Abstract
Purpose
Pedicle subtraction osteotomy (PSO) as an invasive procedure with high reoperation and complication rates in an often elderly population has often been questioned. The purpose of our study was to evaluate the impact of PSO for sagittal imbalance (SI) on patient-reported outcomes including self-reported satisfaction and health-related quality of life 2 years postoperatively.
Methods
Consecutive patients who underwent correction of their spinal deformity by thoracolumbar PSO were assessed using self-reporting questionnaires 2 years postoperatively. Outcome was measured by visual analogue scale (VAS) for back and leg pain, Oswestry Disability Index (ODI), and EQ-5D scores. Additionally, a Patient Satisfaction Index (PSI) rated in four grades (A: very satisfied to D: not satisfied), walking range, and the Timed Up and Go (TUG) Test were evaluated.
Results
Sixty-five patients were included, and each parameter was assessed preoperatively and 24 months postoperatively. The intervention led to significant improvements in back pain (8.1 ± 1.2 vs. 2.9 ± 1.9; p < 0.001), as well as ODI scores (57.7 ± 13.9 vs. 32.6 ± 18.9; p < 0.001), walking range (589 ± 1676 m vs. 3265 ± 3405 m; p < 0.001), and TUG (19.2 s vs. 9.7 s; p < 0.05). 90.7% of patients (n = 59/65) reported a PSI grade “A” or “B” 24 months postoperatively.
Conclusion
Patient satisfaction 24 months after PSO for SI is high. Quality of life improved significantly by restoring sagittal balance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
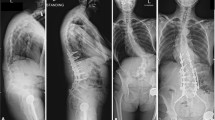
Sagittal imbalance (SI) is commonly related to adult spinal deformity. Etiologies include primary deformity, such as scoliosis (degenerative and idiopathic), as well as secondary deformity, i.e., posttraumatic kyphosis and iatrogenic flat back syndrome. In the last decade, SI became a well-known cause of severe back pain and decreasing mobility, resulting in low health-related quality of life. Furthermore, patients commonly experience severe functional disability. As conservative treatment options fail in most patients, surgical interventions aiming to restore sagittal balance have increasingly gained importance [3]. Correction is typically accomplished by extensive instrumentation, frequently combined with osteotomy. While the surgical procedure has to be adapted to the amount of correction, pedicle subtraction osteotomy (PSO) is one of the most commonly performed interventions and results in sagittal correction of about 30° [13]. The PSO procedure was first described in 1985, aiming to correct kyphotic spinal deformities and was originally used in the ankylosed spine [25]. The principle is a closed wedge osteotomy with shortening of the dorsal structures, obtained by resection of the lamina, the facet joints, and the pedicles or the additional resection of the superior disc. Although the method is technically challenging, previous studies reported satisfactory clinical outcomes and improved quality of life by restoring sagittal alignment [2, 4, 13, 14, 16]. PSO and PSOplus (meaning an additional discectomy in the proximal adjacent level of the PSO) according to the classification of Schwab grades 3 and 4 [19] as invasive procedures with high reoperation and complication rates in an often elderly population have often been criticized and the benefit for the patients has been questioned [1, 6, 13]. Studies focusing on patient self-reported outcome after implementation of PSO for SI are lacking. Therefore, the purpose of this study was to investigate patient satisfaction and health-related quality of life (HRQOL) in patients suffering from SI and treated by a PSO.
Material and methods
Patient data
This study presents data from a prospective observational patient registry. Clinical management was not delayed or altered by participation in this study. The study was approved by the Local Ethics Committee (AN2014-0234) in accordance with the ethical principles originating from the Declaration of Helsinki and in compliance with Good Clinical Practice. Sixty-five consecutive patients, who underwent PSO or PSOplus in the thoracolumbosacral spine for SI between January 2011 and May 2018 at the authors’ institution, were enrolled. A full data set was obtained in all patients. Indication for surgery was determined in an interdisciplinary spinal case conference. The spino-pelvic parameters were assessed according to the FBI method of Le Huec et al. [13]. All patients were postoperatively observed and monitored for at least 24 h at the IMCU/ICU. Orthoses were not systematically prescribed. Demographic data as well as preoperative and postoperative clinical parameters were collected using the patient’s electronic chart. Furthermore, the occurrence of intraoperative and perioperative complications, as well as causes for revision surgery within 24 months postoperatively, was documented.
Patient-reported outcome
Patient-reported outcome measures included visual analogue scale (VAS) for leg and back pain, Oswestry Disability Index (ODI), and EQ-5D-5L plus EQ-5D-VAS. The ODI is a widely used, simple, and quick condition-specific outcome measure in patients with spinal disorders. Zero to 20% indicate minimal disability, 20–40% moderate disability, 40–60% severe disability, 60–80% very serious disability, and 80–100% bed-bound disability [24]. The EQ-5D-5L is a simple re-runnable questionnaire, which is composed of five questions regarding mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The EQ-5D index, calculated from a specific algorithm, is subsequently subtracted from 1.000. The EQ-5D-VAS thermometer asks patients to mark their health status (0–100) on the day of the assessment [18]. Furthermore, walking range (in meters), Timed Up and Go Test (TUG in seconds [s]) [8], representing a performance-based functional test, objectively quantifying the physical ability of walking, and the NASS Patient Satisfaction Index (PSI) rated in four grades (A: very satisfied to D: not satisfied) were assessed [7]. Scores were obtained preoperatively and 3 months, 12 months, and 24 months postoperatively. All clinical outcome measures were determined during routine outpatient visits by the patients with assistance of a study nurse if necessary.
Surgical procedure
Patients were placed in a prone position after induction of general anesthesia with the goal to place the vertebral body to be osteotomized directly at the pivot point of the operating table [10]. Standard posterior exposure of the spine was realized and bony structures were fully visible. Pedicle screws were placed in a standardized manner, at least two levels above and two levels below the aimed PSO level. If necessary, Smith-Petersen Osteotomy (SPO) [23] and transforaminal lumbar interbody fusion (TLIF) were performed at additional levels. A laminectomy with cranio-caudal undercutting at the index level was performed according to the classification of Schwab et al. [19]. Additionally, the transverse process of the osteotomized level and the facet joints of the remaining adjacent and instrumented segments were resected. Pedicles were then opened by using multiple specific dilators. Cancellous bone was progressively pushed anteriorly to create a solid anterior fusion mass. Pedicles were resected with differently shaped osteotomes (PSO Osteotomy Set, Medtronic, Dublin, Ireland). If necessary, the adjacent superior disc was removed (PSOplus). The posterior vertebral wall was resected in two steps with a special posterior wall impactor. The osteotomy was then closed in a gentle manner by adjustment of the OR table hinge remote controlled and under continuous visualization of the dural sac and the descending nerve roots [10]. One or two satellite rods were usually inserted to span the osteotomy [21].
Statistical analysis
All patients with complete initial data were considered for the retrospective analysis. Continuous variables are expressed by mean ± standard deviation (SD). The Kolmogorov–Smirnov test was used for testing normal distribution. The unpaired Student t-test and Mann–Whitney U test were performed to analyze differences in clinical and demographic characteristics and in clinical outcome variables. Frequencies were compared by the chi-square and Fisher’s exact tests. A p-value < 0.05 was considered as statistically significant. All statistical evaluations were performed with SPSS Version 21.0 (IBM Corp. Released 2012. IBM SPSS Statistics for Mac OS X, Version 21.0, NY: IBM Corp.). Figures and tables were designed using Microsoft Excel (Version 15.36 for Mac OS X, Microsoft Corporation 2017, Redmond, USA).
Results
Clinical details
The data of sixty-five prospectively included patients matching the inclusion criteria and completing their 24-month follow-up were analyzed. Demographic details and patient characteristics are outlined in Table 1. Thirteen patients (20%) experienced intraoperative complications, with 11/13 cases (84.6%) of incidental durotomy and 2/13 cases (15.4%) of extensive blood loss (> 5000 mL). Eleven patients (16.9%) demonstrated perioperative complications: 2/11 (3.1% overall) developed a superficial wound infection, 4/11 (6.2% overall) experienced a postoperative thrombosis, and 5/11 (7.7%) demonstrated postoperative neurological worsening. Within 24 months, 4/65 patients (6.2%) were treated for proximal junction kyphosis (PJK), whereas 6/65 patients (9.2%) received revision surgery due to hardware failure.
Self-reported, health-related quality of life
The VAS for back and leg pain demonstrated significantly lower values comparing pre- to 24-month postoperative data (81 ± 12 vs. 29 ± 19; p < 0.001; 46 ± 29 vs. 20 ± 22; p < 0.001; respectively; Fig. 1). Surgery also significantly improved ODI scores (57.7 ± 13.9 vs. 32.6 ± 18.9; p < 0.001; Fig. 2) and EQ-5D values (0.48 ± 0.21 vs. 0.67 ± 0.26; p = 0.028; Fig. 3). The self-reported health state, as a part of the EQ-5D evaluation, demonstrated lower values during the postoperative course, but no statistically significant differences (50.6 ± 21.5 vs. 61.6 ± 15.8; p = 0.109). The patient-reported walking range and the TUG test improved significantly in the period between the preoperative and 24-month postoperative evaluation (589 ± 1676 m vs. 3265 ± 3405 m; p < 0.001 and 19.2 s vs. 9.7 s; p = 0.017; respectively; Fig. 4). 90.7% of patients (n = 59/65) reported a PSI grade “A” or “B” 24 months postoperatively, i.e., they would have the operation performed once again with the same outcome (Fig. 5). A correlating trend of worse preoperative and improved postoperative scores could be shown (p = 0.161). There was no correlation of sex or gender and HRQOL outcome.
Distribution of the PSI 24 months postoperatively. A: Surgery met my expectations; B: Surgery improved my condition enough so that I would go through it again with the same outcome; C: surgery helped me but I would not go through it again for the same outcome; D: I am the same or worse compared to before surgery
Discussion
The prospective evaluation of health-related quality of life 24 months after PSO for SI demonstrated excellent improvement of quality of life, pain, and functionality. Patient satisfaction was very high, as 90.7% of patients were satisfied with their outcome 2 years postoperatively.
A direct correlation between low HRQOL and SI has already been described [15]. Causes for this and main indications for deformity correction surgery include significant functional impairment and intractable pain. Spinal osteotomies seem to be effective methods in restoring sagittal balance and improving HQOL in patients with severe thoraco-lumbar deformities [2, 13, 14]. Their use, however, has often been criticized due to a relatively high complication rate in an elderly population. Nevertheless, there is a lack of studies reporting on the patient self-reported HRQOL and on patient satisfaction following thoracolumbar PSO for SI.
Complications
Numbers presented in this study are comparable to recently published data, where intraoperative and perioperative complications are reported in up to 55%, mostly independent from the surgeon’s experience [1, 6, 20]. This may be explained by the fact that most patients receiving treatment for SI are over 50 years of age and commonly had prior surgery [6]. Perioperative complication rates and causes, as well as the incidence of hardware failure and PJK, coincide with recent reports [5, 22]. According to these findings, the indication for such an invasive operation should be comprehensively evaluated and the patients should be well informed before surgery. This is particularly applicable in patient cohorts like the treated group, characterized by advanced age and a significantly higher risk due to often multiple previous operations.
Improvement of pain
We could demonstrate a significant improvement of pain, and the minimal clinical important difference (MCID) of at least 28 points was reached immediately [17]. This coincides with previous reports, where realignment surgery has been shown to improve radicular symptoms as well as back pain [22].
Improvement of disability
Significant improvement could also be demonstrated for ODI, as results improved even more than the reported MCID of 10 points [17]. As a further instrument for quantification, the TUG test showed a significant improvement during the postoperative course. The TUG test represents a performance-based functional test that objectively documents and quantifies the physical ability of walking and is reported to be sensitive and appropriate for assessing postoperative changes after instrumented fusion surgery. The MCID has been reported at 3.4 s [9, 12]. Our results correspond with previous studies, demonstrating that even mild SI may be detrimental for the patient’s functional status, and the correction of the sagittal alignment shows an early and significant improvement [11, 22]. Furthermore, our data may be interpreted to show even better benefit of the surgical procedure, the higher the preoperative disability was rated.
Improvement of health status
EQ-5D-5L values, accounting for the generic health status, showed significant improvement over time, reaching significantly more than the MCID of 0.03 points at 24 months (0.48 ± 0.21 vs. 0.67 ± 0.26) [24]. Similar results could be shown for the EQ-5D-VAS, where patients are asked to rate their subjective health status and clearly reached the previously reported MCID of 10.5 points [24]. Moreover, the individual walking range reported by patients significantly improved over time, showing a nearly sevenfold increase between the preoperative and 24-month postoperative evaluation.
Limitations
Limitations of the study include the small patient cohort, the single-center management and bias, and the short period of follow-up. Nevertheless, our data might well be conclusive, as the majority of complications and re-operations — and the resulting disability — is known to occur within the first 2 years after correction surgery [21].
As the population ages, the rate of surgeries performed for adult spinal deformity will continue to rise. Better understanding of sagittal deformities, technical improvements, and improved preoperative and postoperative care allow these surgeries to become highly complex. This, however, might be associated with a concomitantly increased risk of complications. Despite a reoperation rate of 15.4% and a complication rate of 20% intraoperatively and 16.9% postoperatively, however, more than 90% of patients were satisfied with the procedure.
Conclusion
Despite the complex surgical procedure and a relatively high overall complication rate with PSO to restore sagittal balance, patient satisfaction is high, and quality of life improved significantly 24 months after surgery.
References
Auerbach JD, Lenke LG, Bridwell KH, Sehn JK, Milby AH, Bumpass D et al (2012) Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine 37:1198–1210. https://doi.org/10.1097/BRS.0b013e31824fffde
Boissière L, Takemoto M, Bourghli A, Vital J-M, Pellisé F, Alanay A et al (2017) Global tilt and lumbar lordosis index: two parameters correlating with health-related quality of life scores—but how do they truly impact disability? Spine J 17:480–488. https://doi.org/10.1016/j.spinee.2016.10.013
Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A et al (2003) Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine 28:2093–2101. https://doi.org/10.1097/01.BRS.0000090891.60232.70
Cho K-J, Bridwell KH, Lenke LG, Berra A, Baldus C (2005) Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine 30:2030–2037. https://doi.org/10.1097/01.brs.0000179085.92998.ee
Choi HY, Hyun S-J, Kim K-J, Jahng T-A, Kim H-J (2020) Radiographic and clinical outcomes following pedicle subtraction osteotomy : minimum 2-year follow-up data. J Korean Neurosurg Soc 63:99–107. https://doi.org/10.3340/jkns.2018.0170
Daubs MD, Brodke DS, Annis P, Lawrence BD (2016) Perioperative complications of pedicle subtraction osteotomy. Glob Spine J 6:630–635. https://doi.org/10.1055/s1570088
Fairbank JCT, Pynsent PB (2000) The Oswestry Disability Index. Spine 25:2940–2953. https://doi.org/10.1097/00007632-200011150-00017
Gautschi OP, Corniola MV, Schaller K, Smoll NR, Stienen MN (2014) The need for an objective outcome measurement in spine surgery–the timed-up-and-go test. Spine J 14(10):2521–2522. https://doi.org/10.1016/j.spinee.2014.05.004
Gautschi OP, Stienen MN, Corniola MV, Joswig H, Schaller K, Hildebrandt G et al (2017) Assessment of the minimum clinically important difference in the timed up and go test after surgery for lumbar degenerative disc disease. Neurosurgery 80:380–385. https://doi.org/10.1227/NEU.0000000000001320
Girod P-P, Kögl N, Molliqaj G, Lener S, Hartmann S, Thomé C (2022) Flexing a standard hinge-powered operating table for lumbosacral three-column osteotomy (3-CO) site closure in 84 consecutive patients. Neurosurg Rev 45:517–524. https://doi.org/10.1007/s10143-021-01559-5
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine 30:682–688. https://doi.org/10.1097/01.brs.0000155425.04536.f7
Hartmann S, Hegewald AA, Tschugg A, Neururer S, Abenhardt M, Thomé C (2016) Analysis of a performance-based functional test in comparison with the visual analog scale for postoperative outcome assessment after lumbar spondylodesis. Eur Spine J 25:1620–1626. https://doi.org/10.1007/s00586-015-4350-y
Le Huec J-C, Faundez A, Dominguez D, Hoffmeyer P, Aunoble S (2015) Evidence showing the relationship between sagittal balance and clinical outcomes in surgical treatment of degenerative spinal diseases: a literature review. Int Orthop (SICOT) 39:87–95. https://doi.org/10.1007/s00264-014-2516-6
Kim K-T, Lee S-H, Suk K-S, Lee J-H, Jeong B-O (2012) Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine 37:1667–1675. https://doi.org/10.1097/BRS.0b013e3182552fd0
Lee S-H, Son E-S, Seo E-M, Suk K-S, Kim K-T (2015) Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. The Spine J 15:705–712. https://doi.org/10.1016/j.spinee.2013.06.059
Obeid I, Bourghli A, Boissière L, Vital J-M, Barrey C (2014) Complex osteotomies vertebral column resection and decancellation. Eur J Orthop Surg Traumatol 24:49–57. https://doi.org/10.1007/s00590-014-1472-6
Patel M, Newey M, Sell P (2013) Minimal clinical important differences in spinal surgery. Orthop Proc 95-B:15–15. https://doi.org/10.1302/1358992X.95BSUPP_4.SBPR2011-015
Podsiadlo D, Richardson S (1991) The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Schwab F, Blondel B, Chay E, Demakakos J, Lenke L, Tropiano P et al (2014) The comprehensive anatomical spinal osteotomy classification. Neurosurgery 74:112–120. https://doi.org/10.1227/NEU.0000000000000182o
Sciubba DM, Yurter A, Smith JS, Kelly MP, Scheer JK, Goodwin CR et al (2015) A comprehensive review of complication rates after surgery for adult deformity: a reference for informed consent. Spine Deformity 3:575–594. https://doi.org/10.1016/j.jspd.2015.04.005
SeyedVosoughi A, Joukar A, Kiapour A, Parajuli D, Agarwal AK, Goel VK et al (2019) Optimal satellite rod constructs to mitigate rod failure following pedicle subtraction osteotomy (PSO): a finite element study. Spine J 19:931–941. https://doi.org/10.1016/j.spinee.2018.11.003
Smith JS, Shaffrey CI, Berven S, Glassman S, Hamill C, Horton W et al (2009) Operative versus nonoperative treatment of leg pain in adults with scoliosis: a retrospective review of a prospective multicenter database with two-year follow-up. Spine 34:1693–1698. https://doi.org/10.1097/BRS.0b013e3181ac5fcd
Smith-Petersen MN, Larson CB, Aufranc OE (1969) Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res 66:6–9
Soer R, Reneman MF, Speijer BLGN, Coppes MH, Vroomen PCAJ (2012) Clinimetric properties of the EuroQol-5D in patients with chronic low back pain. Spine J 12:1035–1039. https://doi.org/10.1016/j.spinee.2012.10.030
Thomasen E (1985) Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res 194:142–152
Funding
Open access funding provided by University of Innsbruck and Medical University of Innsbruck.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Girod, PP., Lener, S., Kögl, N. et al. Health-related quality of life 2 years after pedicle subtraction osteotomy for sagittal imbalance: a single-center experience of 65 patients. Acta Neurochir 165, 3521–3527 (2023). https://doi.org/10.1007/s00701-023-05787-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05787-0