Abstract
This is the second of two papers which critically examine the relationship between the 1918/19 influenza pandemic and encephalitis lethargica (EL). The role of influenza in the etiology of EL was vigorously debated until 1924. It is notable, however, that the unitarian camp were largely reactive in their argumentation; while the influenza skeptics provided detail descriptions of EL and the features they argued to be unique or at least unusual, influenza supporters focused on sequentially refuting the evidence of their opponents. The impression which emerges from this debate is that the individual features identified by the skeptics were not absolutely pathognomic for EL, but, on the other hand, their combination in one disorder had not previously been described for any other disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Was the neuropathology of EL consistent with influenza infection?
The adage that the pathologist has the final word regarding diagnosis is particularly pertinent when considering neurological disease. The neuropathology of encephalitis lethargica (EL) cannot be described in detail here, nor can the 1920s debate regarding what constituted “encephalitis” be pursued (review: Spatz 1930): discussion must be limited to features which distinguished EL from influenza encephalitis.
Economo cited four features of EL which distinguished its neuropathology from that of influenza encephalitis: neuronophagia; its preference for the grey matter of the brain; its non-hemorrhagic character; and the predominantly lymphocytic nature of the inflammation process. Economo’s early reports were largely corroborated by subsequent investigators, their findings encapsulated by the Swiss neuropathologist Tobler’s comprehensive title of his 1920 paper: “acute, focal, disseminated, non-purulent, principally lymphocytic, infectious-toxic, epidemic polioencephalomyelitis”. Jordan summarized the situation succinctly in 1927:
While the clinical symptoms are varied and a number of different types of the disease have been distinguished by some observers …, the pathological lesions present a close agreement in cases studied in Austria, France, England, and the United States, and are sufficient in the opinion of most writers to establish lethargic or epidemic encephalitis as a distinct disease … Flexner (1924) [(1863–1946); leading American bacteriologist, foundation director of the Rockefeller Institute for Medical Research in New York], indeed, regards the current pandemic of epidemic encephalitis as the first appearance of this disease, and does not identify the malady with any of the earlier outbreaks of brain disease known in epidemic history (Jordan 1927).
The following features were consistently reported in examinations of the EL brain:
-
non-hemorrhagic acute inflammation of the grey matter with largely negative macroscopic findings;
-
superficial congestion, occasional meningeal hemorrhages;
-
especial involvement of substantia nigra, locus ceruleus and other brainstem areas; no Lewy bodies, but widespread neurofibrillary tangles (no plaques);
-
lymphocytic infiltration in basal ganglia, midbrain, pons, Sylvian aqueduct;
-
minor to major neuronophagia;
-
minor involvement of cerebral cortex and cerebellum.
(representative reports: Marinesco 1918; Bassoe and Hassin 1919; Trétiakoff 1919; Stern 1919/20; Buzzard and Greenfield 1919; Marie and Trétiakoff 1920; Siegmund 1920; Boyd 1920/21; Kuczynski and Wolff 1921; Klarfeld 1922; Agostini 1925; Greenfield 1927; Lucksch 1928; Rostan 1928; Pette 1932; Hassler 1938; Klaue 1940; Greenfield and Bosanquet 1953; reviewed: von Economo 1929a; Rietti 1935; Stern 1936; see also Bernheimer et al. 1973).
The neuropathology of EL was exhaustively investigated from Economo’s first publication on the disorder in 1917 until the 1930s, with studies undertaken by the leading neuroanatomists and neuropathologists of the time, as well as by numerous medical students completing doctoral theses. The vast majority of these studies recognized similarities with other neurological disorders—particularly viral poliomyelitis, rabies, Borna disease and typhus—but expressly not with influenza encephalitis. The latter had itself been intensively studied in the course and wake of the late nineteenth century influenza pandemic, and constituted one of the two best described forms of encephalitis: Strümpell-Leichtenstern encephalitis and Wernicke’s encephalitis.
Strümpell-Leichtenstern encephalitis and EL
Strümpell-Leichtenstern or acute hemorrhagic encephalitis (SLE) was first described in detail during the 1890s influenza epidemic in Germany by Ernst von Strümpell (1853–1925) and Otto Leichtenstern (1845–1900) (von Strümpell 1890; Leichtenstern 1892). Each author noted that it was most commonly but not exclusively associated with influenza. Children and adolescents were at greatest risk for the disorder, which usually manifested itself a few days or weeks into the recovery from influenza itself. The clinical symptoms included somnolence and stupor, the possibility of convulsive seizures and varying degrees of paralysis, as well as oculomotor palsies in some patients. Recovery could be complete, but enduring motor deficits, mostly hemiplegias, and psychotic sequelae were possible. It should be noted, however, that it was not frequently seen even during the 1890s pandemic, and rarely otherwise: further cases were reported irregularly until the First World War, including those of Virchow and Senator (1891) and Fürbringer (1892); Koenigsdorf (1892); Bücklers (1892) and Schmidt (1892). Hermann Oppenheim and Richard Cassirer, who published the standard monograph on encephalitis in 1907, regarded influenza as a common cause of encephalitis, and believed the prognosis for recovery was generally good. Nevertheless, the number of reported cases was low, and even the association with influenza was more circumstantial than circumspect (review: Puin 1957).
Differences between the neuropathology of EL and influenza encephalitis became clearer with the accretion of knowledge of the EL brain throughout the 1920s. But as early as 1921, Schröder and Pophal (Psychiatric Clinic, Greifswald) had collated the published neuropathological literature on influenza encephalitis during the 1890s epidemic (13 cases in all), and concluded that “[the] acceptance of an identity between lethargica and influenza encephalitis could arise only from insufficient consideration of the fundamental anatomical difference between the two processes.” They emphasized that the neuropathology of EL, despite individual variations, was better defined and more consistent between cases than SLE; the two neuropathological pictures could hardly be more divergent, and were without doubt qualitatively distinct processes.
That an SLE brain had sustained major injury was apparent even to the untrained, naked eye. The hallmarks of influenza encephalitis were massive pial infiltration and extensive hemorrhage throughout the brain, focal hemorrhagic malacia, particularly as the result of thromboses of the major cerebral sinuses. Single or multiple focal white matter hemorrhages (“flea-bite” hemorrhages) were characteristic, the confluence of which produced areas of marked hemorrhage ranging in size from “cherry pip to pigeon egg”, between which “the tissue was more or less softened, and colored grey to grey-red”; secondary hemorrhages could occur in these areas of softening (Leichtenstern 1912, p 159). Grey matter hemorrhages were largely limited to the cerebral cortex and central ganglia, and were rarely described in brainstem or cerebellum. Purpura cerebri (brain purpura) was often described: macroscopically recognizable collections of diapedetic “ring hemorrhages”, each consisting of a broad external ring and pale inner ring centred on a distinct central point (Schmidt 1905; Kirschbaum 1920; Siegmund 1921); similar phenomena were also seen in a number of other hemorrhagic encephalitides, as well as in connection with various intoxications. SLE cases also presented purulent aspects, including meningitis and abscess formation.
Influenza encephalitis was even less common in the 1918/19 pandemic than in 1890, purpura cerebri especially so (Jorge 1920; Kuczynski and Wolff 1921). In a retrospective assessment of 285 influenza autopsies in Kiel, the doctoral student Juhl (1921) identified hemorrhagic encephalitis in 26 cases, with lesions randomly distributed throughout the brain, but most prominent in the white matter. Encephalitis and encephalomyelitis in influenza patients were not associated with any particular brain region, nor were the observed changes specific for influenza, resembling those of other post-infectious encephalitides.
The macroscopic examination of EL cases, in contrast, generally revealed no more than minor infiltration. It was only at the microscopic level that small, localized areas of glial and mesodermal proliferation were evident, together with lymphocytic infiltration around blood vessels. Ring bleeding was sometimes seen in EL; purpura cerebri, on the other hand, never. The histological picture in fresh cases was dominated by extreme congestion of the cerebral tissue, perivascular bleeding and adventitial infiltrates around small veins, precapillary vessels and capillaries. The focal damage exhibited preference for the grey substance of certain brain regions (the peri-aqueductal grey, tegmentum, hypothalamus, distal striatum and pallidum). Particularly liable to catastrophic damage was the substantia nigra, the hallmark of EL being its almost total cellular and pigment loss and replacement by a pale glial scar. Involvement of the extended mark and grey substance of the spinal cord, particularly the anterior horns, was more common in EL (although untypical) than in influenza encephalitis. The cortex was usually spared in EL. Elsewhere coarse, dispersed foci of ring-shaped expression were observed, but no major hemorrhagic foci or thrombosis development. The white matter was generally spared in EL, and in the cases where white matter neuropathology was described it was mostly those cases where the fulminant course had ended promptly in death. The suggestion that more expansive white matter lesions in EL may have healed to some extent by the time a case came to autopsy is rendered less significant by the fact that neuropathologists were able to distinguish even acutely fatal cases of EL from influenza encephalitis. Finally, influenza encephalitis was frequently accompanied by meningeal hyperemia or edema; evidence for meningeal inflammation or infiltration was usually more restricted in EL, and was interpreted as indicative of irritation rather than inflammation, and sufficient to explain the meningeal symptoms sometimes observed early in its course (Stern 1919/20; Tobler 1920; Siegmund 1920; von Economo 1929a, p 102f).
Two years after his first EL cases, Economo reported to the Viennese Society for Neurology and Psychiatry his histological examination of cases of post-influenzal encephalitis and myelitis (von Economo 1919), and he was adamant that the neuropathology was quite distinct from that of EL. Ten years later he summarized his findings thus:
… influenza occasionally causes cerebral manifestations which are based on a genuine influenzal encephalitis. This influenza encephalitis, however, differs clinically and patho-anatomically quite considerably from encephalitis Iethargica. … Patho-anatomically influenza encephalitis does not consist of multiple microscopic foci, as in encephalitis lethargica, but large hemorrhagic foci, necrosis of vascular walls, and even the building of abscesses as the result of metastatic coccal embolisms which destroy larger sections of white medullary tissue of the cerebrum and other parts of the nervous system (von Economo 1929b).
The contrast between SLE could hardly be starker. Strümpell (1920) himself negated the question of the identity of the two encephalitis forms; even those pathologists who noted the similarity of influenza encephalitis in the 1890s and 1918/19 pandemics recognized that it differed fundamentally from EL (reviewed: Juhl 1921).
It was ultimately not so much the nature of the histological features which differentiated EL from influenza, but rather their localization. The Cologne neuropathologist Siegmund was of similar mind, having himself examined 19 cases in a particularly meticulous study:
The brain changes were generally in the brainstem [in only two cases were the cerebral hemispheres, especially the cortex, affected, a finding foreshadowed by the clinical symptoms in these cases], from the medulla oblongata up to the nucleus lentiformis, with a preference for subependymal tissue. … Taken together, the findings are, in principle, not different from changes in non-purulent inflammations of the cerebral substance of different etiology, such as lyssa [rabies], post-meningococcal encephalitis, Strümpell’s disease, tropical sleeping sickness, poliomyelitis acuta superior and sporadic encephalitis. Our cases are, however, certainly different anatomically from the encephalitis hemorrhagica of Wernicke. They also have little in common with the hemorrhagic encephalitis of Leichtenstern … The current encephalitis epidemic is distinguished not through fundamental anatomical differences when compared with cerebral inflammations of other etiology, but rather the characteristic and consistent localization of the changes in the central grey, on the floor of the third and fourth ventricles, and around the aqueduct (Siegmund 1920).
Double infection with influenza and EL may have occurred, resulting in instances where the neuropathology reflected contributions by both disease processes. The Dutch neuropathologists Baumann and de Leeuw (1933) nevertheless concluded: “Whoever has studied the pathological anatomy of both (EL and SLE) can hardly imagine that the two could ever offer occasion for error in decisions of diagnosis intra vitam” (see also Groß 1923).
“Comatose form of influenza” and EL
Leichtenstern’s somnolent form of influenza encephalitis was exceedingly rare in the 1890s pandemic, and no neuropathological data was published. Comparison with that of EL was correspondingly not possible.
Wernicke’s encephalitis and EL
Parallels were noted between EL and polioencephalitis haemorrhagica superior, more commonly known as Wernicke’s encephalitis (from the late 1920s: encephalopathy), which at this time was not exclusively associated with alcoholism. Somnolence and oculomotor palsies were also prominent in this form, especially in non-alcoholic patients, and the midbrain was typically involved, although the neuropathology could be quite diffuse. The features which particularly distinguished EL from Wernicke’s encephalitis were the pathognonomic involvement of the substantia nigra in EL, and the more extensive hemorrhagic damage in Wernicke’s encephalitis (reviewed: Gutzwiller 1924).
Poliomyelitis and EL
There was also some suggestion that EL might be linked with poliomyelitis, then usually referred to as “childhood paralysis” or “Heine-Medin disease”, and particularly with the form designated Strümpell’s disease (acute polioencephalomyelitis in children; Strümpell 1885) (see, for instance, Gerlach 1920). The predilection of both disorders for the grey matter linked the two disorders, with EL perhaps representing an atypically anterior localization of the poliomyelitis “virus” (Häuptli 1921). The absence of spinal lesions in most cases of EL, however, reduced the credibility of this thesis, as did the fact that annual and seasonal case numbers of EL and poliomyelitis/polioencephalitis were not correlated. Harold Amoss (at Flexner’s Rockefeller Institute) also provided in 1921 immunological evidence for the discreteness of the two disorders. On the other hand, Wickmann included in his authoritative account of the various clinical forms of poliomyelitis a variation, “bulbar or pontine poliomyelitis”, which was referred to lesions in the brainstem and mesencephalon (Wickman 1913, pp 62–68; see also Oppenheim 1899a, b; Bremer 1910; Batten 1916). It is possible that this unusual form, which most German authors noted had never been described in Germany, represented pre-1917 EL cases (see also Bozzolo 1900; Hall 1918).
Neuropathological evidence linking EL with influenza
The unitarian hypothesis was not completely devoid of neuropathological support. The German neuropathologist Franz Lucksch (Prague), in a comprehensive review in English of the German language literature, noted the many quantitative differences of the 1918/19 influenza pandemic from earlier epidemics:
The most striking phenomenon of the most recent [influenza] epidemic—besides the great mortality—is the frequent and grave participation of the central nervous system in the disease. Among these nervous changes, the chronic or so-called residual phenomena apparently have no predecessors of equal significance and frequency in former epidemics, at least not in the striking and oft repeated picture of parkinsonism and of the vegetative disturbances associated with it (Lucksch 1928).
Lucksch regarded nervous changes as characteristic of the 1918/19 pandemic because he saw EL as distinct from SLE, but nonetheless as another form of influenza encephalitis:
The facts in the history of influenza force one to assume a chronologic connection between influenza and the syndrome which has been called encephalitis. … A transition between the lesions appears histologically possible. The etiologic and experimental research on encephalitis has not revealed a separate causative agent. The most probable opinion attributed the syndrome called epidemic encephalitis to the action of poisons that appear in the body in influenza (Lucksch 1928).
The pathologist Rudolf Jaffé (1920; Berlin) recognized that most EL and influenza encephalitis cases could be confidently distinguished from one another, but argued that they nonetheless represented opposite ends of a spectrum of pathology, whereby “on occasion the one form, on others the alternative form dominates to a greater extent, or even exclusively, the clinical picture.” Kuczynski and Wolff (1921), in their comprehensive review of the pathology and pathogenesis of influenza, offered the interpretation that although both forms were etiologically linked with influenza, the two clinical pictures reflected divergent underlying processes, differences which would ultimately be clarified only in the framework of a general treatment of the “encephalitis problem”.
In 1931 Meerloo (1931; Rotterdam Psychiatric Hospital, Maasoord) described a toxic influenza encephalopathy which particularly injured the brainstem and vegetative centres, albeit in the most cases transiently. He argued on this basis for the identity of the causative agent in influenza and EL, but conceded that this conclusion presupposed “a particular susceptibility and primitive psyche with an easily injured mesencephalon. … the difference between a reversible intoxication and an inflammation with persistent consequences is often merely a question of degree determined by the vulnerability of the tissue and the virulence of the toxin involved.” Meerloo thus proposed that individual constitutional differences determined whether one recovered without major repercussion from CNS influenza infection or succumbed to chronic EL; Bernhardt and Simons had suggested this possibility as early as 1919. It is notable, however, that Meerloo did not report that he had actually encountered an EL case in his patient collective.
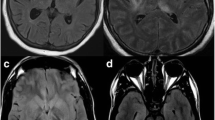
Status of influenza encephalitis after 1930
In 1919 it had been plausible to assert that “[postinfluenzal] diseases of the cerebrospinal axis are of common occurrence” (Mayer 1919) despite dissenting voices (for instance, Eichhorst 1919). But the experience of subsequent influenza pandemics and the employment of increasingly refined pathological techniques led some to comment that influenzal encephalitis was quite rare (Crome 1954), while others cast doubt on the existence of influenza encephalitides altogether (Aronovich 1934; Stuart-Harris 1953, p 23). “Influenza-associated acute encephalitis/encephalopathy” is now defined as “an uncommon neurological syndrome of childhood and adolescence that typically presents during the early phase of influenza infection”; post-influenza encephalopathy presents after the resolution of respiratory symptoms, but typically within 3 weeks (Toovey 2008). An Austrian study of both disorders found that the first was frequently associated with metabolic disturbances; post-influenzal encephalopathy, on the other hand, “seemed to be a less distinct clinical entity”, with the identification of other viruses in patient CSF suggesting that it has a number of different etiologies (Steininger et al. 2003). Further, post-EL descriptions of neuropathology associated with influenza, the most recent employing advanced imaging techniques in the living brain, have not found the characteristic mesencephalic neuropathology of EL (Davison et al. 2003). SLE is now rarely reported, and influenza is not regarded as a major cause of encephalitis. The objection that the 1918/19 influenza was somehow atypical—that its neuropathological footprint differed from that of influenza both before and after the EL pandemic—simply begs the question.
Only a brief overview of the neuropathology of EL has been possible here, but it is nevertheless clear that EL as a polioencephalitis with a consistent and specific localization was quite distinct from the non-specific leukencephalitis associated with influenza. This is one of the strongest indicators of the separateness of the two disorders.
The 1920s debate on the link between EL and influenza
Early in the EL epidemic the Bonn physician Hirsch (1920) posed the question “What at the moment is not encephalitis lethargica?” Neither clinical presentation nor neuropathology convinced him that EL was anything genuinely new; at the same time, however, he reminded readers that the diagnosis “influenza” was often applied without a great deal of consideration, a view expressed before the influenza pandemic by Jelliffe (1902): “One cannot help suspecting that … influenza, like charity, covereth a multitude of sins of careless diagnosis”.
It was in this atmosphere that a number of German doctoral dissertations addressed the question of the relationship between EL and influenza. For example, Werner Gottstein (1894–1959; Berlin) addressed comprehensively the question of whether “the etiology, clinical presentation and pathological anatomy distinguish EL from other disorders”, and answered the question in the negative. He concluded that Economo’s criteria were not as specific as the Austrian neuropathologist claimed, and Gottstein identified overlaps not only between EL and influenza encephalitis, but also between EL and other encephalitides, including polioencephalitis. The etiological link which he proposed was built on a number of speculative premises, including a view of influenza as an inconsistent disease elicited by shifting combinations of infectious agents. In particular, the isolation of similar streptococci from both the respiratory tract and the brainstem was interpreted as favoring the unitarian etiology hypothesis of influenza and EL, as was the isolation of Pfeiffer’s bacillus from the body fluids of EL patients. Nevertheless, Gottstein conceded that it was far from clear whether every EL case commenced with genuine influenza. He concluded that the clinical picture of EL is sufficiently distinct to justify it as a diagnosis, but that it shared its etiology with influenza, for which reason he pleaded for the replacement of “encephalitis lethargica” by the term Grippeenzephalitis (Gottstein 1921, 1922).
Julius Emil Kayser-Petersen (1886–1954; Frankfurt am Main), later a leading figure in tuberculosis research, forwarded questionnaires in 1920 to all German university clinics and major hospitals seeking information regarding the appearance of influenza and EL in each district during the epidemics of 1918/19 and 1919/20; he also supplemented this data with reports published in medical journals. The result was an intriguing picture of the epidemiology of EL in the German Reich, including identification of apparent foci of infection from which the disease spread in 1919 and 1920, as well as of areas and cities in central Germany where curiously few or even no cases of EL had been reported. But the author nevertheless concluded that an etiological link between EL and influenza existed, purely on the basis that EL occurred only during or following influenza outbreaks. The sketchy numerical data presented in the paper, however, were national figures, whereas his epidemiological data for individual districts (for example, the gradual spread in 1919/20 from seemingly unrelated foci in the Ruhr valley, Cologne and Danzig) suggested that a more local approach might have yielded more useful insights (Kayser-Petersen 1921, 1923; Kayser-Petersen and Schwab 1923).
Christian Faßbender (Berlin) compiled a report based on official statistics which examined the relationship between influenza and EL in Prussia (the largest German state, stretching from the Baltic to the Rhine). He reviewed the positions of various authors, and reached the conclusion that “a close connection between influenza and encephalitis lethargica, under which name we collect the various brain inflammations we have observed in recent years, appears indubitable to me.” He admitted, however, that the etiology and epidemiology of influenza had become more complicated in recent years, so that the nature of this relationship was obscure (Faßbender, 1921).
Faßbender also discussed in detail the views of the Swedish pathologist Einar Sjövall (1879–1964; Lund). The Scandinavians, he noted, recognized epidemics of “sleeping disease” between influenza pandemic periods, and therefore tended to regard the two disorders as distinct. Sjövall suspected that a relationship between the two existed, but also that this relationship owed more to an “epidemic constitution”—the proneness of communities to succumb at a particular time point to epidemic disease—than to a shared pathogenic agent, and this view was partly adopted by Faßbender.
Evidence against the unitary hypothesis
Many authors stalwartly employed terms such as “post-influenza encephalitis”, “encephalitis comatosa” and “encephalitis post gripposa” throughout the EL period (including Heiman 1919; Mayer 1919; Re 1919; Jaksch-Wartenhorst 1922, 1923; Fleischmann 1923; Herrmann and Wotke 1925). But these were more than matched by opposing reports, many of which were based on significantly greater case numbers. The official report of the British Ministry of Health, for instance, concluded that no direct connection between the two could be found (Ministry of Health 1922). The 1919/20 report of the United States Public Health Service identified a number of epidemiological and clinical features which distinguished EL from both influenza and poliomyelitis; further, a history of influenza had been recorded in only 56 of 122 EL cases (Smith 1921). Happ and Mason (1921), reviewing 81 cases at the Johns Hopkins Hospital, similarly saw no evidence of a relationship, or indeed of the contagiousness of EL. Interestingly, not a single case of EL was noted in the long list of secondary diagnoses associated with the 734,397 primary diagnoses of influenza in the United States Army during the First World War (Hall 1928).
EL was increasingly regarded as a disorder in its own right as experience with the disease increased. This change in attitude is especially evident in the opinions of those who concerned themselves with EL over an extended period. Felix Stern (1884–1941), for example, was regarded by many as the leading EL expert in the German-speaking world. In 1923 he published a detailed discussion of the etiology question which was interpreted by many as a cautious endorsement of the central role of influenza in EL, either as the primary infectious agent or as an activator of the actual pathogen. This view had changed markedly by 1936, as evidenced by his final major scientific contribution, his chapter on EL in the Handbuch der Neurologie (published between the ejection of the highly respected Jewish Nervenarzt from Göttingen and his suicide in Berlin). Here he summarized his position succinctly: “that what has previously described as influenza encephalitis … has neither clinically nor anatomically any connection with epidemic encephalitis can now be regarded as definitive” (Stern 1936). The etiology of influenza was being debated at this time more heatedly than ever, with several new bacterial and filterable candidates in discussion. Stern saw no point, therefore, in speculating about the specific etiology, but was convinced that the epidemiological and pathological evidence contributed by Economo, himself and others was sufficient to establish the separateness of the two disorders, and that the relationship, if any, was quite complex and far from obligate. Influenza might act as an agent provocateur, according to Stern, but it was not specific; measles (Capaldo 1932), typhus (Nagtegaal 1927; Rabinowitsch 1928) and malaria (Wilson 1921) could also elicit EL-like symptoms. Indeed, the similarity of EL and a number of other encephalitides with no connection to influenza—Japanese encephalitis, poliomyelitis and post-vaccinal encephalitis—was indirect evidence for the frailty of the unitary EL/influenza hypothesis (Stern 1936). It might be added that a number of other conditions which appeared to be aberrant forms of EL—epidemic hiccough, epidemic vertigo, certain forms of encephalomyelitis—exhibited little relationship with influenza (Engel 1919; Anonymus 1925; Neel 1925).
Julius Hurst (Veterans’ Administration) published a detailed analysis of United States data in 1934, and by now the evidence against the involvement of influenza in EL was overwhelming. Hurst employed detailed data from South Carolina, partly because the influenza burden had been greater here than in any other US state in the period 1925–1929, as well as selected summaries of data from Great Britain and Canada, all of which led him to the unambiguous conclusion:
The evidence fails in any particular to indicate a common entity for influenza and epidemic encephalitis. It fails to indicate that the presence of influenza predisposes to encephalitis, either in the mass or in the individual (Hurst 1934).
As the influenza pandemic receded into the past, attempts to implicate it in EL were less confident. A further reason for the decline in popularity of the influenza hypothesis was that research into the etiology of EL had long developed along different lines. Attempts to elicit EL in experimental animals by transfer of material from influenza cases achieved nothing, whereas investigation of herpes virus and of streptococci and staphylococci appeared to offer greater promise. These alternative research directions ultimately ran to sand, but were not in vain, despite the evolution of somewhat rigid camps supporting one or other infectious candidate, as will be described elsewhere. When the influenza virus was discovered at the end of the 1920s, there was no evidence that it had anything to do with EL, and interest in pursuing the question had in any case waned as the number of notified acute EL cases began to dwindle.
End of the debate?
In the discussion of EL in his exhaustive review of the 1918/19 influenza pandemic, American bacteriologist Edwin Jordan listed four possibilities regarding the relationship between the two infectious diseases (Jordan 1927):
-
1.
Epidemic encephalitis is the sequel of a certain—though small—proportion of influenza cases, and is due perhaps to the cerebral localization of the influenza virus.
-
2.
It is the manifestation of a peculiar modification of the influenza virus.
-
3.
An attack of influenza weakens and predisposes certain individuals to epidemic encephalitis, but the virus of the latter disease is distinct and independent.
-
4.
… [the] concurrence of the two maladies is accidental and without essential causal relation.
Jordan concluded that there was no compelling evidence to support a causal link of any kind between the two infections, certainly none that did not require acceptance of a conjectured but hitherto undemonstrated “neurotropic influenza virus”. Heinrich Pette (1887–1964; Hamburg), one of the leading German investigators of the neuropathology of viral disease, reviewed the situation fifteen later and similarly asserted that the “original viewpoint which held the influenza “virus” for the instigator of epidemic encephalitis could be rejected as untenable only a few years after the hypothesis had been advanced” (Pette 1942). Twenty years later, the English virologist Charles Stuart-Harris (1909–1996), one of the leading influenza investigators, was also clear about the lack of a connection between the two:
The older literature on influenza contains many references to neurological and psychological disturbances during or after the disease. It is most likely that many of these bear no direct relationship to the influenza itself. This almost certainly applies to the numerous cases of encephalitis seen after the 1918 epidemic of influenza which culminated in the 1920–21 epidemic of encephalitis lethargica … sporadic encephalitis is known to occur in England and Wales every year whether or not there is an influenza epidemic (Stuart-Harris 1965, p 52f).
Discussion
Felix Stern commented that more was to be learned from identifying and studying that which was common to EL cases than from becoming frustrated by its variability. The apparent clinical heterogeneity of EL proved to be reducible to a small number of major forms characterized by particular constellations of symptoms traceable to focal neurological injuries, primarily in the brainstem (review: Vilensky and Gilman 2006). Attempts to attribute these symptoms to neurological influenza achieved little, for a number of reasons.
First, many EL symptoms could indeed be observed in other maladies: the oculomotor symptoms evinced comparisons, for example, with similar signs in diphtheria, botulism—and influenza. Disparate causes can elicit similar symptoms, so that similarities in clinical presentation cannot be assumed to indicate a common etiology.
Second, many comparisons of the symptoms of EL and influenza have not adequately recognized that common or characteristic EL symptoms were being equated with atypical phenomena in influenza and influenza encephalitis. Similarly, it appears that some authors, on the basis that the 1889–1892 influenza was associated with certain nervous phenomena, assume that all nervous symptoms may be a priori attributed to influenza.
Third, the hallmark of EL neuropathology was the destruction of the substantia nigra. Since the 1930s a panoply of infectious and toxic agents have been identified which exhibit a certain “preference” for the black nucleus (Casals et al. 1998), including the influenza virus (Mihara et al. 2001; Takahashi and Yamada 2001; Shinya et al. 2005). The evidence discussed in this paper does not permit, however, specifically ascribing EL to any one of these noxae, least of all influenza.
Finally, EL was ultimately defined not by somnolence or oculomotor dysfunction or adolescent psychosis, or even by parkinsonism: it was defined by the systematic conjunction of these and other phenomena in a structured syndrome. And it was demarcated from other disorders precisely by the fact that this syndrome was unique.
Why the influenza hypothesis was revived
There is more support for the view that EL was not a specific neurological response to influenza than for the converse. Why then has the influenza etiology of EL proved so popular? First, it must be noted that it gained broad acceptance only after EL had ceased being an epidemic disease. Although the research efforts devoted to identifying the pathogen could hardly have been more intense, the primary cause of EL, in contrast to many other diseases investigated in the first third of the twentieth century, defied all attempts at identification. But history abhors a vacuum, especially where it concerns explanations for unusual events. Despite having lost most of its support by 1930, the influenza hypothesis nonetheless provided a convenient explanation when looking back at EL from the distance of a half century.
Further, as events recede into the past, accounts of the complicated reality in which they are embedded are gradually simplified, linear narratives and straightforward explanations are preferred to uncertainty and complicated interpretations. The rise of influenza and EL occurred at approximately the same time; “influenza-like” symptoms were sometimes reported in EL; influenza was known to be capable of eliciting a broad range of clinical responses, including dire neurological consequences. Two puzzling infectious diseases at the same time and the same place thus become one, particularly as the more mysterious of the pair is now little more than a historical curiosity, a “vanished disease”. Post (or even apud) hoc, ergo propter hoc: the attempt to find a critical role for influenza in EL is ultimately grounded in the approximately coincident appearance of the two diseases in 1917–1919.
Influenza as agent provocateur in EL
But does the evidence discussed in this paper exclude entirely a role for the influenza “virus” in EL? Many analysts who conceded that evidence for a direct causal link was not conclusive—particularly during the 1920s, when the infectious agent in influenza itself was not known—nevertheless opined that the temporal overlap between the two epidemics could not be mere coincidence. On the basis of the argument that EL-like phenomena were historically associated with “influenza” epidemics, Economo himself commented that “a certain epidemiological link with influenza can be ascertained, with a probability approaching certainty, and this relationship appears at times to even be able to exert a decisive influence upon the clinical picture, as shown by the severe toxicity of the hyperkinetic forms of EL during influenza epidemics” (von Economo 1929a, p 146).
It might also be argued that influenza weakened those it infected and thereby paved the way for infection with EL, playing a crucial if not primary role in the latter disease. As seductive as this argument sounds, the earliest clusters of probable EL cases (France, 1915) preceded the arrival of pandemic influenza by 2 years. Even one to subscribe to the theory that the 1918/19 influenza virus had been present in France as early as 1915, albeit in less virulent form, there is still the problem that the scales and timetables of the influenza and EL epidemics exhibited little correlation. The argument that the two disorders might be related in this manner is ultimately as dubious as the argument aired in the aftermath of the influenza pandemic that the physical and psychological toll of the World War had sufficiently reduced physiological resistance to infection to a degree which transformed influenza from an irritation to a scourge (Auerbach 1922). Further, it only changes the etiological equation from “EL = infection with pathogen X” to the equally unresolved “EL = infection with influenza plus pathogen X”.
The diagnosis issue in influenza
There were probably cases where the two disorders were confused by those not familiar with both. An EL patient who died in the middle of the influenza epidemic might well be classified without further investigation as an influenza death, despite the absence of catarrhal signs, and there would have been little call to conduct an autopsy to determine neuropathological damage. Marcus (1920), without referring to EL, noted that nervous forms of influenza (but not influenza encephalitis) had been observed in Sweden during the 1918/19 epidemic, and, quite interestingly, that these cases, at least in retrospect suggestive of EL, were concentrated in geographical and temporal clusters. On the other hand, Jordan observed that “it is possible that an attack of encephalitis may have been preceded by an obscure or mild form of influenza which went unrecognised” (Jordan 1927).
The problem of influenza diagnosis had already been understood during the 1890s pandemic. The Chicago neurologist Church had identified more than 400 papers concerning its neurological effects in the English, French and German language literature, and advised caution in attributing too much to influenza, presaging the 1965 observation by Stuart-Harris cited earlier in this paper:
it is well to remember that during an epidemic of this nature every departure from health is liable to be attributed by the laity, and even by medical practitioners, to the prevailing malady; that many instances of minor ailments have probably been erroneously called grippe, and. that a preceding attack of influenza is not a competent cause for every subsequent illness … Moreover, it is not unreasonable to suppose that grippe and other diseases may occur concomitantly without necessary intimate relation (Church 1891).
This lack of diagnostic security with respect to influenza further undermines attempts to link it with EL. But it is also possible that EL cases early in the epidemic were misdiagnosed as influenza, particularly before EL had been recognized as a clinical entity. Smith mentioned this possibility in his 1921 review of EL in the United States. The pre-eminent English neurologist Kinnier Wilson expressed guarded doubts about the relationship between influenza and encephalitis in his textbook Neurology:
[Influenza] may be the cause of encephalitis or encephalomyelitis, although uncertainty surrounding its diagnosis has hardly yet been dispelled; … a large number of nervous and mental syndromes were described in relation to the pandemic of 1918–19 … Yet the possible connexion of some of these cases with encephalitis of the lethargic type cannot be ignored, and raises questions extremely difficult to answer (Wilson 1954).
In 1924 the important Italian EL neuropathologist Corrado Da Fano (1879–1927) described an unusual “acute case of encephalitis presumably epidemic”. A 43-year-old man complained of headache, lapsed into unconsciousness and died in hospital 36 h later. Initial examination of the brain revealed SLE-like hemorrhages, but limited to remarkably few areas of the cortex; on closer examination, however, most proved to represent not genuine hemorrhages, but rather vascular dilatation. Histological examination revealed perivascular and parenchymatous infiltrations of extraordinary intensity in the upper medulla, in the pons, midbrain, optic thalamus and cerebral cortex, consisting principally of neutrophils, lymphocytes and macrophages, in the absence of true plasma cells. Focal, acute nerve cell degeneration, an active penetration of neutrophils into the cytoplasm of nerve cells and clasmatodendrosis (damage to grey matter astrocytes characterized by cytoplasmic distention and loss of dendritic processes) were observed in the same structures. Comparing the clinical and histopathological observations with those made by other investigators in both acute hemorrhagic encephalitis and EL, Da Fano concluded:
(1) that the present case was, probably, a somewhat atypical one of lethargic encephalitis; and (2) that some at least of the acute encephalitic forms of the so-called Strümpell-Leichtenstern type were, presumably, sporadic instances of the same malady (Da Fano 1924).
Da Fano explicitly indicated here the possibility that some EL cases might be misinterpreted as “influenza”, even at the neuropathological level.
Even in the 1920s, influenza was not sufficiently defined, clinically or pathologically, to allow diagnostic precision; serious influenza cases could be difficult to differentiate from tuberculosis or dengue (cf. Fiessinger and Janet 1920). Further “influenza” at the time of the EL epidemic cannot unambiguously be identified with “infection with the influenza virus” (Foley 2009). After the influenza virus had been identified, immunoreactivity to the virus was established as the principal diagnostic criterion for influenza. But in the first few decades after the identification of the influenza virus, it was found that, on this basis, a large proportion of “influenza” diagnoses had been erroneous. Reviewing studies in the Soviet Union, Zhdanov and Rutshteyn (1950) reported that the number of false influenza diagnoses in major Russian hospitals between 1934 and 1942 ranged from 22 to 46%, with 40% being typical. Among the most common “corrected” diagnoses were pneumonia, bronchitis, sinusitis and chronic rhinitis, “various sore throats”, pulmonary tuberculosis, typhus and malaria (see also Epshteyn 1944; Johnson and Mueller 2002).
The impartial investigator is thereby confronted by the possibility that not only is EL not a form of influenza encephalitis, but that an undetermined proportion of “influenza cases” may actually have been EL infections of varying severity. In this respect, the suggestion that EL contributed to the anomalous hump in the 1918 influenza mortality curve might be speculative, but nonetheless worthy of consideration. As discussed in Foley (2009), existing attempts to explain the W-shaped deaths versus age curve of the influenza pandemic have been less than totally satisfying. The superposition of the characteristic inverted V-shaped EL curve upon the normal U-shaped influenza curve would, on the other hand, provide an alternative explanation which concords with the data for both disorders, both before and subsequent to the influenza pandemic. The mortality associated with diagnosed EL varied according to time and place, but generally declined during the 1920s, suggesting that the relationship between pathogen and host changed markedly in a very short time.
If not influenza, what caused EL?
Two questions remain unresolved. The first is: If the influenza virus did not cause EL, what did? The evidence reviewed does not exclude the possibility that one of the pathogenetic components of the “complex virus” discussed in Foley (2009) might be involved; Alfred Reinhart, for example, proposed in 1922 a similar explanation for the Kiel EL epidemic. Nevertheless, evidence implicating the usual suspects in this regard—Pfeiffer’s bacillus, Micrococcus catarrhalis—has thus far not been forthcoming. There was some support from microbiological investigations undertaken at the time that either a filterable agent (virus? mycoplasma?) or a streptococcal species (or both) was involved; no candidate, however, received conclusive experimental or clinical support before the end of the EL epidemic.
This question cannot be further considered here. Maurizi’s 1989 “challenge to the naysayers”, the influenza hypothesis skeptics, was misplaced: one cannot retain a scientific hypothesis simply because it feels comfortable, when the weight of evidence indicates that it is inconsistent with the available data. Questioning the role of influenza in EL does not require that a replacement pathogen be nominated. It should simply provoke us to keep an open mind in the search for the real culprit. Is the etiology of EL even important? In a very practical sense, it is: without knowing what caused EL, we can make no informed predictions about whether it might return; without a clear idea of what EL was, we might not even recognize cases outside a major epidemic. Equally importantly, without knowing the pathogen, it is difficult to formulate a rational therapeutic strategy.
This leads to the second problem: What was “influenza”? Both the 1889–1892 and 1918/19 pandemics were regarded by those who experienced them as genuine “influenza”—as opposed to “seasonal catarrh”—but major differences between the courses and symptomatology of the two pandemics were nevertheless recognized. Both pandemics, on the other hand, were very different from more recent experiences of viral influenza (including the “American” or “swine influenza” of 2009). It is proposed that this is at least partially attributable to the fact that 1918/19 was not just a viral influenza pandemic, but rather a catastrophic “influenza plus” event, involving multiple infections, the nature of which varied across the globe. The most urgent consequence of this perspective is that genetic changes in the influenza virus alone do not determine the outcomes of future pandemics, but also the bacterial background against which this pandemic unfolds, the general health of the affected population, and the availability of effective antibiotic therapy.
Conclusion
The specific features which permitted the definition of EL as an infectious disorder distinct from influenza were:
-
Epidemiology: there was no clear temporal or geographical link between the rise and fall in incidence and impact of the two disorders.
-
Transmissibility: influenza was highly contagious, whereas transmission of EL within families or hospitals was rare.
-
Symptomatology: even in the acute phase, the clinical picture for the two disorders was quite divergent, and even unitarians differentiated between the two sets of symptoms. No single EL or post-EL symptom was entirely pathognomic for the disease, but their combination as a syndrome was unique.
-
Neuropathology: The overlap between the neuropathological features of influenza encephalitis (SLE and other forms) and those of EL was limited, both in extent (the changes in influenza were apparent to the naked eye) and specificity (influenza encephalitis lacked the uniformity and systematic distribution of EL lesions).
-
Disease process outcome: “It is, however, by its residua that epidemic encephalitis has separated itself most clearly from all other epidemic infections” (Hall 1924, p 39). It is not the acute phase phenomena of EL but rather the ineluctable, progressive psychiatric and neurological features of the chronic phase which render the disease enduringly interesting. Nothing similar has ever been described in more than a handful of influenza cases.
One might challenge any one of these lines of evidence, their combination nevertheless renders the nosological individuality of EL more likely than otherwise.
The data concerning the relationship between EL and influenza presented here has inevitably been selective, and such a compact synopsis of the relevant material must necessarily omit much that is both relevant and interesting, concentrating on that which was most typical for EL and influenza encephalitis. By providing a broad overview of the published material representing the general consensus established by detailed scientific investigation of EL during its heyday, however, I hope to have provided a platform for further critical discussion of the issues touched upon in these papers.
References
Agostini G (1925) Sull’anatomia patologica e sulla patogenesi dell’encefalite epidemica cronica. Ann Osp Psichiatr Perugia 19:3–103
Amoss HL (1921) Immunological distinctions of encephalitis and poliomyelitis. J Exp Med 33:187–192
Anonymus (1925) Epidemic hiccup. Br Med J 2:78–79
Apoнoвич ГД (1934) К xapaктepиcтикe пopaжeнии нepвнoй cиcтeмы пpи эпидeмичecкoм гpиппe. Coв Bpaч Гaз 16:1178–1188 (Aronovich GD (1934) K kharakteristike porazheniy nervnoy sistemy pri epidemicheskom grippe. Sov vrach gaz 16:1178–1188)
Auerbach S (1922) Ein Versuch zur Erklärung des epidemischen Auftretens der Encephalitis in den letzten Jahren. Dtsch Zschr Nerv enheilk 75:165–168
Bassoe P, Hassin GB (1919) A contribution to the histopathology of epidemic (“lethargic”) encephalitis. Arch Neurol Psychiatry 2:24–40
Batten FE (1916) Acute poliomyelitis. Brain 39:115–211
Baumann C, de Leeuw CH (1933) Encephalitis epidemica und Grippeencephalitis. Zschr ges Neurol Psychiat 143:403–426
Bernhardt G, Simons A (1919) Zur Encephalitis lethargica. Neurol Centralbl 38:705–715
Bernheimer H, Birkmayer W, Hornykiewicz O, Jellinger K, Seitelberger F (1973) Brain dopamine and the syndromes of Parkinson and Huntington. Clinical, morphological and neurochemical correlates. J Neurol Sci 20:415–455
Boyd W (1920/21) Epidemic encephalitis. A study of 75 cases, with 16 necropsies. Ann Med (Hagerstown) 1:195–221
Bozzolo C (1900) Polioencefaliti emorragiche acuta da influenza. Riv crit clin med (Firenze) 1:69–73
Bremer K (1910) The variability of the lesions in polioencephalomyelitis. Lancet 175:421
Bücklers (1892) Zur Kenntniss der acuten primären hämorrhagischen Encephalitis. Arch Psychiat Nervenkr 24:730–757
Buzzard EF, Greenfield JG (1919) Lethargic encephalitis; its sequelæ and morbid anatomy. Brain 42:305–338
Capaldo L (1932) Un caso di encefalite morbillosa con postumi parkinsoniani. Policlinico (Sez prat) 39:94–96
Casals J, Elizan TS, Yahr MD (1998) Postencephalitic parkinsonism: a review. J Neural Transm 105:645–676
Church A (1891) The nervous features and sequences of la grippe. Chicago Med Rec 1:418–426
Crome L (1954) Encephalitis during an epidemic of influenza. Mschr Psychiat Neurol 128:159–179
Da Fano C (1924) The histology of the central nervous system in an acute case of encephalitis presumably epidemic. J Pathol Bacteriol 27:11–26
Davison KL, Crowcroft NS, Ramsay ME, Brown DWG, Andrews NJ (2003) Viral encephalitis in England, 1989–1998: What did we miss? Emerg Infect Dis 9:234–240
Eichhorst H (1919) Hirnstörungen bei Influenza. Zschr Ärztl Fortbild (Jena) 16:489–493
Engel K (1919) [Über die zurzeit in Budapest aufgetretene Singultusepidemie]. Orv Hetil nr. 6 (abstract: Neurol Cbl 39 (1920):273–274)
Faßbender C (1921) Das epidemische Auftreten der Grippe und der Encephalitis lethargica in Preußen im Jahre 1920 und die gegenseitigen Beziehungen der beiden Krankheiten. Nach dem amtlichen Berichten bearbeitet (Veröffentlichungen aus dem Gebiete der Medizinalverwaltung. XIII. Band, 8. Heft (pp 565–602)). Richard Schoetz, Berlin
Fiessinger N, Janet H (1920) Erreurs de diagnostic avec l’encéphalite léthargique; 1° Hémorragie méningée; 2° Sarcomatose diffuse; 3° Granulie généralisée avec tuberculose cérébrale. Bull Mém Soc Méd Hôp Paris:1230–1236
Fleischmann S (1923) An epidemic of encephalitis gripposa. J Nerv Ment Dis 58:435–447
Flexner S (1924) Epidemic encephalitis. NY State Dept Health Quart 1 (nr. 3):91–97
Foley PB (2009) Encephalitis lethargica and influenza. I. The role of the influenza virus in the influenza pandemic of 1918/1919. J Neural Transm 116:143–150
Fürbringer (1892) Zur Kenntnis schwerer organischer Hirnleiden im Gefolge von Influenza. Dtsch Med Wschr 18:45–48
Gerlach KW (1920) Über Encephalitis lethargica im Kindesalter. Thesis, Jena (Neuenhahn, Jena)
Gottstein W (1922) Die Encephalitis lethargica. Ergebn Hyg Bakteriol Immunitätsforsch Exp Ther 5:394–474
Greenfield JG (1927) The pathology of epidemic encephalitis. J Ment Sci 73(575–581):736–738
Greenfield JG, Bosanquet FD (1953) The brain-stem lesions in Parkinsonism. J Neurol Neurosurg Psychiat 16:213–226
Groß W (1923) Über Encephalitis. Virchows Arch Pathol Anat Physiol 242:452–478
Gutzwiller K (1924) Polioencephalitis haemorrhagica superior acuta (Wernicke) und Encephalitis lethargica (epidemica). Eine vergleichende Studie. Thesis, Basel (Ammann, Lenzburg)
Hall GW (1918) Report of a case of poliomyelitis of the bulbar-spinal type presenting rather unusual eye symptoms. J Nerv Ment Dis 48:445–446
Hall AJ (1924) Epidemic encephalitis (encephalitis lethargica). John Wright, Bristol
Hall MW (1928) Inflammatory diseases of the respiratory tract (bronchitis; influenza; bronchopneumonia; lobar pneumonia). In: Siler JF (ed) Communicable and other diseases (Lynch, C Weed FW, McAfee L (eds) The Medical Department of the United States Army in the World War (The Official History Series), vol IX). U.S. Army Surgeon General’s Office, Washington, pp 61–169
Happ WM, Mason VR (1921) Epidemic encephalitis. A clinical study. Bull Johns Hopkins Hosp 32:137–159
Hassler R (1938) Zur Pathologie der Paralysis agitans und des postenzephalitischen Parkinsonismus. J Psychol Neurol (Leipzig) 48:387–476
Häuptli O (1921) Zur Histologie der Poliomyelitis acuta und der Encephalitis epidemica (lethargica). Dtsch Zschr Nervenheilk 71:1–44
Heiman H (1919) Postinfluenzal encephalitis lethargica. Am J Dis Child 18:83–87
Herrmann G, Wotke E (1925) Die Beeinflussung des Tremors bei Encephalopathia postgripposa durch Nicotin. Med Klin 21:1842–1844
Hirsch C (1920) Zur vergleichenden Pathologie der Enzephalitis nebst kritischen Bemerkungen zur Encephalitis lethargica (epidemica)-Diagnose. Berl Klin Wschr 57:605–607
Hurst JH (1934) The relationship of influenza and epidemic encephalitis. Med Bull Vet Adm 11:110–134
Jaffé R (1920) Pathologisch-anatomische Untersuchungen über die Encephalitis lethargica, mit besonderer Berücksichtigung ihrer Stellung to Grippe-Encephalitis. Med Klin 16:1005–1008
Jaksch-Wartenhorst E (1922) Über Encephalitis und Encephalopathia postgripposa. Münch Med Wschr 69:1033–1035
Jaksch-Wartenhorst R (1923) Zur Klinik der akuten und chronischen grippösen Encephalopathien. Acta Med Scand 58:557–584
Jelliffe SE (1902) Influenza and the nervous system. Phil Med J 10:1041–1044
Johnson NPAS, Mueller J (2002) Updating the accounts: global mortality of the 1918–1920 “Spanish” influenza pandemic. Bull Hist Med 76:105–115
Jordan EO (1927) Epidemic encephalitis and influenza. In: Epidemic influenza: a survey. American Medical Association, Chicago, pp 326–336
Jorge R (1920) L’encéphalite léthargique. Épidémiologie, nosologie, histoire. Bull Off int Hyg publ 12:1275–1325
Juhl D (1921) Beiträge zur pathologischen Anatomie der Grippe. Virchows Arch Pathol Anat Physiol 232:58–94
Kayser-Petersen JE (1921) Versuch einer Epidemiologie der epidemischen Enzephalitis (Vorläufige Mitt.). Münch Med Wschr 68:507–508
Kayser-Petersen JE (1923) Zur Geschichte der Gehirngrippe. Dtsch Zschr Nervenheilk 78:272–292
Kayser-Petersen JE, Schwab E (1923) Die Epidemiologie der epidemischen Encephalitis in Deutschland während der Jahre 1918–1920, mit besonderer Berücksichtigung des Zusammenhangs mit der Grippe. Zschr Hyg Infektionskrankh 100:339–346
Kirschbaum MA (1920) Über capilläre Gehirnblutungen. Frankf Z Pathol 23:444–472
Klarfeld B (1922) Einige allgemeine Betrachtungen zur Histopathologie des Zentralnervensystems (auf Grund von Untersuchungen über die Encephalitis epidemica). Zschr ges Neurol Psychiat 77:80–161
Klaue R (1940) Parkinsonsche Krankheit (Paralysis agitans) und postencephalitischer Parkinsonismus. Versuch einer klinisch-anatomischen Differentialdiagnose. Arch Psychiat 111:251–321
Koenigsdorf (1892) Ein neuer Fall von acuter haemorrhagischer Encephalitis während der jetzigen Influenza-Epidemie. Dtsch Med Wschr 18:182–184
Kuczynski MH, Wolff EK (1921) Ätiologie, Epidemiologie, pathologische Morphologie und Pathogenese der Grippe. B. The Pathomorphologie und Pathogenese der Grippe. Ergeb Allgem Pathol Pathol Anat 19:2 (Abt:947–1163)
Leichtenstern O (1892) Über primäre acute haemorrhagische Encephalitis (mit Demonstration). Dtsch Med Wschr 18:39–40
Leichtenstern O (1912) Influenza, 2nd edn (expanded and edited by Georg Sticker). Alfred Hölder, Vienna; Leipzig
Lucksch F (1928) Pathologic anatomy of influenza. A review based chiefly on German sources. Arch Pathol Lab Med 5:448–491
Marcus H (1920) Die Influenza und das Nervensystem. Studie während der Epidemie in Schweden 1918–1919. Zschr ges Neurol Psychiat 54:166–224
Marie P, Trétiakoff C (1920) Anatomie pathologique de l’encephalite lethargique (Etude histopathologique comparative de 4 cas). Ann Méd 7:1–15
Marinesco G (1918) Contribution à l’étude de l’histologie pathologique de l’encéphalite léthargique. Bull Acad Méd (Paris) 80:411–418
Maurizi CP (1989) Influenza caused epidemic encephalitis (encephalitis lethargica): the circumstantial evidence and a challenge to the naysayers. Med Hypotheses 28:139–142
Mayer EE (1919) Post-influenzal disturbances of the nervous system. J Am Med Assoc 72:670–671
Meerloo AM (1931) Die Grippekomplikationen und die toxische Grippe-Encephalopathie. Beitrag zum Problem Krankheitsform und Persönlichkeit. Zschr ges Neurol Psychiat 136:508–522
Mihara M, Utsugisawa K, Konno S, Tohgi H (2001) Isolated lesions limited to the bilateral substantia nigra on MRI associated with influenza A infection. Eur Neurol 45:290–291
Ministry of Health (1922) Encephalitis lethargica (Reports on public health and medical subjects No. 11). His Majesty’s Stationery Office, London
Nagtegaal CG (1927) Een geval van Parkinsonisme na typhus. Ned Tijdschr Geneeskd 71:2079–2083
Neel AV (1925) Om Forekomsten af Encephalitis lethargica og Singultus epidemica samt Influenza og Poliomyelitis ant. acut. i Danmark i de senere Aar. Hospitalstidende 68(392–403):409–415
Oppenheim H (1899a) Weiterer Beitrag zur Lehre von der acuten, nicht-eitrigen Encephalitis und der Poliencephalomyelitis. Dtsch Zschr Nervenheilk 15:1–27
Oppenheim H (1899b) Zur Encephalitis pontis des Kindesalters, zugleich ein Beitrag zur Symptomatologie der Facialis- und Hypoglossuslähmung. Berl Klin Wschr 36:405–409
Oppenheim H, Cassirer R (1907) Die Encephalitis, 2nd edn edn. Alfred Hölder, Vienna
Pette H (1932) Eine vergleichende Betrachtung der akut infektiösen Erkrankungen vornehmlich der grauen Substanz des Nervensystems (Poliomyelitis, epidemische Encephalitis, Lyssa, Bornasche Krankheit). Dtsch Zschr Nervenheilk 124:43–76
Pette H (1942) Epidemische Encephalitis (Economo). In: Die akut entzündlichen Erkrankungen des Nervensystems (Viruskrankheiten, Entmarkungsenzephalomyelitiden, Neuritiden). Georg Thieme, Leipzig, pp 153–220
Puin H (1957) Über hämorrhagische Encephalitis bei Grippe. Thesis, Frankfurt am Main
Rabinowitsch J (1928) Über die nervösen Erscheinungen beim Fleckfieber. Zschr ges Neurol Psychiat 115:34–84
Re G (1919) La cosidetta encefalite letargica acuta epidemica considerata come una manifestazione nervosa dell’ influenza. Rif Med 35:851–856
Reinhart A (1922) Die epidemische Encephalitis. Ergebn inn Med Kinderheilk 23:245–359
Rietti F (1935) Encefalite letargica acuta e cronica. Francesco Vallardi, Milano
Rostan A (1928) Contributo alla patologia dell’encefalite epidemica cronica. Riv Neurol 1:177–196
Schmidt J (1892) Acute primäre hämorrhagische Encephalitis. Dtsch Med Wschr 703
Schmidt MB (1905) Über Gehirnpurpura und hämorrhagische Encephalitis. Beitr Pathol Anat Allg Pathol Suppl 7:419–455
Schröder P, Pophal R (1921) Encephalitis epidemica und Grippe. Med Klin 17:875–876
Shinya K, Suto A, Kawakami M, Sakamoto H, Umemura T, Kawaoka Y, Kasai N, Ito T (2005) Neurovirulence of H7N7 influenza A virus: brain stem encephalitis accompanied with aspiration pneumonia in mice. Arch Virol 150:1653–1660
Siegmund H (1920) Zur pathologischen Anatomie der herrschenden Encephalitis epidemica. Berl Klin Wschr 57:509–512
Siegmund H (1921) Die Histopathologie der Encephalitis epidemica, zugleich ein Beitrag zur Lehre von der Entzündung der Hirnsubstanz. Frankf Z Pathol 25:526–565
Smith HF (1921) Epidemic encephalitis (encephalitis lethargica, nona). Report of studies conducted in the United States. Public Health Rep 36:207–242
Spatz H (1930) Encephalitis. In: Bumke O (ed) Handbuch der Geisteskrankheiten. 11. Band. Spezieller Teil VII. Die Anatomie der Psychosen. Julius Springer, Berlin, pp 157–281
Steininger C, Popow-Kraupp T, Laferl H, Seiser A, Gödl I, Djamshidian S, Puchhammer-Stöckl E (2003) Acute encephalopathy associated with influenza A virus infection. Clin Infect Dis 36:567–574
Stern F (1919/20) Die Pathologie der sogenannten “Encephalitis lethargica”. Arch Psychiat Nervenkr 61:621–692
Stern F (1923) Pathogenetische Probleme der epidemischen Encephalitis. Klin Wschr 2:433–436
Stern F (1936) Epidemische Encephalitis (Economosche Krankheit). In: Bumke O, Foerster O (eds) Handbuch der Neurologie. Band XIII. Spezielle Neurologie V, Erkrankungen des Rückenmarks und Gehirns III. Infektionen und Intoxicationen II. Julius Springer, Berlin, pp 307–500
Strümpell A (1885) Über die akute Encephalitis der Kinder (Polioencephalitis acuta, cerebrale Kinderlähmung). Jb Kinderheilk 22:173–178
Strümpell A (1920) Über Encephalitis epidemica (Encephalitis lethargica). Dtsch Med Wschr 46:705–707
Stuart-Harris CH (1953) Influenza and other virus infections of the respiratory tract. Edward Arnold, London
Stuart-Harris CH (1965) Influenza and other virus infections of the respiratory tract, 2nd edn edn. Edward Arnold, London
Takahashi M, Yamada T (2001) A possible role of influenza A virus infection for Parkinson’s disease. In: Calne D, Calne SM (eds) Parkinson’s disease (Advances in Neurology, vol 86). Lippincott Williams & Wilkins, Philadelphia; London, pp 91–104
Tobler T (1920) Pathologische Beiträge zur Kenntnis der akuten, herdförmig disseminierten, nichteitrigen, vorwiegend lymphocytären, infektiös-toxischen, epidemischen Polioencephalomyelitis (Encephalitis lethargica). Schweiz Med Wschr 1(446–453):470–475
Toovey S (2008) Influenza-associated central nervous system dysfunction: a literature review. Travel Med Infect Dis 6:114–124
Trétiakoff C (1919) Contribution a l’étude de l’anatomie pathologique du locus niger de Soemmering avec quelques déductions relatives à la pathogénie des troubles du tonus musculaire et de la maladie de Parkinson. Thesis, Paris
Vilensky JA, Gilman S (2006) Encephalitis lethargica: could this disease be recognised if the epidemic recurred? Pract Neurol 6:360–367
Virchow R, Senator H (1891) Hämorrhagische Apoplexie. Dtsch Med Wschr 17:1336–1337
von Economo C (1919) Grippe-Encephalitis und Encephalitis lethargica. Wr Klin Wschr 32:393–396
von Economo C (1929a) Die Encephalitis lethargica, ihre Nachkrankheiten und ihre Behandlung. Urban & Schwarzenberg, Berlin
von Economo C (1929b) Encephalitis lethargica (epidemica). In: Klemperer G, Klemperer F (eds) Neue Deutsche Klinik. Handwörterbuch der praktischen Medizin mit besonderer Berücksichtigung der inneren Medizin, der Kinderheilkunde und ihrer Grenzgebiete. III. Band. Urban & Schwarzenberg, Berlin, Wien, pp 106–135
von Strümpell A (1890) Über primäre acute Encephalitis. Dtsch Arch Klin Med 47:53–74
Wickman I (1913) Acute poliomyelitis: Heine-Medin’s disease (Nervous and mental disease monograph series,vol 16). The Journal of Nervous and Mental Disease, New York
Wilson SAK (1921) Case of paralysis agitans following malaria. Proc R Soc Med (London) 14 (Sect Neurol): 48
Wilson SAK (1954) Epidemic encephalitis. In: Bruce AN (ed) Wilson’s Neurology, vol vol 1, 2nd edn edn. Butterworth & Co, London, pp 118–165
Ждaнoв BM, Pyтштeйн ПB (1950) O тaк нaзывaeмыx пocтгpиппoзныx нeвpoинфeкцияx. Bpac Дeлo 9:837–840 (Zhdanov VM, Rutshteyn PV (1950) O tak nazyvayemykh postgrippoznykh neyroinfektsiyakh. Vrach Dyelo 9:837–840)
Эпштeйн, ФГ (1944) К xapaктepиcтикe тaк нaзывaeмыx гpиппoзныx зaбoлeвaний. Клин Meд (Mocк) 22(4):39–44 (Epshteyn FG (1944) K kharakteristike tak nasyvayemkh grippoznykh zabolevaniy. Klin med (Mosk) 22(4):39–44)
Acknowledgments
This work was supported by the Australian Research Council (Discovery Research Grant DP0451188; and an Australian Postdoctoral Fellowship) and by the National Library of Medicine (Grants for Scholarly Works in Biomedicine and Health, grant no 1G13LM00986 -01).
Author information
Authors and Affiliations
Corresponding author
Additional information
The three papers of this series are based on a presentation by the author on June 21, 2007 at the annual meeting of the International Society for the History of the Neurosciences in Los Angeles.
Rights and permissions
About this article
Cite this article
Foley, P.B. Encephalitis lethargica and the influenza virus. III. The influenza pandemic of 1918/19 and encephalitis lethargica: neuropathology and discussion. J Neural Transm 116, 1309–1321 (2009). https://doi.org/10.1007/s00702-009-0296-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-009-0296-8