Abstract
Purpose
Endoscope-assisted transsphenoidal surgery over the last few years has led to more radical excision of pituitary adenomas (PAs) with a low complication rate. Systematic registration of complications by experienced surgical teams could help to improve this technique while ameliorating the patients’ quality of life.
Materials and methods
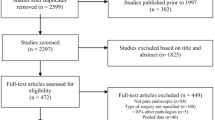
One hundred ten endoscopic procedures were performed in 94 patients with PAs (37 functional) by the same neurosurgical team of a tertiary center during the period 2014–2019. Post-surgical complications were analyzed and compared with data published during the last 5 years in the PubMed and Cochrane databases by performing a systematic review and meta-analysis of the literature.
Results
The overall complication rate in our series was 23.4%. Diabetes insipidus (DI) and intraoperative cerebrospinal fluid (CSF) leakage were the commonest complications (12.8%), followed by postoperative hypopituitarism (9.2%) and hematoma (8.5%) during the follow-up of 2.15 ± 1.4 years. Syndrome of inappropriate antidiuretic hormone secretion, meningitis, deep vein thrombosis, and hyposmia were rare (< 3%). Postoperative hypopituitarism was significantly associated with incidence of hematoma. No statistically significant association was found between PAs Hardy and Knosp scale grading or between patients’ characteristics with the occurrence of postoperative complications. Our meta-analysis including nine studies found no significant differences comparing the complications of endoscopic versus microscopic surgery.
Conclusion
The endoscopic approach is safe when performed by experienced surgical teams. CSF leakage and DI were the commonest complications in our series; however, confirmation by larger studies is required. Meta-analysis showed no statistically significant differences in complication rates comparing endoscopic versus microscopic surgery.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author [P.S.].
Code availability
Not applicable.
Change history
15 April 2022
A Correction to this paper has been published: https://doi.org/10.1007/s42000-022-00367-w
References
Fernandez A, Karavitaki N, Wass JA (2010) Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin Endocrinol (Oxf) 72(3):377–382. https://doi.org/10.1111/j.1365-2265.2009.03667.x
Mete O, Cintosun A, Pressman I, Asa SL (2018) Epidemiology and biomarker profile of pituitary adenohypophysial tumors. Mod Pathol 31(6):900–909. https://doi.org/10.1038/s41379-018-0016-8
Ezzat S, Asa SL, Couldwell WT, Barr CE, Dodge WE, Vance ML et al (2004) (2004) The prevalence of pituitary adenomas: a systematic review. Cancer 101(3):613–619. https://doi.org/10.1002/cncr.20412
Ntali G, Wass JA (2018) Epidemiology, clinical presentation and diagnosis of non-functional pituitary adenomas. Pituitary 1(2):111–118. https://doi.org/10.1007/s11102-018-0869-3
Lee JP, Park IW, Chung YS (2011) The volume of tumor mass and visual field defect in patients with pituitary macroadenoma. Korean J Ophthalmol 25(1):37–41. https://doi.org/10.3341/kjo.2011.25.1.37
Shlomo M (2011) Pathogenesis of pituitary tumors. Nat Rev Endocrinol 7:257–266. https://doi.org/10.1038/nrendo.2011.40
Syro LV, Rotondo F, Ramirez A, Di Ieva A, Sav MA, Restrepo LM et al (2015) Progress in the diagnosis and classification of pituitary adenomas. Front Endocrinol (Lausanne) 6:97. https://doi.org/10.3389/fendo.2015.00097
Levy MJ, Jäger H, Powell M, Matharu MS, Meeran K, Goadsby PJ (2004) Pituitary volume and headache. Size is not everything. Arch Neurol 61(5):721–725. https://doi.org/10.1001/archneur.61.5.721
Marazuela M, Astigarraga AV, Estrada C, García-Uría J, Lucas T (1994) Recovery of visual and endocrine function following transhenoidal surgery of large nonfunctioning pituitary adenomas. J Endocrinol Invest 17:703–707. https://doi.org/10.1007/BF03347763
Theodros D, Patel M, Ruzevick J, Lim M, Bettegowda C (2015) Pituitary adenomas: historical perspective, surgical management and future directions. CNS Oncol. 4(6):411–29. https://doi.org/10.2217/cns.15.21
Schmidt RF, Choudhry OJ, Takkellapati R, Eloy JA, Couldwell WT, Liu JK (2012) Hermann Schloffer and the origin of transsphenoidal pituitary surgery. Neurosurg Focus 33(2):E5. https://doi.org/10.3171/2012.5.FOCUS12129
Hirsch O (1910) Endonasal method of removal of hypophyseal tumors with report of two successful cases. J Amer Med Ass 55:772–774. https://doi.org/10.1001/jama.1910.04330090046014
Cushing H (1914) The Weir Mitchell lecture: surgical experiences with pituitary disorders. JAMA 63:1516–1525
Hardy J (1971) Transphenoidal hypophysectomy. J Neurosurg 34:582–594. https://doi.org/10.3171/jns.1971.34.4.0582
Ciric I, Ragin A, Baumgartner C, Pierce D (1997) Complications of transsphenoidal surgery: results of a national survey, review of the literature, and personal experience. Neurosurgery 40:225–237. https://doi.org/10.1097/00006123-199702000-00001
Cappabianca P, Cavallo LM, Colao A, Diviviis E (2002) Surgical complications associated with the endoscopic endonasal transsphenoidal approach for pituitary adenomas. J Neurosurg 97:293–298. https://doi.org/10.3171/jns.2002.97.2.0293
Jho HD (2001) Endoscopic transsphenoidal surgery. J Neurooncol 54:187–195. https://doi.org/10.1023/a:1012969719503
Yang I, Wang MB, Bergsneider M (2010) Making the transition from microsurgery to endoscopic trans-sphenoidal pituitary neurosurgery. Neurosurg Clin N Am 21(4):643–651. https://doi.org/10.1016/j.nec.2010.07.008
Agam MS, Wedemeyer MA, Wrobel B, Weiss MH, Carmichael JD, Zada G (2018) Complications associated with microscopic and endoscopic transsphenoidal pituitary surgery: experience of 1153 consecutive cases treated at a single tertiary care pituitary center. J Neurosurg 1:1–8. https://doi.org/10.3171/2017.12.JNS172318
Hardy J (1991) Atlas of transsphenoidal microsurgery in pituitary tumors. Igaku-Shoin Medical Publishers, New York. https://doi.org/10.1002/micr.1920120510
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33(4):610–617. https://doi.org/10.1227/00006123-199310000-00008
Li A, Liu W, Cao P, Zheng Y, Bu Z, Zhou T (2017) Endoscopic versus microscopic transsphenoidal surgery in the treatment of pituitary adenoma: a systematic review and meta-analysis, world neurosurgery. 101:236–246, ISSN 1878–8750. https://doi.org/10.1016/j.wneu.2017.01.022.
Partlett C, Riley RD (2017) Random effects meta-analysis: coverage performance of 95% confidence and prediction intervals following REML estimation. Stat Med 36(2):301–317. https://doi.org/10.1002/sim.7140
Akbari H, Malek M, Ghorbani M, Hashem S M Ri, Khamseh M E, Ali Zare Mehrjardi AZ, et al. (2018) Clinical outcomes of endoscopic versus microscopic trans-sphenoidal surgery for large pituitary adenoma, Br J Neurosurg 32:2, 206–209. https://doi.org/10.1080/02688697.2018.1429569
Broersen LHA, van Haalen FM, Biermasz NR, Lobatto DJ, Verstegen MJT, van Furth WR, W R, et al (2019) Microscopic versus endoscopic transsphenoidal surgery in the Leiden cohort treated for Cushing’s disease: surgical outcome, mortality, and complications. Orphanet J Rare Dis 14:64. https://doi.org/10.1186/s13023-019-1038-0
Castaño-Leon AM, Paredes I, Munarriz PM, Jiménez-Roldán L, Hilario A, Calatayud M et al (2020) Endoscopic transnasal trans-sphenoidal approach for pituitary adenomas: a comparison to the microscopic approach cohort by propensity score analysis. Neurosurgery 86(3):348–356. https://doi.org/10.1093/neuros/nyz201
Eseonu CI, ReFaey K, Rincon-Torroella J, Garcia O, Wand G S, Salvatori R, et al. (2017) Endoscopic versus microscopic transsphenoidal approach for pituitary adenomas: comparison of outcomes during the transition of methods of a single surgeon; World Neurosurg 97:317–325, ISSN 1878–8750. https://doi.org/10.1016/j.wneu.2016.09.120
Gao Y, Zheng H, Xu S, Zheng Y, Wang Y, Jiang J et al (2016) Endoscopic versus microscopic approach in pituitary surgery. J Craniofac Surg 27(2):e157–e159. https://doi.org/10.1097/SCS.0000000000002401
Guo-Dong H, Tao J, Ji-Hu Y, Guo-Dong H, Tao J, Ji-Hu Y, Wen-Jian Z, Xie-Jun Z, Jian G et al (2016) Endoscopic versus microscopic transsphenoidal surgery for pituitary tumors. J Craniofac Surg 27(7):e648–e655. https://doi.org/10.1097/scs.0000000000003000
Guvenc G, Kizmazoglu C, Pinar E, Imre A, Kaya I, Bezircioglu H et al (2016) Outcomes and complications of endoscopic versus microscopic transsphenoidal surgery in pituitary adenoma. J Craniofac Surg 27(4):1015–1020. https://doi.org/10.1097/scs.0000000000002684
Levi V, Bertani GA, Guastella C, Pignataro L, Zavanone ML, Rampini PM et al (2017) Microscopic versus endoscopic transsphenoidal surgery for pituitary adenoma: analysis of surgical safety in 221 consecutive patients. Clin Otolaryngol 42(2):466–469. https://doi.org/10.1111/coa.12631
Zaidi HA, Awad AW, Bohl MA, Chapple K, Knecht L, Jahnke H et al (2016) Comparison of outcomes between a less experienced surgeon using a fully endoscopic technique and a very experienced surgeon using a microscopic transsphenoidal technique for pituitary adenoma. J Neurosurg 124(3):596–604. https://doi.org/10.3171/2015.4.JNS15102
De Divitiis E, Cappabianca P, Cavallo M (2003) Endoscopic endonasal transsphenoidal approach to the sellar region. In: de Divitiis E, Cappabianca P (eds) Endoscopic endonasal transsphenoidal surgery. Springer. Wien, pp 91–130. https://doi.org/10.1007/978-3-7091-6084-8_7
Shou X, Shen M, Zhang Q, Zhang Y, He W, Ma Z et al (2016) Endoscopic endonasal pituitary adenomas surgery: the surgical experience of 178 consecutive patients and learning curve of two neurosurgeons. BMC Neurol 16(1):247. https://doi.org/10.1186/s12883-016-0767-0
Varshney S, Gupta C, Bansal KK, Bist SS, Bhagat S (2013) Endoscopic trans-nasal trans-sphenoidal (TNTS) approach for pituitary adenomas: our experience. Indian J Otolaryngol Head Neck Surg 65(Suppl 2):308–313. https://doi.org/10.1007/s12070-011-0457-6
Rotenberg B, Tam S, Ryu WH, Duggal N (2010) Microscopic versus endoscopic pituitary surgery: a systematic review. Laryngoscope 120:1292–1297. https://doi.org/10.1002/lary.20949
Schur S, Lasry O, Tewfik MA, Di Mai S (2001) Assessing the association of tumor consistency and gland manipulation on hormonal outcomes and delayed hyponatremia in pituitary macroadenoma surgery. J Endocrinol Invest 24(2):83–87. https://doi.org/10.1016/j.inat.2019.100628
Younus I, Gerges MM, Godil SS, Uribe-Cardenas R, Dobri GA, Ramakrishna R et al (2019) Incidence and risk factors associated with reoperation for sellar hematoma following endoscopic transsphenoidal pituitary surgery. J Neurosurg 23:1–7. https://doi.org/10.3171/2019.6.JNS191169
Zhou T, Wei SB, Meng XH, Xu BN (2010) Pure endoscopic endonasal transsphenoidal approach for 375 pituitary adenomas. Zhonghua Wai Ke Za Zhi 48(19):1443–1446
Black PM, Zervas NT, Candia GL (1987) Incidence and management of complications of transsphenoidal operation for pituitary adenomas. Neurosurgery 20(6):920–924. https://doi.org/10.1227/00006123-198706000-00017
Charalampaki P, Ayyad A, Kockro RA, Perneczky A (2009) Surgical complications after endoscopic transsphenoidal pituitary surgery. J Clin Neurosci 16:786–789. https://doi.org/10.1016/j.jocn.2008.09.002
Chowdhury T, Prabhakar H, Bithal PK, Schaller B, Dash HH (2014) Immediate postoperative complications in transsphenoidal pituitary surgery: a prospective study. Saudi J Anaesth 8(3):335–341. https://doi.org/10.4103/1658-354X.136424
Gondim JA, Almeida JPC, Albuquerque LAF, Schops M, Gomes E, Ferraz T et al (2011) Endoscopic endonasal approach for pituitary adenoma: surgical complications in 301 patients. Pituitary 14:174–183. https://doi.org/10.1007/s11102-010-0280-1
Smith TR, Maher Hulou M, Huang KT et al (2015) (2015) Complications after transsphenoidal surgery for patients with Cushing’s disease and silent corticotroph adenomas. Neurosurg Focus 38(2):E12. https://doi.org/10.3171/2014.10.FOCUS14705
Rudnik A, Kos-Kudła B, Larysz D, Zawadzki T, Bazowski P (2007) Endoscopic transsphenoidal treatment of hormonally active pituitary adenomas. Neuro Endocrinol Lett 28(4):438–444. https://doi.org/10.1007/s11102-018-0893-3
Zada G, Cavallo LM, Esposito F, Fernandez-Jimenez JC, Tasiou A, De Angelis M et al (2010) Transsphenoidal surgery in patients with acromegaly: operative strategies for overcoming technically challenging anatomical variations. Neurosurg Focus 29(4):E8. https://doi.org/10.3171/2010.8.FOCUS10156
Olson BR, Gumowski J, Rubino D, Oldfield EH (1997) (1997) Pathophysiology of hyponatremia after transsphenoidal pituitary surgery. J Neurosurg. 87(4):499–507. https://doi.org/10.3171/jns.1997.87.4.0499
Cavallo LM, Solari D, Tasiou A, Esposito F, de Angelis M, D’Enza AI et al (2013) Endoscopic endonasal transsphenoidal removal of recurrent and regrowing pituitary adenomas: experience on a 59-patient series. World Neurosurg 80:342–350. https://doi.org/10.1016/j.wneu.2012.10.008
El-Asmar N, El-Sibai K, Al-Aridi R, Selman WR, Arafah BM (2016) Postoperative sellar hematoma after pituitary surgery: clinical and biochemical characteristics. Eur J Endocrinol 5:573–582. https://doi.org/10.1530/EJE-15-0961
Tabaee A, Anand VK, Barrón Y, Hiltzik DH, Brown SM, Kacker A et al (2009) Endoscopic pituitary surgery: a systematic review and meta-analysis. J Neurosurg 111:545–554. https://doi.org/10.3171/2007.12.17635
Author information
Authors and Affiliations
Contributions
Conceptualization: SP and AA. Methodology: KS and TS. Data curation: SP. Formal analysis and investigation: MC and TG. Meta-analysis: AF. Writing-original draft and preparation: SP and KG. Writing-review and editing: SP and AA. Supervision and final approval: KS, TS, and AA.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The Bioethics Committee of the Medical School of National and Kapodistrian University of Athens, Athens, Greece (No 142/27.06.2019) approved the study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Additional informed consent was obtained from all individual participants for whom identification information is included in this article.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Stefanidis, P., Kyriakopoulos, G., Athanasouli, F. et al. Postoperative complications after endoscope-assisted transsphenoidal surgery for pituitary adenomas: a case series, systematic review, and meta-analysis of the literature. Hormones 21, 487–499 (2022). https://doi.org/10.1007/s42000-022-00362-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-022-00362-1