Abstract
Background and Purpose
In recent years there has been a re-evaluation regarding the clinical implications of temporal lobe arachnoid cysts (temporal arachnoid cysts) in children. These cysts have often been considered asymptomatic, or if symptomatic, only causing focal neurological symptoms or signs of increased intracranial pressure. However, several studies have more recently reported on cognitive symptoms improving after surgery. This study aimed to evaluate if reported cognitive improvement after surgery of temporal arachnoid cysts were stable after five years.
Method
Ten consecutive children (m = 14.65; range 12.1–19.415 were assessed cognitively five years after micro-neurosurgical fenestration of a temporal arachnoid cyst. Results were compared to results from their pre- and post-surgical evaluations. Evaluations included the Wechsler-scales, Boston Naming Test (BNT), Rey Auditory Verbal Learning Test (RAVLT), verbal fluency test (FAS) and Rey Complex Figure Test (RCFT).
Results
The analysis revealed significant postsurgical improvement compared to baseline on the Wechsler-scales measures of general intelligence (FSIQ), verbal abilities (VCI) and processing speed (PSI). Mean differences after surgery were 8.3 for FSIQ, (p = 0.026), 8.5 for VI (p = < .01) and 9.9 for PSI (p = 0.03). There were no significant differences in mean test results when comparing postsurgical scores with scores five years after surgery, indicating long-term stability of improvements.
Conclusion
The results indicate that affected cognitive functions in children with temporal arachnoid cysts improve after surgery and that the improvements remain stable five years later. The improvements and long term stability were also consistent with the experience of both parents and children. The findings provide a strong argument for neurosurgical fenestration of temporal arachnoid cysts in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arachnoid cysts in children are benign, space-occupying, intracranial anomalies with a reported prevalence of up to 2.6% [3]. The origins of the cysts are not fully understood but they are often considered congenital, caused by a duplication of the arachnoid during fetal development. Another less commonly expressed hypothesis is that the cysts are secondary to trauma or infection [10]. The duplication of the arachnoid layers leads to the formation of a fluid-filled sac which may compress and dislocate adjacent structures including the brain parenchyma [45]. In children arachnoid cysts are often identified incidentally during the first decade of life, when the child is undergoing neuroimaging for other reasons [3]. The most common cyst location, seen in 47% of cases is the middle cranial fossa (temporal arachnoid cysts), where the cyst compresses or dislocates the temporal lobe and in many cases also ventral posterior parts of of the frontal lobe [3].
Though often considered asymptomatic, arachnoid cysts have been linked to symptoms like rapid head growth, headaches, seizures, increased intracranial pressure, increased head circumference, focal neurological symptoms and mental developmental delay [9]. During the last decades a number of studies have presented results indicating that arachnoid cysts may also cause cognitive symptoms.The majority of research regarding this have been conducted in older teenagers and adults. In one study, 55 patientswith arachnoid cysts (41 temporal arachnoid cysts) aged 16–70 years old, were assessed cognitively and results were compared to a healthy controlgroup. The patients with cysts performed worse on tests of visual retention, impulse control, visual scanning and sequencing [31]. In another study with 22 adult patients with supra-tentorial cysts (19 temporal arachnoid cysts) the patients performed worse than a control group in tests of verbal knowledge, mental flexibility, inhibitory capacity, problem solving, and planning skills [30]. This research have focused on arachnoid cysts in different locations.
More recent research have been conducted in children with cysts specifically located in the temporal lobe.Results indicate that children with temporal arachnoid cysts also present with cognitive symptoms. In a study by Cuny and co-workers 100 consecutive children with temporal arachnoid cysts were assessed cognitively [12]. The authors found that the children had lower results on the Wechsler-scales measure of general cognitive ability, verbal functions, processing speed and working memory. Impairments were also found in other tests of language, memory, executive functions and visual attention. In another study, 32 children with temporal arachnoid cysts were assessed with the Stanford Binet Intelligence Scale [23]. The results revealed significantly lower scores for general verbal knowledge, visuospatial functions and quantitative reasoning. In a previously published study from our team similar results were found in the presurgical assessment of 11 children with temporal arachnoid cysts. The children in our study had clearly below average preoperative scores on overall IQ, verbal comprehension and processing speed [33].
Alongside the growing knowledge of cognitive symptoms in children with temporal arachnoid cysts there are also studies reporting improvement in cognitive functions after decompression of the cysts. In a follow-up by Cuny [11] 34 of a initial 100 children that went through neurosurgery were re-assessed cognitively after surgery. The authors found statistically significant postsurgical improvement on the Wechsler-scales measures of overall IQ, verbal comprehension, processing speed. and perceptual reasoning. Improvement were also seen in language and memory functions. In another study [22] three boys with temporal arachnoid cysts were evaluated cognitively before and after neurosurgery. In the authors presurgical examination the results showed that the boys had lower scores in tests of general cognitive capacity, executive functions like attention and processing speed, when compared to the population norms. They also performed worse in tests of verbal memory. A postsurgical follow-up, conducted 3 to 6 months after surgery revealed improvements in general cognition, executive functions and verbal memory. The postsurgical assessment in our previous study [33] reported improvements in overall IQ, verbal comprehension and processing speed.
Temporal arachnoid cysts can be treated surgically, through microneurosurgical decompression. This reduces cyst size, intracystic pressure and mass effect. There is, however, a lack of consensus on whether or not the cysts should be treated surgically and what should be the indications for the procedure. The traditional standpoint is that temporal arachnoid cysts should be treated conservatively when asymptomatic or when symptoms are ambiguous. Surgery should only be proposed when patients present with signs of increased intracranial pressure, ascertained rupture with intracystic or subdural hemorrhage or risk thereof [5]. Cognitive symptoms have thus far not been considered as indicators for surgery [4, 40]. Research on both adults and children indicate that there may be cognitive symptoms in patients with temporal arachnoid cysts and that these improve after surgery and therefore the question is raised more frequently about whether these improvements also should be considered in a decision about surgery.
To the best of our knowledge no long term cognitive follow-up of surgically treated children with temporal arachnoid cysts has been done utilising the same set of comprehensive and psychometrically robust test-instruments in the presurgical, postsurgical and long-time follow-up. The aim of the present study was to evaluate if cognitive improvements after surgery of temporal arachnoid cysts in children are stable over a period of five years.
Materials and methods
This was a longitudinal prospective study conducted at Astrid Lindgren Children’s Hospital, Karolinska University Hospital, a tertiary hospital in Stockholm, Sweden. In the initial study 15 consecutive children with temporal arachnoid cysts were evaluated cognitively 6 months before surgery. Of these 15 children 11 underwent microneurosurgical fenestration of the cyst and were re-evaluated cognitively 6 months after the surgery [33]. One child was lost during the five-year follow-up and all results for that child were excluded from all analyses in the present study. In the present study 10 of the surgically treated children were evaluated five years after surgery (6 boys and 4 girls) (Tables 1 and 2). We compared the five-year follow-up results to the results from presurgical and postsurgical evaluations in the same cohort. The mean test–retest interval between the postoperative evaluation and five-year follow-up was 55.1 months. The median age at study inclusion was 9.2 years (range 6.8–12.6) and at the five-year follow-up, the median age was 14.7 years (range 12.1–19.4).
The children were evaluated by the same neuropsychologist (TA) on all three occasions with an identical set of standardized and age-adjusted cognitive tests.
Evaluation methods
Wechsler intelligence scale
Wechsler Intelligence scales [42] are used to assess cognitive functions. The test is individually administered and consists of fifteen subtests of which 10 is used to establish a full-scale IQ (FSIQ) and four indexes for comparison in this study; Verbal Comprehension index (VCI), Visuospatial Index (VSI), Working memory index (WMI) and Processing speed index (PSI). In earlier editions of the Wechsler Intelligence scales the VSI was called perceptual reasoning index (PRI). In the present study we use the term VSI. We used the fourth edition of the scales in the presurgical and postsurgical evaluations and WISC-V in the five-year follow-up. At the five-year follow-up, two participants were older than 16 years and thus were evaluated with the adult version of the Wechsler scales, WAIS-IV. We used the most current and age appropriate versions of the scales to ensure that the most recent norms were used. The scores of the three versions of the Wechsler scales can be considered equivalent. According to the tests technical manuals, the three versions can be considered measuring the same constructs with a high level of correlation between versions [13, 24, 42].
FAS
FAS is a test of phonological verbal fluency. The test subject is required to produce as many words as possible in 60 s each for the letters F, A, and S [38]
Boston Naming Test (BNT)
Boston Naming Test is a test of forced naming ability. The test subject is required to name nouns from 60 black-and-white pictures [38].
Rey Complex Figure Test (RCFT)
Rey Complex Figure Test is a test of visuospatial memory, where the test subject is required to draw a copy of a complex figure and recall the figure from memory after a 3 min and a 30 min delay [38]
Rey Auditory Verbal Learning Test (RAVLT)
The Rey Auditory Verbal Learning Test (RAVLT) assesses verbal memory. The test subject is required to remember 15 words read 5 times by the examiner, with recall after each repeated reading and after a 15-min delay [38]
Statistical analysis
A one-way repeated measures ANOVA with Bonferroni adjustment for multiple comparisons was used to compare the pre-surgical, post-surgical and five-year follow-up-results of the assessments with the Wechsler scales. The Friedman test was used to compare results for FAS, BNT, RAVLT and RCFT due to non-normally distributed data. The Wilcoxon rank-sum was used in analysis of between-group differences in the Friedman test. Data were analyzed with SPSS, version 28. Statistical significance level was preset to p < 0.05.
Results
Wechsler intelligence scale
There were significant differences in mean test scores when comparing results from the presurgical, postsurgical and five-year follow-up evaluations. When comparing postsurgical follow-up with baseline (presurgical scores) there were significant differences in the results for FSIQ (F (2, 10) = 9.852, p = 0.001), VCI (F (1.38, 10) = 6.37, p = 0.02) and PSI (F(2,10) = 6.47 p = 0.01). These indexes all improved from a low average presurgical level to an average postsurgical level. Mean improvement in FSIQ was 8.3 points (95% CI 1.00–15.61, p = 0.026) and on the VCI 8.5 points (95% CI 3.19–13.81, p = < 0.01). The largest improvement was detected in processing speed, with a mean difference of 9.9 points (95% CI 1.0–18.8, p = 0.03) between presurgical and postsurgical scores (Table 3).
When comparing the scores from the five-year follow-up with the scores from the postsurgical evaluation, no significant differences were found (FSIQ, (p = 1.00), VCI (p = 0.88), PSI (p = 1.0)), indicating stability of postsurgical improvements five years after surgery of TLACs in children. (Table 4).
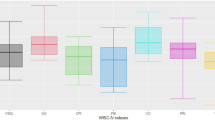
The results indicate that post-surgical improvements in cognitive test results remain stable after five years. The improvements in FSIQ, VCI and SI seen six months after surgery are still present after five years (Fig. 1). Results also indicate stability in the indexes that did not improve after surgery, indicating no deterioration in post-surgical results.
Preoperative, postoperative and five-year follow-up results on the Wechsler scales. FSIQ: Full Scale Intelligence Quotient. VCI: Verbal Comprehension Index. VSI: Perceptual Reasoning Index. WMI: Working Memory Index. PSI: Processing Speed Index. a population mean = 100, standard deviation = 15. Results ranging from 1 to 2 standard deviations below average are considered low average to clearly below average.*indicates significance
FAS
No significant differences in results were detected between any of the three occasions for verbal fluency (χ2 (2) = 1.20, p = 0.55). The results on the test of verbal fluency were on an average level before and after surgery as well as at the five-year follow-up (Table 5).
Boston Naming Test (BNT)
On the BNT the analysis detected no difference in results between the three occasions for picture naming (χ2(2) = 2.65, p = 0.27). The picture naming ability was on a presurgical level below average and remained on this level at both postsurgical and five year follow-up (Table 5).
Rey Complex Figure Test (RCFT)
No difference in results were found between the three occasions for visual memory (χ2(2) = 2.60, p = 0.27). The visual memory ability was on a level below average presurgically and at the postsurgical follow-up. Five years after surgery a non significant improvement to the level “low average” were seen (Table 5).
Verbal memory (RAVLT)
No significant differences were found between the results on the three occasions regarding verbal memory for a list of words (χ2(2) = 4.22, p = 0.12). The results for verbal memory was on an average level before surgery and remained on this level after surgery and at the five-year follow-up. (Table 5).
Discussion
The present study is to the best of our knowledge the first five year follow-up of cognitive functions after surgery of temporal arachnoid cysts in children. The results showed that postoperative improvement on the Wechsler-scales measures of general intellectual ability (FSIQ), verbal comprehension (VCI) and perceptual speed (PSI) in children with temporal arachnoid cysts remained stable five years after surgery. Several previous studies, including one by our team, have presented postoperative cognitive improvement [11, 23, 26, 30, 33]. These preoperative and postoperative comparisons have however been done with a shorter test–retest interval of 3–14 months and long term follow-ups have been lacking. One study investigated long term stability using a parent questionnaire to perform a follow up after four years. The authors found that parents experienced that postoperative cognitive improvement were still present after four years [11]. In the present five year follow-up we used the same comprehensive set of psychometrically robust cognitive test instruments as in the preoperative and postoperative asssessments [33].
When comparing preoperative and postoperative test results, several studies have presented improvement in general cognitive abilities measured with cognitive test batteries like the Wechsler-Scales, Stanford-Binet or Ravens Progressive Matrices [2, 11, 43]. These studies also report postoperative improvement in specific tests of perceptual functions, working memory, picture naming, verbal fluency and verbal memory. In our study we did not find improvement in results on tests of specific functions, neither at the short-term follow-up, nor after five years. We observed these functions to be on an average to low average level before surgery, after surgery, and at the five year follow-up.
Improvement of cognitive functions in children with ACs after surgery have a great impact on their everyday functioning. General IQ (FSIQ) predicts school performance to a large extent [32], and for this reason it would seem fair to conclude that the increase in the children’s FSIQ in our study would have a substantial impact on their overall school achievements. General intellectual functioning is not a single and coherent entity, and it is often divided into several underlying functions. In the Wechsler-scales this is represented by a hierarchical model where the FSIQ is the major factor explaining a substantial part of the variation in results on underlying functions in the test (VCI, VSI, WMI and PSI) [8]. As FSIQ explains a substantial part of underlying functions, an increase in this is of great value. In the present study we found an improvement of the VCI in the Wechsler-scales. This is of significance as verbal functions are important for memory formation and learning and also for social interactions [16]. The improvement in results on the PSI has an impact on the overall cognitive performance as processing speed gives a person quicker access to other cognitive functions [17, 39].
For children, school achievments are closely linked to their perceived quality of life and affects mental and emotional well-being [1]. Factors such as emotional resilience, self-esteem, ability to manage stress, and access to mental health support services can impact their emotional well-being and overall quality of life. The function of the temporal lobe can have a significant impact on an individual's quality of life. Dysfunction or impairment in the region can lead to various challenges that may affect daily functioning and overall well-being. Even small improvement in temporal lobe function might have an impact on the individual. Since the postsurgical improvement seems to be stable over time, it is possible that early intervention will produce the greatest benefit for the child.
A possible explanation to similarities between studies regarding improvement in verbal abilities and executive functions like attentional control and processing speed may be found in theories of neuroanatomical distribution of these functions. Many important language functions are located in the temporal lobe, perisylvian structures and from early childhood also posterior lateral and ventral frontal lobe structures [41]. The ventral and posterior lateral parts of the frontal lobe are also involved in executive functions [21]. The localization of the temporal arachnoid cysts adjacent to these structures may be one explanation to why they interfere with language and executive functions. However, for both language and executive functions like processing speed, attention and goal directed behavior the theory of strict localization of functions is a simplification. The theory must be complemented by more complex explanations, involving larger functional networks consisting of cortical and subcortical areas connected by white matter tracts [37, 44]. Language and executive functions rely on the integrity of the frontoparietal and language networks [6, 7, 15, 27]. Affected language and executive functions in children with temporal arachnoid cysts may be explained by this network theory, as structural and functional connectivity are related and alterations or damage to the structural network may affect functional connectivity [19].
Cysts are thought to act as mass lesions within the closed intracranial compartment and affect the adjacent brain parenchyma through local compression and possibly also by raising the overall intracranial pressure [28]. One possible explanation to the reduced capacity in certain cognitive domains lies in a decrease in regional cerebral blood-flow (rCBF) in structures and networks adjacent to the cyst. There are studies using Single-photon emission computed tomography (SPECT) that supports this hypothesis [25, 36]. As a decrease in rCBF have a negative impact on cognitive functioning [29, 34], a restoration of the blood-flow might explain the postoperative improvement of functional symptoms found in patients with ACs. The hypothesis of consequenses of mass-effects was also investigated in a study of brain glucose utilization in a patient with a left-sided temporal arachnoid cyst [14]. Using PET (Positron Emission Tomography) the researchers detected hypo-methabolism in the parenchyma adjacent to the cyst and after shunt-placement the metabolic activity in the affected parenchyma was significantly improved. The improvement in metabolism correlated with improvement of language functions. Language functions are typically located in the affected left hemisphere and this might be one explanation to this improvement. More research is however needed regarding the neurobiological mechanisms behind cognitive symptoms in temporal arachnoid cysts.
The finding that improvement in cognitive functions persist after five years is important, as it indicates that surgery has a potential of being beneficial for children with temporal arachnoid cysts in a longer perspective. The fact that the functions that did not improve in this study remained stable after five years is equally important, as this indicates that surgery does not seem to negatively affect cognitive functions in a longer perspective. Although results are promising for a postoperative reduction of cognitive symptoms and long term stability of these improvements, the risks of performing neurosurgery must also be taken into consideration. Risks include CSF leakage, postoperative infection, hemmorhage or need for reoperation [4]. The rate of complications in surgery of intracranial cysts differ somewhat between surgical techniques and complication rates reported for microneurosurgical fenestration of the cyst are between 6 and 16% and for endoscopic fenestration 10% to 18%. For cystoperitonial schunting the rate of complications has been reported to be 5% [35]. Specifically for children the rate of complications after surgery of temporal arachnoid cysts have been reported as low and when reported the complications are often considered mild [18]. When cysts are symptomatic several variabels have traditionally indicated the need for surgery: focal neurological deficits, mass effect, location, affected CSF dynamics, headaches and seizures [20]. In line with the results of the present study, cognitive symptoms should be considered as an additional important factor influencing the decision about surgery. A thorough cognitive evaluation should be a part of the investigation before a decision about surgery is made.
Limitations
The study was conducted on a small group of consecutive patients and the study had no controlgroup This of course limits the generalizability of the results and will have to be taken into consideration when interpreting the results. Our study group is heterogenous regarding age, cyst size and location which also might affect the external validity of the study.
Conclusion
In our study improvement in general intellectual ability, verbal functions and processing speed seen after surgery of temporal arachnoid cysts in children sustain over a period of five years after surgery. The improvement may have a significant impact on school achievements and consequently also on possibilities in the future lives of the children. The persistence of the improvement over a long period suggests that surgery of temporal arachnoid cysts in children may be justified in part by these improvements. A reasonable conclusion would be that the potential risk of cognitive deficits in these children must be considered and cognitive testing should be a part of the investigation in this group of patients.
Data availability
Data from the present study can be made available upon reasonable request.
References
Adelantado-Renau M, Monzonís-Carda I, Moliner-Urdiales D, Beltran-Valls MR (2023) The bidirectional longitudinal association between health-related quality of life and academic performance in adolescents: DADOS study. Qual Life Res 32:729–738. https://doi.org/10.1007/s11136-022-03291-z
Agopian-Dahlenmark L, Mathiesen T, Bergendal Å (2020) Cognitive dysfunction and subjective symptoms in patients with arachnoid cyst before and after surgery. Acta Neurochir (Wien) 162:1041–1050. https://doi.org/10.1007/s00701-020-04225-9
Al-Holou WN, Yew AY, Boomsaad ZE, Garton HJ, Muraszko KM, Maher CO (2010) Prevalence and natural history of arachnoid cysts in children. J Neurosurg Pediatr 5:578–585. https://doi.org/10.3171/2010.2.Peds09464
Ali M, Bennardo M, Almenawer SA, Zagzoog N, Smith AA, Dao D, Ajani O, Farrokhyar F, Singh SK (2015) Exploring predictors of surgery and comparing operative treatment approaches for pediatric intracranial arachnoid cysts: a case series of 83 patients. J Neurosurg Pediatr 16:275–282. https://doi.org/10.3171/2015.2.Peds14612
Amelot A, Beccaria K, Blauwblomme T, Bourgeois M, Paternoster G, Cuny ML, Zerah M, Sainte-Rose C, Puget S (2019) Microsurgical, endoscopic, and shunt management of pediatric temporosylvian arachnoid cysts: a comparative study. J Neurosurg Pediatr 23:749–757. https://doi.org/10.3171/2018.12.Peds18484
Ardila A, Ostrosky F (2022) What do neuropsychological tests assess? Appl Neuropsychol Adult 29:1–9. https://doi.org/10.1080/23279095.2019.1699099
Barbeau EB, Descoteaux M, Petrides M (2020) Dissociating the white matter tracts connecting the temporo-parietal cortical region with frontal cortex using diffusion tractography. Sci Rep 10:8186. https://doi.org/10.1038/s41598-020-64124-y
Canivez GL, Watkins MW, McGill RJ (2019) Construct validity of the Wechsler Intelligence Scale For Children - Fifth UK Edition: Exploratory and confirmatory factor analyses of the 16 primary and secondary subtests. Br J Educ Psychol 89:195–224. https://doi.org/10.1111/bjep.12230
Chen Y, Fang HJ, Li ZF, Yu SY, Li CZ, Wu ZB, Zhang YZ (2016) Treatment of middle cranial fossa arachnoid cysts: a systematic review and meta-analysis. World Neurosurg 92:480-490.e482. https://doi.org/10.1016/j.wneu.2016.06.046
Cincu R, Agrawal A, Eiras J (2007) Intracranial arachnoid cysts: current concepts and treatment alternatives. Clin Neurol Neurosurg 109:837–843. https://doi.org/10.1016/j.clineuro.2007.07.013
Cuny ML, Piolino P, Paternoster G, Piana H, Blauwblomme T, Beccaria K, Bourgeois M, Stricker S, Prodhomme J, Trousson C, Navarro B, Esnault E, Cozzo M, Abram M, James S, Boddaert N, Sainte-Rose C, Vaivre-Douret L, Puget S (2022) Temporosylvian arachnoid cysts in children. Part 2: Postoperative neuropsychological and clinical improvement. J Neurosurg Pediatr 30:50–159. https://doi.org/10.3171/2021.11.Peds21207
Cuny ML, Vaivre-Douret L, Piana H, Blauwblomme T, Beccaria K, Paternoster G, Bourgeois M, James S, Zerah M, Prodhomme J, Esnault E, Cozzo M, Trousson C, Navarro B, Stricker S, Boddaert N, Sainte-Rose C, Piolino P, Puget S (2022) Temporosylvian arachnoid cysts in children. Part 1: Cognitive profile of children with a temporal cyst and impact of the cyst in daily life. A prospective study in 100 consecutive children. J Neurosurg Pediatr 30:138–149. https://doi.org/10.3171/2021.11.Peds21203
Wechsler D (2008) WAIS-IV Technical and interpretive manual. NCS Pearson Inc, San Antonio, Texas
De Volder AG, Michel C, Thauvoy C, Willems G, Ferrière G (1994) Brain glucose utilisation in acquired childhood aphasia associated with a sylvian arachnoid cyst: recovery after shunting as demonstrated by PET. J Neurol Neurosurg Psychiatry 57:296–300. https://doi.org/10.1136/jnnp.57.3.296
Dick AS, Tremblay P (2012) Beyond the arcuate fasciculus: consensus and controversy in the connectional anatomy of language. Brain 135:3529–3550. https://doi.org/10.1093/brain/aws222
Esposito AG, Bauer PJ (2022) Determinants of elementary-school academic achievement: Component cognitive abilities and memory integration. Child Dev 93:1777–1792. https://doi.org/10.1111/cdev.13819
Gordon R, Smith-Spark JH, Newton EJ, Henry LA (2018) Executive function and academic achievement in primary school children: The use of task-related processing speed. Front Psychol 9:582. https://doi.org/10.3389/fpsyg.2018.00582
Helland CA, Wester K (2006) A population-based study of intracranial arachnoid cysts: clinical and neuroimaging outcomes following surgical cyst decompression in children. J Neurosurg 105:385–390. https://doi.org/10.3171/ped.2006.105.5.385
Honey CJ, Thivierge JP, Sporns O (2010) Can structure predict function in the human brain? Neuroimage 52:766–776. https://doi.org/10.1016/j.neuroimage.2010.01.071
Jafrani R, Raskin JS, Kaufman A, Lam S (2019) Intracranial arachnoid cysts: Pediatric neurosurgery update. Surg Neurol Int 10:15. https://doi.org/10.4103/sni.sni_320_18
Jones DT, Graff-Radford J (2021) Executive dysfunction and the prefrontal cortex. Continuum (Minneap Minn) 27:1586–1601. https://doi.org/10.1212/con.0000000000001009
Kwiatkowska K, Dębicka M, Maryniak A, Kwiatkowski S (2020) Cognitive impairment in children with arachnoid cyst of Sylvian fissure: does it justify the neurosurgical treatment? J Neurol Surg A Cent Eur Neurosurg 81:362–367. https://doi.org/10.1055/s-0039-1698385
Kwiatkowska K, Milczarek O, Dębicka M, Baliga Z, Maryniak A, Kwiatkowski S (2021) Are arachnoid cysts actually clinically mute in relation to neuropsychological symptoms? Cognitive functioning in children with AC of middle and cranial fossa. Clin Neurol Neurosurg 208:106825. https://doi.org/10.1016/j.clineuro.2021.106825
Lenhard A, Daseking M (2022) Accounting for intraindividual profiles in the wechsler intelligence scales improves the prediction of school performance. Children 9:1635. https://doi.org/10.3390/children9111635
Martínez-Lage JF, Almagro M-J, López-Guerrero AL (2018) Chapter 16 - SPECT studies in patients with arachnoid cysts. In: Cysts Arachnoid, (Epidemiology, Biology, and Neuroimaging, (eds) Wester K. Academic Press, Massachusetts, USA, pp 199–214. https://doi.org/10.1016/B978-0-12-809932-2.00016-8
Matsuda W, Akutsu H, Miyamoto S, Noguchi S, Tsunoda T, Sasaki M, Matsumura A (2010) Apparently asymptomatic arachnoid cyst: postoperative improvement of subtle neuropsychological impediment -case report. Neurol Med Chir (Tokyo) 50:430–433. https://doi.org/10.2176/nmc.50.430
Monroy-Sosa A, Chakravarthi SS, Cortes-Contreras AP, Hernandez-Varela M, Andres-Arrieta V, Epping A, Rovin RA (2021) The evolution of cerebral language localization: historical analysis and current trends. World Neurosurg 145:89–97. https://doi.org/10.1016/j.wneu.2020.09.028
Muhlestein WE, Maher CO (2021) Incidental intracranial cysts in children. Pediatr Clin North Am 68:775–782. https://doi.org/10.1016/j.pcl.2021.04.005
Nakamizo A, Amano T, Michiwaki Y, Kawano Y, Kuwashiro T, Yasaka M, Okada Y (2018) Long-term neurocognitive outcomes in patients with adult moyamoya disease. World Neurosurg 119:e441–e448. https://doi.org/10.1016/j.wneu.2018.07.179
Bg P, Schmid M, Hammar A, Wester K (2013) Intracranial arachnoid cysts: impairment of higher cognitive functions and postoperative improvement. J Neurodev Disord 5:21. https://doi.org/10.1186/1866-1955-5-21
Raeder MB, Helland CA, Hugdahl K, Wester K (2005) Arachnoid cysts cause cognitive deficits that improve after surgery. Neurology 64:160–162. https://doi.org/10.1212/01.Wnl.0000148724.61966.A4
Bea R (2015) Intelligence and school grades: A meta-analysis. Intelligence 53:118–137. https://doi.org/10.1016/j.intell.2015.09.002
Sandvik U, Adolfsson T, Jacobson DN, Tedroff K (2020) Cognition in children with arachnoid cysts. J Clin Med 9:850
Schmithorst VJ, Badaly D, Beers SR, Lee VK, Weinberg J, Lo CW, Panigrahy A (2022) Relationships between regional cerebral blood flow and neurocognitive outcomes in children and adolescents with congenital heart disease. Semin Thorac Cardiovasc Surg 34:1285–1295. https://doi.org/10.1053/j.semtcvs.2021.10.014
Schulz M, Oezkan Y, Schaumann A, Sieg M, Tietze A, Thomale UW (2021) Surgical management of intracranial arachnoid cysts in pediatric patients: radiological and clinical outcome. J Neurosurg Pediatr 28:102–112. https://doi.org/10.3171/2020.10.Peds20839
Sgouros S, Chapman S (2001) Congenital middle fossa arachnoid cysts may cause global brain ischaemia: a study with 99Tc-hexamethylpropyleneamineoxime single photon emission computerised tomography scans. Pediatr Neurosurg 35:188–194. https://doi.org/10.1159/000050420
Stam CJ, van Straaten EC (2012) The organization of physiological brain networks. Clin Neurophysiol 123:1067–1087. https://doi.org/10.1016/j.clinph.2012.01.011
Strauss ESEMS, Spreen O (2006) A compendium of neuropsychological tests. Oxford University Press
Takeuchi H, Kawashima R (2012) Effects of processing speed training on cognitive functions and neural systems. Rev Neurosci 23:289–301. https://doi.org/10.1515/revneuro-2012-0035
Tomita T, Kwasnicki AM, McGuire LS, Dipatri AJ (2023) Temporal sylvian fissure arachnoid cyst in children: treatment outcome following microsurgical cyst fenestration with special emphasis on cyst reduction and subdural collection. Childs Nerv Syst 39:127–139. https://doi.org/10.1007/s00381-022-05719-w
Wang J, Yamasaki BL, Weiss Y, Booth JR (2021) Both frontal and temporal cortex exhibit phonological and semantic specialization during spoken language processing in 7- to 8-year-old children. Hum Brain Mapp 42:3534–3546. https://doi.org/10.1002/hbm.25450
Wechsler D (2014) WISC-V Technical and interpretive manual. NCS Pearson, inc, San Antonio, Texas
Wester K, Hugdahl K (1995) Arachnoid cysts of the left temporal fossa: impaired preoperative cognition and postoperative improvement. J Neurol Neurosurg Psychiatry 59:293–298. https://doi.org/10.1136/jnnp.59.3.293
Wong C, Gallate J (2012) The function of the anterior temporal lobe: a review of the empirical evidence. Brain Res 1449:94–116. https://doi.org/10.1016/j.brainres.2012.02.017
Öcal E (2023) Understanding intracranial arachnoid cysts: a review of etiology, pathogenesis, and epidemiology. Childs Nerv Syst 39:73–78. https://doi.org/10.1007/s00381-023-05860-0
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the conceptualization or design of the work, drafted or revised the work critically for important intellectual content. Material preparation, data collection and analysis were performed by Tomas Adolfsson. The first draft of the manuscript was written by Tomas Adolfsson and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Regional Ethics Board in Stockholm (EPN 2018/1873–31) and adhered to the Helsinki Declaration.
Conflicts of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Consent
All legal guardians, children and adult participants were given oral and written study information and consented to participation in the study and publication of the results.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Adolfsson, T., Edström, E., Tedroff, K. et al. Cognition in children with arachnoid cysts – A five-year follow-up after microneurosurgical fenestration. Acta Neurochir 166, 226 (2024). https://doi.org/10.1007/s00701-024-06120-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06120-z