Abstract
Introduction
Early mobilization is key in neurologically impaired persons, limiting complications and improving long-term recovery. Self-balanced exoskeletons are used in rehabilitation departments to help patients stand and walk. We report the first case series of exoskeleton use in acute neurosurgery and intensive care patients, evaluating safety, clinical feasibility and patients’ satisfaction.
Methods
We report a retrospective observational study including individuals hospitalized in the neurosurgical intensive care and neurosurgery departments. We included patients with a medical prescription for an exoskeleton session, and who met no contraindication. Patients benefited from standing sessions using a self-balanced exoskeleton (Atalante, Wandercraft, France). Patients and sessions data were collected. Safety, feasibility and adherence were evaluated.
Results
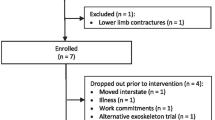
Seventeen patients were scheduled for 70 standing sessions, of which 27 (39%) were completed. They were typically hospitalized for intracranial hemorrhage (74%) and presented with unilateral motor impairments, able to stand but with very insufficient weight shifting to the hemiplegic limb, requiring support (MRC 36.2 ± 3.70, SPB 2.0 ± 1.3, SPD 0.7 ± 0.5). The average duration of standing sessions was 16 ± 9 min. The only side effect was orthostatic hypotension (18.5%), which resolved with returning to seating position. The most frequent reason for not completing a session was understaffing (75%). All patients were satisfied and expressed a desire to repeat it.
Conclusions
Physiotherapy using the exoskeleton is safe and feasible in the acute neurosurgery setting, although it requires adaptation from the staff to organize the sessions. An efficacy study is ongoing to evaluate the benefits for the patients.

Similar content being viewed by others
Data availability
Data are available on demand for academic purpose.
Code availability
Not applicable.
Abbreviations
- MRC:
-
Medical Research Council
- SPB:
-
Seated postural balance
- SPD:
-
Standing postural balance
References
Apra C, Serra M, Robert H, Carpentier A (2022) Early rehabilitation using gait exoskeletons is possible in the neurosurgical setting, even in patients with cognitive impairment. Neurochirurgie 68(4):458–460
Bowen DJ, Kreuter M, Spring B et al (2009) How we design feasibility studies. Am J Prev Med 36(5):452–457
Cuschieri S (2019) The STROBE guidelines. Saudi J Anaesth 13(Suppl 1):S31–S34
Langhorne P, Wu O, Rodgers H, Ashburn A, Bernhardt J (2017) A Very Early rehabilitation trial after stroke (AVERT): a phase III, multicentre, randomised controlled trial. Health Technol Assess 21(54):1–120
Lee SY, Amatya B, Judson R, Truesdale M, Reinhardt JD, Uddin T, Xiong X-H, Khan F (2019) Clinical practice guidelines for rehabilitation in traumatic brain injury: a critical appraisal. Brain Inj 33(10):1263–1271
Lo K, Stephenson M, Lockwood C (2017) Effectiveness of robotic assisted rehabilitation for mobility and functional ability in adult stroke patients: a systematic review. JBI Database System Rev Implement Rep 15(12):3049–3091
Louie DR, Mortenson WB, Durocher M, Teasell R, Yao J, Eng JJ (2020) Exoskeleton for post-stroke recovery of ambulation (ExStRA): study protocol for a mixed-methods study investigating the efficacy and acceptance of an exoskeleton-based physical therapy program during stroke inpatient rehabilitation. BMC Neurol 20(1):35
Morone G, Bragoni M, Iosa M, De Angelis D, Venturiero V, Coiro P, Pratesi L, Paolucci S (2011) Who may benefit from robotic-assisted gait training? A randomized clinical trial in patients with subacute stroke. Neurorehabil Neural Repair 25(7):636–644
Mortenson WB, Pysklywec A, Chau L, Prescott M, Townson A (2022) Therapists’ experience of training and implementing an exoskeleton in a rehabilitation centre. Disabil Rehabil 44(7):1060–1066
Nydahl P, Sricharoenchai T, Chandra S, Kundt FS, Huang M, Fischill M, Needham DM (2017) Safety of patient mobilization and rehabilitation in the intensive care unit. Systematic review with meta-analysis. Ann Am Thorac Soc 14(5):766–777
Park G-M, Cho S-H, Hong J-T, Kim D-H, Shin J-C (2023) Effects and safety of wearable exoskeleton for robot-assisted gait training: a retrospective preliminary study. J Pers Med 13(4):676
Ueba T, Hamada O, Ogata T, Inoue T, Shiota E, Sankai Y (2013) Feasibility and safety of acute phase rehabilitation after stroke using the hybrid assistive limb robot suit. Neurol Med Chir 53(5):287–290
Winkelman C, Peereboom K (2010) Staff-perceived barriers and facilitators. Crit Care Nurse 30(2):S13–S16. https://doi.org/10.4037/ccn2010393
Winstein CJ, Stein J, Arena R et al (2016) Guidelines for adult stroke rehabilitation and recovery. Stroke 47(6):e98–e169
Acknowledgements
The authors thank Mrs Christine Bacnus and the neurosurgical department paramedical staff for their help. We thank « L'Union des Blessés de la Face et de la Tête » and « Fonds APRES » of the Assistance Publique – Hôpitaux de Paris APHP for financial support.
Funding
The exoskeleton was funded by « L'Union des Blessés de la Face et de la Tête» and « Fonds APRES» of the Assistance Publique – Hôpitaux de Paris APHP.
Author information
Authors and Affiliations
Contributions
CA developed the original idea. MS, VD, AC and CA coordinated the funding of the exoskeleton. VD, AC, MR and CA organized the access to the exoskeleton, selected and informed the patients. AEK, MS, AL, CG, HN and MR performed the exoskeleton sessions and collected the clinical data. AEK, MS, AL and CA performed the data analyses. AEK and MS drafted the manuscript. CA critically revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval
The procedures used in this study adhere to the tenets of the Declaration of Helsinki and comply with the French law Jarde 2012–300. Approval was granted to the intensive care department for the use of innovative therapy to improve the standard of care.
Consent to participate
Informed consent was obtained from all individual participants included in the study or their legal guardian.
Consent for publication
The authors affirm that participants provided informed consent for publication of the images in Fig. 1 and for their data analysis and publication.
Conflicts of interest/Competing interests
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous communication
Preliminary results from this work have been presented at the congress for the “Société de Langue Française de Réanimation” in French in June 2023 by M. Serra.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
El Kaim, A., Serra, M., De Noray, H. et al. Safety and practicality study of using an exoskeleton in acute neurosurgery patients. Acta Neurochir 166, 221 (2024). https://doi.org/10.1007/s00701-024-06112-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06112-z