Abstract
Objective
To investigate the visual outcomes and optimal timing for repeat surgery in cases of postoperative hematoma following transsphenoidal surgery for pituitary neuroendocrine tumors (PitNETs).
Methods
A retrospective study was conducted on 28 patients who developed evident postoperative hematoma out of a total of 9,010 patients. The hematomas were classified into three types based on their CT appearance. Type 1a - mild high density with no tension, Type 1b - thin-layer high density; Type 2a - solid high density with large empty cavities, Type 2b - solid high density with small empty cavities; Type 3 –solid high density with no cavity showing high tension. Patient data were collected for analysis.
Results
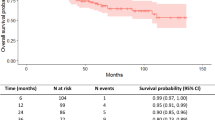
The study cohort comprised 10 female and 18 male patients, with a mean age of 51.5±11.9 years. Most patients presented with large adenomas (median diameter 36mm). Postoperative visual sight improved in 12 patients, remained stable in 11 patients, and worsened in 5 patients. Notably, no patients experienced worsened visual sight beyond twenty-four hours after the operation. Among the five patients with visual deterioration, four had CT type 3 hematoma (4/6, 66.7%), and one had CT type 2b hematoma (1/9, 11.1%). Patients in the type 3 CT group were significantly more prone to experience visual deterioration compared to those in the type 2 group (odds ratio [OR] 2.154 [95% CI 1.858-611.014], P=.027). Four patients underwent repeat surgery after visual deterioration, resulting in visual improvement following a prolonged recovery period. Postoperative hematoma had limited impact on pituitary dysfunction and hyponatremia.
Conclusion
Our study reveals a significant association between postoperative hematoma CT types and visual deterioration. For patients with stable visual sight and type 1 or 2a hematoma, conservative strategies may be considered. Conversely, type 2b and 3 patients are at higher risk of visual deterioration, especially within the first 24 hours after the operation. Consequently, early reoperation before vision worsens may be a prudent approach to reduce risks and improve visual outcomes, particularly in type 3 patients.


Similar content being viewed by others
Data availability
The datasets used or analysed during the current study are available from the corresponding author on reasonable request.
References
Akbari H, Malek M, Ghorbani M, Ramak Hashemi SM, Khamseh ME, Zare Mehrjardi A, Emami Z, Ebrahim Valojerdi A (2018) Clinical outcomes of endoscopic versus microscopic trans-sphenoidal surgery for large pituitary adenoma. Br J Neurosurg 32(2):206–209
Asa SL, Mete O, Perry A, Osamura RY (2022) Overview of the 2022 WHO Classification of Pituitary Tumors. Endocr Pathol 33(1):6–26
Atkinson JL, Nippoldt TB, Koeller KK (2008) Reoperation for sella haematoma after pituitary surgery. Clin Endocrinol (Oxf) 68(3):413–415
El-Asmar N, El-Sibai K, Al-Aridi R, Selman WR, Arafah BM (2016) Postoperative sellar hematoma after pituitary surgery: clinical and biochemical characteristics. Eur J Endocrinol 174(5):573–582
Gittleman H, Ostrom QT, Farah PD et al (2014) Descriptive epidemiology of pituitary tumors in the United States, 2004-2009. J Neurosurg 121(3):527–535
Guinto Balanzar G, Abdo M, Mercado M, Guinto P, Nishimura E, Arechiga N (2011) Diaphragma sellae: a surgical reference for transsphenoidal resection of pituitary macroadenomas. World neurosurgery 75(2):286–293
Hojo M, Goto M, Miyamoto S (2013) Chronic expanding pituitary hematoma without rebleeding after pituitary apoplexy. Surg Neurol Int 4:41
Li J, Ding W, Huang Z, Xie B, Li ZY (2019) Comparison of Short-Term Outcomes Between Endoscopic and Microscopic Trans-Sphenoidal Surgery for the Treatment of Pituitary Adenoma. J Craniofac Surg 30(8):2421–2424
Lin K, Li J, Lu L et al (2021) Diaphragma sellae sinking can predict the onset of hyponatremia after transsphenoidal surgery for pituitary adenomas. J Endocrinol Invest 44(11):2511–2520
Lin K, Lu L, Pei Z, Mu S, Huang S, Wang S (2022) Predictive factors for delayed hyponatremia after transsphenoidal surgery in patients with pituitary adenomas. Endocr Connect 11(1):e210497
Lin K, Zeng R, Mu S, Lin Y, Wang S (2022) Novel Nomograms to Predict Delayed Hyponatremia After Transsphenoidal Surgery for Pituitary Adenoma. Front Endocrinol (Lausanne) 13:900121
Martinez-Perez R, Requena LC, Carrau RL, Prevedello DM (2021) Modern endoscopic skull base neurosurgery. Journal of neuro-oncology 151(3):461–475
Ogawa Y, Sato K, Matsumoto Y, Tominaga T (2016) Evaluation of Fine Feeding System and Angioarchitecture of Giant Pituitary Adenoma--Implications for Establishment of Surgical Strategy. World neurosurgery 85:244–251
Pereira MP, Oh T, Joshi RS et al (2020) Clinical characteristics and outcomes in elderly patients undergoing transsphenoidal surgery for nonfunctioning pituitary adenoma. Neurosurg Focus 49(4):E19
Semple PL, Webb MK, de Villiers JC, Laws ER Jr (2005) Pituitary apoplexy. Neurosurgery 56(1):65-72; discussion -3
Tagoe NN, Essuman VA, Bankah P, Dakurah T, Hewlett VK, Akpalu J, Ndanu TA (2019) Visual Outcome of Patients with Pituitary Adenomas Following Surgery and Its Contributory Factors at a Tertiary Hospital in Ghana. Ethiop J Health Sci 29(1):895–902
Thakur JD, Corlin A, Mallari RJ et al (2021) Complication avoidance protocols in endoscopic pituitary adenoma surgery: a retrospective cohort study in 514 patients. Pituitary 24(6):930–942
Thotakura AK, Patibandla MR, Panigrahi MK, Addagada GC (2017) Predictors of visual outcome with transsphenoidal excision of pituitary adenomas having suprasellar extension: A prospective series of 100 cases and brief review of the literature. Asian J Neurosurg 12(1):1–5
Turgut M, Ozsunar Y, Başak S, Güney E, Kir E, Meteoğlu I (2010) Pituitary apoplexy: an overview of 186 cases published during the last century. Acta Neurochir (Wien) 152(5):749–761
Veldhuis JD, Santen RJ (1979) Pituitary pseudotumor. Mimicry of recurrent prolactinoma by a chronic intrasellar hematoma. Arch Intern Med 139(11):1309–1311
Yano S, Hide T, Shinojima N (2017) Efficacy and Complications of Endoscopic Skull Base Surgery for Giant Pituitary Adenomas. World neurosurgery 99:533–542
Funding
This study was supported by National Natural Science Foundation of China (grant number 82003023) and Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (grant number 2022-JKCS-06).
Author information
Authors and Affiliations
Contributions
Peng Li: Conceptualization, Methodology. Zhe Zhang, Shiwei Li, Ying Wang, Zhenmin Wang: Data curation, Writing- Original draft preparation. Xingchao Wang, Bo Wang: Visualization, Investigation. Zhijun Yang: Supervision. Pinan Liu: Writing- Reviewing and Editing.
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by institutional review boards of Beijng Tiantan Hospital, Capital Medical University (KY2023-170-02).
Code availability
Not applicable.
Consent to participate
Waiver of informed consent was granted because of the retrospective nature of this study.
Consent for publication
Not applicable.
Conflict of interests
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Z., Li, S., Wang, Y. et al. Visual outcomes and optimal timing for repeat surgery in cases of postoperative hematoma following transsphenoidal surgery for pituitary neuroendocrine tumors: A retrospective cohort study. Acta Neurochir 166, 127 (2024). https://doi.org/10.1007/s00701-024-06027-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06027-9