161/01.str.17.5.913
Buga AM, Margaritescu C, Scholz CJ, Radu E, Zelenak C, Popa-Wagner A (2014) Transcriptomics of post-stroke angiogenesis in the aged brain. Front Aging Neurosci 18(6):44. https://doi.org/10.3389/fnagi.2014.00044
Chen A, Akinyemi RO, Hase Y et al (2016) Frontal white matter hyperintensities, clasmatodendrosis and gliovascular abnormalities in ageing and post-stroke dementia. Brain 139:242–258. https://doi.org/10.1093/brain/awv328
Chen W-T, Chi N-F, Cheng H-M et al (2022) Associations between cerebral vasoreactivity and cognitive function in the middle-aged non-demented population. J Alzheimers Dis 86:679–690. https://doi.org/10.3233/JAD-215317
Cheng H-L, Lin C-J, Soong B-W et al (2012) Impairments in cognitive function and brain connectivity in severe asymptomatic carotid stenosis. Stroke 43:2567–2573. https://doi.org/10.1161/STROKEAHA.111.645614
Chi N-F, Hu H-H, Chan L et al (2020) Impaired cerebral autoregulation is associated with poststroke cognitive impairment. Ann Clin Transl Neurol 7:1092–1102. https://doi.org/10.1002/acn3.51075
Chung CSY, Pollock A, Campbell T et al (2013) Cognitive rehabilitation for executive dysfunction in adults with stroke or other adult non-progressive acquired brain damage. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD008391.pub2
Chung C-P, Lee H-Y, Lin P-C, Wang P-N (2017) Cerebral artery pulsatility is associated with cognitive impairment and predicts dementia in individuals with subjective memory decline or mild cognitive impairment. J Alzheimers Dis 60:625–632. https://doi.org/10.3233/JAD-170349
Ciacciarelli A, Sette G, Giubilei F, Orzi F (2020) Chronic cerebral hypoperfusion: an undefined, relevant entity. J Clin Neurosci 73:8–12. https://doi.org/10.1016/j.jocn.2020.01.026
Cipollini V, Sette G, Bossù P et al (2019) Neurovascular dysfunction in Alzheimer disease: assessment of cerebral vasoreactivity by ultrasound techniques and evaluation of circulating progenitor cells and inflammatory markers. Alzheimer Dis Assoc Disord 33:212–219. https://doi.org/10.1097/WAD.0000000000000331
Claassen JAHR, Zhang R, Fu Q et al (2007) Transcranial Doppler estimation of cerebral blood flow and cerebrovascular conductance during modified rebreathing. J Appl Physiol 102:870–877. https://doi.org/10.1152/japplphysiol.00906.2006
Claassen JAHR, Thijssen DHJ, Panerai RB, Faraci FM (2021) Regulation of cerebral blood flow in humans: physiology and clinical implications of autoregulation. Physiol Rev 101:1487–1559. https://doi.org/10.1152/physrev.00022.2020
Firbank MJ, He J, Blamire AM et al (2011) Cerebral blood flow by arterial spin labeling in poststroke dementia. Neurology 76:1478–1484. https://doi.org/10.1212/WNL.0b013e318217e76a
Gröschel K, Terborg C, Schnaudigel S et al (2007) Effects of physiological aging and cerebrovascular risk factors on the hemodynamic response to brain activation: a functional transcranial Doppler study. Eur J Neurol 14:125–131. https://doi.org/10.1111/j.1468-1331.2006.01563.x
Gur AY, Bova I, Bornstein NM (1996) Is impaired cerebral vasomotor reactivity a predictive factor of stroke in asymptomatic patients? Stroke 27:2188–2190. https://doi.org/10.1161/01.str.27.12.2188
Herrera CRC, Beltramini GC, Avelar WM et al (2016) Cerebral vasomotor reactivity assessment using transcranial Doppler and MRI with apnea test. Braz J Med Biol Res 49:e5437. https://doi.org/10.1590/1414-431X20165437
Herzig R, Hlustík P, Skoloudík D et al (2008) Assessment of the cerebral vasomotor reactivity in internal carotid artery occlusion using a transcranial Doppler sonography and functional MRI. J Neuroimaging 18:38–45. https://doi.org/10.1111/j.1552-6569.2007.00168.x
Ide K, Eliasziw M, Poulin MJ (2003) Relationship between middle cerebral artery blood velocity and end-tidal PCO2 in the hypocapnic-hypercapnic range in humans. J Appl Physiol 95:129–137. https://doi.org/10.1152/japplphysiol.01186.2002
Ihara M, Polvikoski TM, Hall R et al (2010) Quantification of myelin loss in frontal lobe white matter in vascular dementia, Alzheimer’s disease, and dementia with Lewy bodies. Acta Neuropathol 119:579–589. https://doi.org/10.1007/s00401-009-0635-8
Immink RV, van Montfrans GA, Stam J et al (2005) Dynamic cerebral autoregulation in acute lacunar and middle cerebral artery territory ischemic stroke. Stroke 36:2595–2600. https://doi.org/10.1161/01.STR.0000189624.06836.03
Jobson DD, Hase Y, Clarkson AN, Kalaria RN (2021) The role of the medial prefrontal cortex in cognition, ageing and dementia. Brain Commun 3:fcab125. https://doi.org/10.1093/braincomms/fcab125
Kalaria RN, Ihara M (2013) Dementia: vascular and neurodegenerative pathways-will they meet? Nat Rev Neurol 9:487–488. https://doi.org/10.1038/nrneurol.2013.164
Keage HAD, Churches OF, Kohler M et al (2012) Cerebrovascular function in aging and dementia: a systematic review of transcranial Doppler studies. Dement Geriatr Cogn Dis Extra 2:258–270. https://doi.org/10.1159/000339234
Kidwell CS, El-Saden S, Livshits Z et al (2001) Transcranial Doppler pulsatility indices as a measure of diffuse small-vessel disease. J Neuroimaging 11:229–235. https://doi.org/10.1111/j.1552-6569.2001.tb00039.x
Kisler K, Nelson AR, Montagne A, Zlokovic BV (2017) Cerebral blood flow regulation and neurovascular dysfunction in Alzheimer disease. Nat Rev Neurosci 18:419–434. https://doi.org/10.1038/nrn.2017.48
Kugler EC, Greenwood J, MacDonald RB (2021) The “neuro-glial-vascular” unit: the role of glia in neurovascular unit formation and dysfunction. Front Cell Dev Biol 9:732820. https://doi.org/10.3389/fcell.2021.732820
Lim E-Y, Yang D-W, Cho A-H, Shim YS (2018) Cerebrovascular hemodynamics on transcranial Doppler ultrasonography and cognitive decline in mild cognitive impairment. J Alzheimers Dis 65:651–657. https://doi.org/10.3233/JAD-180026
Lindegaard KF, Lundar T, Wiberg J et al (1987) Variations in middle cerebral artery blood flow investigated with noninvasive transcranial blood velocity measurements. Stroke 18:1025–1030. https://doi.org/10.1161/01.str.18.6.1025
Marcic M, Marcic L, Marcic B et al (2021) Cerebral vasoreactivity evaluated by transcranial color Doppler and breath-holding test in patients after SARS-CoV-2 infection. J Pers Med 11:379. https://doi.org/10.3390/jpm11050379
Markus H, Cullinane M (2001) Severely impaired cerebrovascular reactivity predicts stroke and TIA risk in patients with carotid artery stenosis and occlusion. Brain 124:457–467. https://doi.org/10.1093/brain/124.3.457
Markus HS, Harrison MJ (1992) Estimation of cerebrovascular reactivity using transcranial Doppler, including the use of breath-holding as the vasodilatory stimulus. Stroke 23:668–673. https://doi.org/10.1161/01.str.23.5.668
Matteis M, Silvestrini M, Troisi E et al (1998) Cerebral hemodynamic patterns during stimuli tasks in multi-infarct and Alzheimer types of dementia. Acta Neurol Scand 97:374–380. https://doi.org/10.1111/j.1600-0404.1998.tb05969.x
Mori S, Sadoshima S, Ibayashi S et al (1994) Relation of cerebral blood flow to motor and cognitive functions in chronic stroke patients. Stroke 25:309–317. https://doi.org/10.1161/01.str.25.2.309
Park YH, Jang J-W, Park SY et al (2015) Executive function as a strong predictor of recovery from disability in patients with acute stroke: a preliminary study. J Stroke Cerebrovasc Dis 24:554–561. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.09.033
Paulson OB, Strandgaard S, Edvinsson L (1990) Cerebral autoregulation. Cerebrovasc Brain Metab Rev 2:161–192
Piraino A, Sette G, D’Ascanio M, La Starza S, Aquilini M, Ricci A (2019) Effect of OSAS on cerebral vasoreactivity and cIMT before and after CPAP treatment. Clin Respir J 13(9):555–559. https://doi.org/10.1111/crj.13057 (Epub 2019 Jul 24)
Popa-Wagner A, Buga AM, Tica AA, Albu CV (2014) Perfusion deficits, inflammation and aging precipitate depressive behaviour. Biogerontology 15:439–448. https://doi.org/10.1007/s10522-014-9516-1
Popa-Wagner A, Buga A-M, Popescu B, Muresanu D (2015) Vascular cognitive impairment, dementia, aging and energy demand. A vicious cycle. J Neural Transm (vienna) 122(Suppl 1):S47-54. https://doi.org/10.1007/s00702-013-1129-3
Poulin MJ, Robbins PA (1996) Indexes of flow and cross-sectional area of the middle cerebral artery using Doppler ultrasound during hypoxia and hypercapnia in humans. Stroke 27:2244–2250. https://doi.org/10.1161/01.str.27.12.2244
Provinciali L, Minciotti P, Ceravolo G et al (1990) Transcranial Doppler sonography as a diagnostic tool in vascular dementia. Eur Neurol 30:98–103. https://doi.org/10.1159/000117320
Qin A-P, Liu C-F, Qin Y-Y et al (2010) Autophagy was activated in injured astrocytes and mildly decreased cell survival following glucose and oxygen deprivation and focal cerebral ischemia. Autophagy 6:738–753. https://doi.org/10.4161/auto.6.6.12573
Rijbroek A, Boellaard R, Vriens EM et al (2009) Comparison of transcranial Doppler ultrasonography and positron emission tomography using a three-dimensional template of the middle cerebral artery. Neurol Res 31:52–59. https://doi.org/10.1179/174313208X325191
Ringelstein EB, Van Eyck S, Mertens I (1992) Evaluation of cerebral vasomotor reactivity by various vasodilating stimuli: comparison of CO2 to acetazolamide. J Cereb Blood Flow Metab 12:162–168. https://doi.org/10.1038/jcbfm.1992.20
Sabayan B, Jansen S, Oleksik AM et al (2012) Cerebrovascular hemodynamics in Alzheimer’s disease and vascular dementia: a meta-analysis of transcranial Doppler studies. Ageing Res Rev 11:271–277. https://doi.org/10.1016/j.arr.2011.12.009
Salinet ASM, Robinson TG, Panerai RB (2015) Effects of cerebral ischemia on human neurovascular coupling, CO2 reactivity, and dynamic cerebral autoregulation. J Appl Physiol 118:170–177. https://doi.org/10.1152/japplphysiol.00620.2014
Salinet AS, Silva NC, Caldas J et al (2019) Impaired cerebral autoregulation and neurovascular coupling in middle cerebral artery stroke: influence of severity? J Cereb Blood Flow Metab 39:2277–2285. https://doi.org/10.1177/0271678X18794835
Schröder J, Heinze M, Günther M, Cheng B, Nickel A, Schröder T, Fischer F, Kessner SS, Magnus T, Fiehler J, Larena-Avellaneda A, Gerloff C, Thomalla G (2019) Dynamics of brain perfusion and cognitive performance in revascularization of carotid artery stenosis. Neuroimage Clin 22:101779. https://doi.org/10.1016/j.nicl.2019.101779
Sette G, Baron JC, Mazoyer B et al (1989) Local brain haemodynamics and oxygen metabolism in cerebrovascular disease. Positron emission tomography. Brain 112(Pt 4):931–951. https://doi.org/10.1093/brain/112.4.931
Shiogai T, Uebo C, Makino M et al (2002) Acetazolamide vasoreactivity in vascular dementia and persistent vegetative state evaluated by transcranial harmonic perfusion imaging and Doppler sonography. Ann N Y Acad Sci 977:445–453. https://doi.org/10.1111/j.1749-6632.2002.tb04850.x
Silvestrini M, Troisi E, Matteis M et al (1996) Transcranial Doppler assessment of cerebrovascular reactivity in symptomatic and asymptomatic severe carotid stenosis. Stroke 27:1970–1973. https://doi.org/10.1161/01.str.27.11.1970
Silvestrini M, Vernieri F, Pasqualetti P et al (2000) Impaired cerebral vasoreactivity and risk of stroke in patients with asymptomatic carotid artery stenosis. JAMA 283:2122–2127. https://doi.org/10.1001/jama.283.16.2122
Silvestrini M, Pasqualetti P, Baruffaldi R et al (2006) Cerebrovascular reactivity and cognitive decline in patients with Alzheimer disease. Stroke 37:1010–1015. https://doi.org/10.1161/01.STR.0000206439.62025.97
Sivakumar L, Riaz P, Kate M et al (2017) White matter hyperintensity volume predicts persistent cognitive impairment in transient ischemic attack and minor stroke. Int J Stroke 12:264–272. https://doi.org/10.1177/1747493016676612
Smoliński Ł, Członkowska A (2016) Cerebral vasomotor reactivity in neurodegenerative diseases. Neurol Neurochir Pol 50:455–462. https://doi.org/10.1016/j.pjnns.2016.07.011
Staszewski J, Dȩbiec A, Skrobowska E, Stȩpień A (2021) Cerebral vasoreactivity changes over time in patients with different clinical manifestations of cerebral small vessel disease. Front Aging Neurosci 13:727832. https://doi.org/10.3389/fnagi.2021.727832
Suministrado MSP, Shuang EWY, Xu J et al (2017) Poststroke cognitive decline is independent of longitudinal changes in cerebral hemodynamics parameters. J Neuroimaging 27:326–332. https://doi.org/10.1111/jon.12395
Turk M, Zaletel M, PretnarOblak J (2016) Characteristics of cerebral hemodynamics in patients with ischemic leukoaraiosis and new ultrasound indices of ischemic leukoaraiosis. J Stroke Cerebrovasc Dis 25:977–984. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.12.045
Uzuner N, Özdemir Ö, TekgölUzuner G (2013) Relationship between pulsatility index and clinical course of acute ischemic stroke after thrombolytic treatment. Biomed Res Int 2013:265171. https://doi.org/10.1155/2013/265171
Valdueza JM, Balzer JO, Villringer A et al (1997) Changes in blood flow velocity and diameter of the middle cerebral artery during hyperventilation: assessment with MR and transcranial Doppler sonography. AJNR Am J Neuroradiol 18:1929–1934
Valdueza JM, Draganski B, Hoffmann O et al (1999) Analysis of CO2 vasomotor reactivity and vessel diameter changes by simultaneous venous and arterial Doppler recordings. Stroke 30:81–86. https://doi.org/10.1161/01.str.30.1.81
Viticchi G, Falsetti L, Potente E et al (2021) Impact of carotid stenosis on cerebral hemodynamic failure and cognitive impairment progression: a narrative review. Ann Transl Med 9:1209. https://doi.org/10.21037/atm-20-7226
Wolf ME (2015) Functional TCD: regulation of cerebral hemodynamics–cerebral autoregulation, vasomotor reactivity, and neurovascular coupling. Front Neurol Neurosci 36:40–56. https://doi.org/10.1159/000366236
Yemisci M, Gursoy-Ozdemir Y, Vural A et al (2009) Pericyte contraction induced by oxidative-nitrative stress impairs capillary reflow despite successful opening of an occluded cerebral artery. Nat Med 15:1031–1037. https://doi.org/10.1038/nm.2022
Zavoreo I, Kes VB, Morović S et al (2010) Breath holding index in detection of early cognitive decline. J Neurol Sci 299:116–119. https://doi.org/10.1016/j.jns.2010.08.062
Zavoreo I, Bašić Kes V, Lisak M, Maršić N, Ciliga D, TroštBobić T (2013) Cognitive decline and cerebral vasoreactivity in asymptomatic patients with severe internal carotid artery stenosis. Acta Neurol Belg 113(4):453–458. https://doi.org/10.1007/s13760-013-0196-4
Zinn S, Bosworth HB, Hoenig HM, Swartzwelder HS (2007) Executive function deficits in acute stroke. Arch Phys Med Rehabil 88:173–180. https://doi.org/10.1016/j.apmr.2006.11.015
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
MS and GS conceived the study. MS performed the literature search. EB and MS drafted the first version of the manuscript. All authors critically revised the work, drafted and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sforza, M., Bianchini, E., Alivernini, D. et al. The impact of cerebral vasomotor reactivity on cerebrovascular diseases and cognitive impairment. J Neural Transm 129, 1321–1330 (2022). https://doi.org/10.1007/s00702-022-02546-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-022-02546-w