Abstract
Purpose
CSF diversion is a recognised intervention in idiopathic intracranial hypertension (IIH), particularly in the presence of vision-threatening papilledema. Although ventriculo-atrial (VA) shunt insertion is a routine neurosurgical procedure, ventriculoperitoneal and lumboperitoneal shunts have been mostly used in this particular indication. This study aims to look at a single centre’s experience with VA shunts in idiopathic intracranial hypertension (IIH).
Methods
Retrospective case series with a review of electronic records over a 10-year period; exclusion criteria were duplication of same shunt insertion, no VA shunt insertion, paediatric patients and indication other than IIH. Notes were reviewed for demographics, shunt survival (defined by time prior to revision) and reasons for revision.
Results
Eight VA shunt procedures were identified in 6 patients (mean age at insertion 34 ± 10 years) with a mean follow-up of 58 ± 25 months. All shunts were secondary procedures; 2 revisions from lumbo-pleural, 2 from ventriculopleural, 2 from ventriculoatrial and one each from ventriculoperitoneal and combined lumbo-/ventriculoperitoneal. At 50 months, 75% of VA shunts had survived, compared to only 58.3% of VPleural shunts in patients with IIH. Revisions were required due to acute intracranial bleed (1 case)—revised at day 1, and thrombus at distal site (1 case)—revised at day 57. Both shunts were later reinserted. From the latest clinic letters, all patients had their treatment optimised with this procedure, although only two patients had documented resolved papilloedema post-procedure.
Conclusions
Ventriculo-atrial shunts are a safe and efficacious alternative option for CSF diversion in IIH. In this series, only 1 shunt was revised for a VA shunt-specific complication.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Idiopathic intracranial hypertension (IIH) is characterised by the presence of raised intracranial pressure (ICP) in the absence of hydrocephalus or a space-occupying lesion with a normal cerebrospinal fluid (CSF) composition [1, 2]. It typically affects obese women of childbearing age [3,4,5]. Symptoms can be debilitating and include headaches, pulsatile tinnitus, and visual disturbances—most commonly transient visual obscurations [6]. Additionally, it carries a risk of potentially irreversible visual loss [7, 8]. When sight is threatened, current UK guidelines recommend the use of CSF diversion or optic nerve sheath fenestration [9].
Unfortunately, due to the frequent comorbidity with other headache disorders, CSF diversion does not always control headache symptoms [10,11,12]. National guidelines recommend the insertion of a ventriculoperitoneal (VP) shunt where CSF diversion is indicated for IIH [9]. CSF diversion shunts are considered efficacious when there is a differential pressure between the proximal and distal end; when associated with high body mass index, IIH causes raised intra-abdominal pressure, thus potentially reducing this pressure gradient. This may lead to a lack of effective CSF drainage in IIH patients undergoing VP shunt insertion. Moreover, complications (CSF pseudocyst formation, abscess, adhesions, peritonitis, perforation and distal tip migration) [13,14,15], contraindications such as raised intra-abdominal pressure states (e.g. pregnancy) and adhesions from previous surgery may require alternative distal sites of a shunt. The most common options include the pleural cavity in ventriculo-pleural (VPleural) shunts and the right atrium in ventriculo-atrial (VA) shunts.
Gap of knowledge
We have previously reported outcomes from a series of 5 IIH patients undergoing 7 VPleural shunt insertions at our centre, with a complication rate of 28.6% and a median shunt survival of 71.7% at 7 months [16]. However, the efficacy and complication rates of VA shunts in IIH have not yet been explored in detail in the literature. Al-Schameri and colleagues reported a single-centre cohort study of 255 patients undergoing VA shunt, 8 of whom had IIH [17]. However, there was no further subgroup analysis on outcomes for these IIH patients. The right atrium may theoretically be a more optimal distal site in IIH given that the right atrial pressure is more predictably 2–6 mmHg, allowing maintenance of the pressure gradient. Hence, the present study reports a single centre’s experience with VA shunts in IIH, survival of shunts, complications and efficacy.
Methods and materials
Study design
A single-centre retrospective case series of adult patients with VA shunts inserted for IIH, identified from electronic records, over a 10-year time frame (6 August 2013 to 6 August 2023).
Participants
Inclusion criteria were (1) patients aged over 18 years when the VA shunt was inserted, (2) with a diagnosis of IIH as an indication of CSF diversion. All patients with alternative indications for CSF diversion, and patients under 18, were excluded. Demographic and clinical data collected included age, sex, number with a primary VA shunt, number with a secondary VA shunt (and previous VP or VPleural shunts) and the indication for VA shunt insertion.
Outcome
Outcome data collected included time to VA shunt revision, number of revisions, indication for revisions and need for shunt adjustment and clinical outcomes, including headache management and neuro-ophthalmology review.
Ventriculo-atrial shunt placement and technique
Ventriculo-atrial shunt insertion is a joint neurosurgery and interventional neuroradiology procedure at our centre. Under a general anaesthetic, the patient is positioned supine with their head on a horseshoe headrest. The ventricular catheter is placed in an identical fashion to regular VP shunt insertion. Using intraoperative ultrasound, usually with the assistance of interventional radiology, the internal jugular vein is identified, punctured and dilated to feed a guidewire to the right atrium. A distal catheter is then passed over the wire using a Seldinger technique. Using contrast media and intraoperative fluoroscopy, the destination of the distal tubing is determined, ensuring it is sitting within the superior cavo-atrial junction. Subcutaneous closure is performed with 2–0 Vicryl Plus (fast-absorbing polyglactin 910, Ethicon, Johnson and Johnson Medical Ltd.). The skin is closed with staples. Post-operative skull and anteroposterior and lateral chest radiograph are obtained to confirm that the distal catheter is optimally placed along the superior cavo-atrial junction.
Statistical analysis
Shunt failure (end of survival) was defined as the time point at which the shunt had to be revised or removed. Survival analysis was performed using the Kaplan–Meier curves and the log-rank (Cox-Mantel) test. All statistical tests were performed on GraphPad Prism 6.0c.
Results
Patient characteristics
A total of 8 VA shunts were inserted with the intention to manage IIH symptoms between August 2013 and April 2023. These 8 procedures were performed in 6 patients. All patients identified were female with a mean age of 34 (range 19–46). All had had one previous type of shunt prior to VA shunt insertion, with three patients trialling more than one type of shunt.
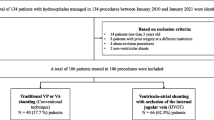
Shunt survival
Of the 8 VA shunts inserted, one was removed on day 1 post-operatively due to an acute intracranial haemorrhage, later being re-inserted with no complications after 5 years and 8 months of follow-up at the time of the study. Moreover, one shunt was revised on day 57 due to a distal thrombus. At 50 months, 75% of VA shunts had survived (Fig. 1).
Efficacy
Of the 6 patients, 3 markers were used to measure the efficacy of the shunts: ophthalmological assessment, symptom control and number of shunt adjustments.
Some ophthalmological assessments occurred in patients’ local hospitals; therefore, full data was not available. Two patients had documented the resolution of papilloedema. On follow-up, each patient had an improvement in headache, vision, or both symptoms. Moreover, each patient had at least 1 shunt adjustment.
Discussion
Study findings
VA shunting is known to be safe and as effective as other CSF shunting techniques for obstructive hydrocephalus and normal pressure hydrocephalus [17,18,19,20]. Hung and colleagues have even recommended VA shunting as a primary treatment for normal pressure hydrocephalus (NPH) [19].
However, there is little published data for the safety and efficacy of VA shunts specifically in the context of IIH. This study is the first to report on this cohort, and we demonstrate that VA shunts can be used as a valid second- or third-line treatment for IIH and indeed is quite effective at controlling symptoms. When compared to a series of patients undergoing VPleural shunt for IIH at our centre, 75% of VA shunts survived at 50 months, compared to 58.3% of VPleural shunts (N = 7) [16]. Whilst 2 shunts required removal, in both cases, they were later able to be replaced without subsequent complications on follow-up. It is of note that the acute intracranial bleed is a risk with all ventricular shunts regardless of distal site and therefore is not specific to VA shunts.
VA shunts for symptom control in IIH
In this cohort, VA shunts provided good long-term control of symptoms of IIH, with two patients each having evidence of resolved papilloedema and superior control of headache symptoms.
The effective symptom control may owe to the relatively higher distal CSF pressures. Pressure in the right atrium is around 2–6 mmHg, higher than pressures within the peritoneal cavity (0–5 mmHg) and the pleural space (− 3.5 mmHg). It is possible that these higher pressures are more physiological for an IIH patient who, often for years, has tolerated raised ICP. Furthermore, a higher distal pressure may reduce over-drainage and siphoning, a problem that occurs in VPleural shunts [16].
VA shunt safety in IIH
Despite our small cohort having a good safety profile, VA shunts are not without their well-reported and significant complications. Distal site-specific complications include obstruction, infection, thrombus formation, pulmonary emboli, pulmonary hypertension and shunt nephritis [21, 22]. There were no significant distal complications in our study, although this was a small cohort. The intracranial haemorrhage observed is not specific to VA shunts. The literature on outcome and safety profiles of VA and VPleural shunts in IIH patients is scarce, but six studies are presented in Table 1.
All studies on VA shunt insertion included IIH patients within the larger surgical cohort without further subgroup analysis, therefore precluding useful comparison to the present study. In Johnston et al.’s study, one patient underwent a secondary VA shunt insertion after persistent infection with valved lumboperitoneal and cisternoatrial shunts. However, this did not function satisfactorily and was removed after two revisions, being replaced with a cisternoatrial shunt [23]. Three studies described ultrasound-guided VA shunt insertion in a total of 11 patients [24,25,26], two of which described no peri-procedural complications [24,25,26]. Although complications arising from VA shunt insertion were described in these articles, this was not disaggregated to IIH patients’ outcomes. In Craven et al.’s study, 5 IIH patients had a VPleural shunt, with two revisions required due to unresolved symptoms [16]. The rate of shunt survival in this VPleural cohort is less than in our study with the VA cohort, but rates of complication, revision and symptom control are the same.
Study strengths and limitations
Although this cohort is small, the findings are encouraging and conducting this study at a larger scale would be beneficial. The longest follow-up in this study was 6 years 8 months, which is long enough for late complications to manifest.
Conclusion
Insertion of a VA shunt for IIH was efficacious for the management of our patients’ ICP, and symptoms were largely well controlled. One significant distal site-specific complication was noted; however, given the small cohort, the applicability of this to the IIH cohort at large is unclear. They remain a safe and effective second-line option where alternative distal sites have failed or are contraindicated and may also be considered first-line due to the reduced differential pressure gradient in the right atrium compared to the peritoneum in IIH.
Data availability
All data in this article is available on request.
Code availability
Not applicable.
References
Portelli M, Papageorgiou PN (2017) An update on idiopathic intracranial hypertension. Acta Neurochir (Wien) 159(3):491–499
Smith JL (1985) Whence pseudotumor cerebri? J Clin Neuroophthalmol 5(1):55–56
Biousse V, Bruce BB, Newman NJ (2012) Update on the pathophysiology and management of idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatr 83(5):488–494
Kilgore KP, Lee MS, Leavitt JA, Mokri B, Hodge DO, Frank RD, Chen JJ (2017) Re-evaluating the incidence of idiopathic intracranial hypertension in an era of increasing obesity. Ophthalmology 124(5):697–700
Radhakrishnan K, Thacker AK, Bohlaga NH, Maloo JC, Gerryo SE (1993) Epidemiology of idiopathic intracranial hypertension: a prospective and case-control study. J Neurol Sci 116(1):18–28
Wall M, Kupersmith MJ, Kieburtz KD et al (2014) The idiopathic intracranial hypertension treatment trial: clinical profile at baseline. JAMA Neurol 71(6):693–701
Best J, Silvestri G, Burton B, Foot B, Acheson J (2013) The incidence of blindness due to idiopathic intracranial hypertension in the UK. Open Ophthalmol J 7:26–29
Thambisetty M, Lavin PJ, Newman NJ, Biousse V (2007) Fulminant idiopathic intracranial hypertension. Neurology 68(3):229–232
Mollan SP, Davies B, Silver NC et al (2018) Idiopathic intracranial hypertension: consensus guidelines on management. J Neurol Neurosurg Psychiatr 89(10):1088–1100
deSouza R-M, Toma A, Watkins L (2015) Medication overuse headache - an under-diagnosed problem in shunted idiopathic intracranial hypertension patients. Br J Neurosurg 29(1):30–34
Friedman DI, Quiros PA, Subramanian PS, Mejico LJ, Gao S, McDermott M, Wall M, and the NORDIC IIHTT Study Group (2017) Headache in idiopathic intracranial hypertension: findings from the idiopathic intracranial hypertension treatment trial. Headache 57(8):1195–1205
Thurtell MJ, Wall M (2013) Idiopathic intracranial hypertension (pseudotumor cerebri): recognition, treatment, and ongoing management. Curr Treat Options Neurol 15(1):1–12
Allouh MZ, Al Barbarawi MM, Asfour HA, Said RS (2017) Migration of the distal catheter of the ventriculoperitoneal shunt in hydrocephalus: a comprehensive analytical review from an anatomical perspective. Clin Anat 30(6):821–830
Chung J-J, Yu J-S, Kim JH, Nam SJ, Kim M-J (2009) Intraabdominal complications secondary to ventriculoperitoneal shunts: CT findings and review of the literature. AJR Am J Roentgenol 193(5):1311–1317
Rinker EK, Williams TR, Myers DT (2015) CSF shunt complications: what the abdominal imager needs to know. Abdom Imaging 40(6):2030–2040
Craven C, Asif H, Farrukh A, Somavilla F, Toma AK, Watkins L (2017) Case series of ventriculopleural shunts in adults: a single-center experience. J Neurosurg 126(6):2010–2016
Al-Schameri AR, Hamed J, Baltsavias G, Winkler P, Machegger L, Richling B, Emich S (2016) Ventriculoatrial shunts in adults, incidence of infection, and significant risk factors: a single-center experience. World Neurosurg 94:345–351
Giordan E, Palandri G, Lanzino G, Murad MH, Elder BD (2018) Outcomes and complications of different surgical treatments for idiopathic normal pressure hydrocephalus: a systematic review and meta-analysis. J Neurosurg 131(4):1024–1036
Hung AL, Vivas-Buitrago T, Adam A, Lu J, Robison J, Elder BD, Goodwin CR, Jusué-Torres I, Rigamonti D (2017) Ventriculoatrial versus ventriculoperitoneal shunt complications in idiopathic normal pressure hydrocephalus. Clin Neurol Neurosurg 157:1–6
Niu H, Wu H, Luo W, Wang K, Zhao L, Wang Y (2021) Ventriculoatrial shunt as a feasible regimen for certain patients of hydrocephalus: clinical features and surgical management. Acta Neurol Belg 121(2):403–408
Hanak BW, Bonow RH, Harris CA, Browd SR (2017) Cerebrospinal fluid shunting complications in children. Pediatr Neurosurg 52(6):381–400
Vernet O, Rilliet B (2001) Late complications of ventriculoatrial or ventriculoperitoneal shunts. Lancet 358(9293):1569–1570
Johnston I, Besser M, Morgan MK (1988) Cerebrospinal fluid diversion in the treatment of benign intracranial hypertension. J Neurosurg 69(2):195–202
Sheth SA, McGirt M, Woodworth G, Wang P, Rigamonti D (2009) Ultrasound guidance for distal insertion of ventriculo-atrial shunt catheters: technical note. Neurol Res 31(3):280–282
Metellus P, Hsu W, Kharkar S, Kapoor S, Scott W, Rigamonti D (2009) Accuracy of percutaneous placement of a ventriculoatrial shunt under ultrasonography guidance: a retrospective study at a single institution. J Neurosurg 110(5):867–870
McCracken JA, Bahl A, McMullan J (2016) Percutaneous ultrasound-guided insertion of ventriculo-atrial shunts. Br J Neurosurg 30(4):411–413
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was conducted as a service evaluation at the National Hospital for Neurology & Neurosurgery and therefore did not require ethical approval.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
As there are no patient-identifiable data in this article; separate consent to publish was not sought.
Conflict of interest
AKT’s research time was supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre. LDW has received honoraria from and served on advisory boards for Medtronic, B. Braun and Codman. SM is an NIHR-funded Academic Clinical Fellow.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sheikh M. B. Momin and Sophie R. Mullins are joint first authors of this work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Momin, S.M.B., Mullins, S.R., Craven, C.L. et al. Ventriculo-atrial shunt in idiopathic intracranial hypertension. Acta Neurochir 166, 98 (2024). https://doi.org/10.1007/s00701-024-05985-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-05985-4