Abstract
Background
The optimal surgical procedure to reduce the recurrence rate of chronic subdural hematoma (CSDH) after burr-hole surgery remains to be established. This study aimed to investigate the association between artificial cerebrospinal fluid (ACF) use during burr-hole surgery and reoperation rate in patients with CSDH.
Method
In this retrospective cohort study, we used the Japanese Diagnostic Procedure Combination inpatient database. We identified patients aged 40–90 years who were hospitalized for CSDH and had undergone burr-hole surgery within 2 days of admission, between July 1, 2010 and March 31, 2019. We performed a one-to-one propensity score-matched analysis to compare the outcomes between patients with and without ACF irrigation during burr-hole surgery. The primary outcome was reoperation within 1 year of surgery. The secondary outcome was the total hospitalization costs.
Results
Of the 149,543 patients with CSDH from 1100 hospitals, ACF was used in 32,748 patients (21.9%). Propensity score matching created highly balanced 13,894 matched pairs. In the matched patients, the reoperation rate was significantly lower in the ACF users than that in the non-users group (6.3% vs. 7.0%, P = 0.015), with a risk difference of −0.8% (95% confidence interval, −1.5 to −0.2). There was no significant difference in the total hospitalization costs between the two groups (5079 vs. 5042 US dollars, P = 0.330).
Conclusions
ACF use during burr-hole surgery may be associated with lower reoperation rate in patients with CSDH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic subdural hematoma (CSDH) is an old blood collection between the brain surface and dura mater. CSDH is one of the most common neurosurgical conditions encountered. Its incidence is higher in the older population and is rising as the older population increases [12]. The standard treatment for CSDH is a burr-hole surgery. The outcome after burr-hole surgery is generally favorable; however, recurrence rates reportedly range from 4 to 27% [7, 9, 10, 12, 19].
Artificial cerebrospinal fluid (ACF) is an irrigation fluid with a composition akin to that of the human cerebrospinal fluid. Since ACF became commercially available in Japan, they have been used in more than 1000 facilities [1]. ACF is reported to have a hemostatic effect and to minimize cerebrovascular permeability [6, 8]; therefore, the use of ACF as an irrigation solution during burr-hole surgery may improve outcomes in patients with CSDH.
Historical observational studies have reported an association between ACF use during burr-hole surgery and lower recurrence rate in patients with CSDH [1, 9, 21, 22]. However, these were small, single-center studies with insufficient adjustments for confounding factors [1, 9, 21, 22]. Recently, a multicenter randomized controlled trial compared ACF with normal saline as an irrigation solution during burr-hole surgery and found no significant difference in recurrence rate between the two groups [23]. This randomized controlled trial had several limitations [23]. First, it might have been underpowered because of the small sample size. Second, 12% of the participants were lost to follow-up, resulting in an attribution bias. Third, the generalizability of the results is limited because all participating institutions in the study were university hospitals [2]. CSDH is usually treated at general local hospitals, and patients with CSDH treated at university hospitals may differ from those treated at general local hospitals.
To overcome these limitations in the antecedent studies, we aimed to investigate the association between ACF use during burr-hole surgery and the need for reoperation in patients with CSDH, by using a large national database.
Methods
This cohort study used the Japanese Diagnosis Procedure Combination (DPC) inpatient database. The study protocol was approved by the Institutional Review Board of the University of Tokyo (approval number: 3501-3; December 25, 2017). The requirement of informed consent from the patients was waived due to the retrospective nature of this observational study that analyzed de-identified data.
Data source
The DPC database is a nationwide database, which includes administrative claims and discharge abstracts from more than 1200 acute care hospitals. It contains the following patient information: hospital type (teaching or non-teaching), age, sex, body weight, height, smoking history (non-smoker, current/past smoker, unknown), activity of daily living scores and level of consciousness at admission, diagnosis (primary diagnosis and comorbidities at admission), drugs used and surgical procedures performed, total hospitalization cost, and discharge status. The International Classification of Diseases, 10th revision (ICD-10), and Japanese medical procedure codes were used to allocate codes for diagnoses and medical procedures, respectively. This database has been validated previously; the specificity of the diagnoses exceeded 96%, the sensitivity of the diagnoses ranged from 50 to 80%, and both the specificity and sensitivity of procedures exceeded 90% [26]. To obtain information about hospitals (university hospitals or not), we linked the database with the facility information and statistical data from the Survey of Medical Institutions 2016 [13].
Study population
Patients aged 40–90 years who were hospitalized with a primary diagnosis of CSDH (ICD-10 codes: I620, S650) and had undergone first burr-hole surgery for CSDH (Japanese procedure code: K164-2) within 2 days of admission were identified from the database from July 1, 2010 to March 31, 2019. Eligible patients were followed-up for 1 year after the first burr-hole surgery at the same hospital where the surgery was performed.
Patients who received ACF during the first burr-hole surgery were defined as ACF users, and those who did not were defined as ACF non-users.
Outcomes and covariates
The primary outcome was reoperation of burr-hole surgery being performed during the same hospitalization or readmission at the same hospital within a year of the first surgery. The secondary study outcomes were the presence of postoperative complications (intracranial hematomas and central nervous system infections) and the total hospitalization cost for both the initial admission and readmission. Postoperative intracranial hematoma was defined as intracranial hematoma (ICD-10 codes: S064, S065, I620, I621, I629) that developed after admission. Postoperative central nervous system infections include bacterial meningitis (ICD-10 code: G00) and brain abscess (ICD-10 codes: G060, G062) that developed after admission. Hospitalization costs, recorded in Japanese yen, were converted to US dollars at a rate of 110 yen to 1 US dollar.
The covariates included the type of hospital (teaching or not, university hospital or not), hospital volume per year, fiscal years and season of admission day, admission on weekends or at night, ambulance use, age, sex, body mass index, activity of daily living that was converted to the Barthel Index, comorbidities on admission, Charlson comorbidity index (CCI), level of consciousness, and duration from admission to burr-hole surgery (1: surgery on admission day or 2: surgery on the following day). The hospital volume was calculated as the average number of patients with CSDH who underwent burr-hole surgery at each hospital per year. Fiscal years were categorized as 2010–2013, 2014–2016, or 2017–2019. Age was categorized as 40–49, 50–59, 60–69, 70–79, and 80–89 years. Body mass index was classified based on the World Health Organization criteria for Asian population as follows: < 18.5 kg/m2, 18.5–24.9 kg/m2, 25.0–29.9 kg/m2, ≥ 30 kg/m2 [25], and missing data. The Japan Coma Scale (JCS) was used to evaluate the levels of consciousness. The JCS is composed of four main categories: 0 (alert), 1–3 (delirium), 10–30 (somnolence), and 100–300 (coma), which correlated well with the Glasgow Coma Scale [27]. The CCI was calculated based on a validated coding algorithm [16, 17] and was categorized into 0, 1, 2, and ≥ 3. Activities of daily living based on the Barthel Index were categorized as follows: independent (Index 100), moderate dependency (61–99), severe dependency (0–60), and missing data [14].
ACF in Japan
ACF became commercially available in Japan in 2008 (ARTCEREB®; Otsuka Pharmaceutical Co. Ltd., Tokushima, Japan). The composition of ACF (pH, 7.3; Na+, 145 mEq/L; Cl−, 129 mEq/L; Mg+, 2.2 mEq/L; Ca2+, 2.3 mEq/L; HCO3−, 23.1 mEq/L; P, 1.1 mmol/L; and glucose 0.61 g/L) is more alike to human cerebrospinal fluid (pH, 7.3; Na+, 145.5 mEq/L; Cl−, 111.9 mEq/L; Mg+, 2.2 mEq/L; Ca2+, 2.3 mEq/L; HCO3−, 23.1 mEq/L; P, 1.1 mmol/L; and glucose 0.61 g/L) than normal saline (pH, 6.3; Na+, 154 mEq/L; and Cl−, 154 mEq/L) and lactated Ringer solution (pH, 6.0–7.5; Na+, 130 mEq/L; Cl−, 109 mEq/L; Ca2+, 3 mEq/L; and HCO3−, 28 mEq/L) [9, 22].
Statistical analysis
We used propensity score matching analysis to compare the outcomes between ACF users and non-users. The propensity score was estimated using a multilevel logistic regression model with all covariates. In the model, hospital was used as a random effect variable to account for the differences in ACF use among hospitals. ACF users were subsequently matched to non-users based on one-to-one nearest neighbor matching, without replacement, within an allowable caliper width of 20% set at the pooled standard deviation of the logit of the propensity score [3]. The standardized mean differences of covariates were evaluated to assess matching performance. An absolute standardized mean difference of ≥ 0.1 was considered a meaningful imbalance. In matched patients, outcomes between the two groups in the cohort were compared using the Mann–Whitney U test for numeric variables and the chi-squared test for categorical variables. The risk difference with 95% confidence interval (CI) was estimated using a mixed-effects linear regression model. The number needed to treat (NNT) was calculated as the inverse of the absolute risk reduction.
All statistical analyses were performed using R (version 3.6.3; R Foundation for Statistical Computing, Vienna, Austria). All statistical tests were two-sided. Statistical significance was defined as P-value < 0.05 or assessed with the 95% CI.
Results
We identified 149,543 patients from 1100 hospitals who were admitted for CSDH and had undergone the first burr-hole surgery within 2 days of admission (Fig. 1). Of these, 32,748 (21.9%) patients underwent burr-hole surgery using ACF, and 8797 (5.9%) required reoperation within a year after surgery. The distribution of the proportion of ACF users among the hospitals is shown in Fig. 2.
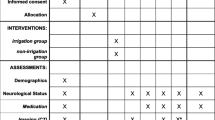
Table 1 summarizes the baseline characteristics of the two groups before and after propensity score matching. Before matching, ACF was more likely to be used in teaching hospitals or lower-volume hospitals. The proportion of surgical sites was imbalanced between the two groups. Propensity score matching selected 13,894 ACF users and 13,894 non-users. After matching, the baseline characteristics were finely balanced between the two groups, with an absolute standardized mean difference of <0.1. In matched patients, the median volume of ACF used during the first burr-hole surgery was 500 mL (interquartile range, 500–1000 mL).
The study outcomes for the matched patients are shown in Table 2. The reoperation rate was significantly lower in the ACF users than that in the non-users (6.3% vs. 7.0%, P = 0.015), with a risk difference of −0.8% (95% CI, −1.5 to −0.2). The estimated NNT was 84 (95% CI, 55 to 178). There was no significant difference in the proportions of postoperative intracranial hematomas (1.0% vs. 0.8%, P = 0.088) or postoperative central nervous system infections (0.1% vs. 0.1%, P = 0.838) and the total hospitalization costs (5079 vs. 5042 US dollars, P = 0.330) between the two groups.
Discussion
Our analysis revealed that ACF use during burr-hole surgery was associated with a significantly lower reoperation rate in patients with CSDH, and there was no significant difference in the hospitalization costs between the ACF users and non-users.
Our results were consistent with those of historical observational studies, though the difference in the reoperation rate between the two groups was much smaller than that previously reported [1, 9]. This discrepancy may be partly explained by the higher recurrence rates in previous studies (15.0% and 23.8%) than in our study (7.0%) and the insufficient adjustment for confounders in the previous studies. The use of a nationwide database enabled us to obtain highly balanced matched patients and derive less-biased results. The most important evidence on this issue is a randomized controlled trial that included 177 ACF users and 165 non-users from ten hospitals in Japan. The study reported a non-significant difference in the recurrence rate after burr-hole surgery for CSDH between the two groups (11.9% vs. 10.9%). However, to detect the observed difference in this study with 80% statistical power and a two-sided type I error rate of 0.05, more than 20,000 samples per group would have been required for a randomized controlled trial. Considering this difficulty, we determined that a large observational study with sufficient adjustment for confounding factors would be ideal as evidence on this issue.
Our findings are consistent with evidence from basic research studies. A study using a mouse model reported that the choice of irrigation solution used in neurosurgical procedures affected the extent of bleeding at the injury site, and ACF irrigation significantly reduced bleeding than normal saline [6]. Calcium is essential for blood coagulation and vascular smooth muscle contraction as they play important roles in hemostasis. The previous study hypothesized that calcium ions included in the ACF may have contributed to the reduced bleeding. A study reported that CSDH membranes irrigated with ACF during burr-hole surgery showed less damage than those irrigated with normal saline; thus, the authors presumed that ACF minimized irritation and promoted healing after surgery [1]. These results suggest that ACF may promote hemostasis of the outer hematoma membrane. In addition, ACF irrigation may reduce recurrence by rinsing out inflammatory mediators from the subdural compartment. Excessive inflammation is one of the main etiological origins of CSDH, and the overproduction of inflammatory mediators is associated with hematoma expansion [5].
Compared to other potential modifications of the surgical procedure to reduce the recurrence rate after burr-hole surgery, ACF use has several advantages. First, it is simple and easy to incorporate in the surgery. Surgeons do not need to change their standard procedure, except for changing the irrigation solution to an ACF. Second, ACF has a favorable safety profile. ACF has a composition that is more similar to that of human cerebrospinal fluid than normal saline. Although normal saline is conventionally used as an irrigation fluid, ACF use is theoretically safer. Studies have reported an association between ACF use during neurosurgery and lower risk of adverse events [15, 23]. Third, ACF is available at a relatively low cost. In Japan, 500 mL of ACF, the median dose used in this study, was available at 16.8 USD. Based on the NNT 84 (95% CI, 55 to 178) in this study, the additional cost needed to reduce one reoperation by changing the irrigation solution from normal saline (1.7 USD for 500 mL) to ACF was calculated to be 1268 (95% CI, 831 to 2688) USD. As this additional cost is presumed to be lower than the hospitalization costs for reoperation [18], ACF use may also be justified in terms of health economics. However, no significant difference in total hospitalization cost in the present study was observed. Further research is needed to clarify this issue.
While ARTCEREB® is not available outside Japan, other types of ACF are in use, such as ACSF (R&D Systems, Inc., Minneapolis, MN, USA) and Elliotts B® Solution (Lukare Medical, LLC, Scotch Plains, NJ, USA). Therefore, our results have clinical implication for surgeons worldwide. Given the aforementioned advantages of ACF, our results suggest that the benefits of ACF use during surgery deserve further consideration. Future prospective trials are needed to confirm our findings and to understand the underlying mechanisms.
Limitations
This study had several limitations. First, it was a retrospective study. We obtained a highly balanced pair cohort; however, biases due to unmeasured confounders were not eliminated. For example, our dataset does not include information on detailed surgical procedures. It is possible that surgeons who used ACF were eager to improve the surgery with active search, and ACF was merely a surrogate indicator of surgical proficiency. Although burr-hole surgery for CSDH is straightforward and surgical techniques to reduce recurrence are not established [11], the difference in surgical techniques may have biased our results. Additionally, information on the temperature [4] and volume [20, 24] of the rinsing solution, which may contribute to recurrence, was not available. Second, causality cannot be directly referred to. Third, the rinsing solution used in the control group was not recorded. Fourth, hospitalizations in one hospital could not be linked to those in another hospital in the database. Based on clinical experience in Japan, we assumed that reoperations were performed at the same hospital, and the likelihood of undergoing reoperation at a different hospital was unrelated to ACF use; however, if these assumptions do not hold, our results could be biased. Finally, our results require external validation in countries with different demographic characteristics and surgical procedures.
Conclusions
ACF use during burr-hole surgery may be associated with lower risk of reoperation in patients with CSDH. Further studies are warranted to confirm our findings and to understand the underlying mechanisms.
References
Adachi A, Higuchi Y, Fujikawa A et al (2014) Risk factors in chronic subdural hematoma: comparison of irrigation with artificial cerebrospinal fluid and normal saline in a cohort analysis. PLoS One 9(8):e103703. https://doi.org/10.1371/journal.pone.0103703
Adachi A, Higuchi Y, Response to Toi et al (2019) Determining if cerebrospinal fluid prevent recurrence of chronic subdural hematoma: a multi-center prospective randomized clinical trial. J Neurotrauma 36(7):1192–1193. https://doi.org/10.1089/neu.2018.5821
Austin PC (2011) An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res 46(3):399–424. https://doi.org/10.1080/00273171.2011.568786
Bartley A, Bartek J Jr, Jakola AS et al (2023) Effect of irrigation fluid temperature on recurrence in the evacuation of chronic subdural hematoma: a randomized clinical trial. JAMA Neurol 80(1):58–63. https://doi.org/10.1001/jamaneurol.2022.4133
Bounajem MT, Campbell RA, Denorme F et al (2021) Paradigms in chronic subdural hematoma pathophysiology: current treatments and new directions. J Trauma Acute Care Surg 91(6):e134–e141. https://doi.org/10.1097/TA.0000000000003404
Fujita Y, Doi K, Harada D, Kamikawa S (2010) Modulation of physiological hemostasis by irrigation solution: comparison of various irrigation solutions using a mouse brain surface bleeding model. J Neurosurg 112(4):824-828. https://doi.org/10.3171/2009.7.JNS09561
Gurelik M, Aslan A, Gurelik B, Ozum U, Karadag O, Kars HZ (2007) A safe and effective method for treatment of chronic subdural haematoma. J Neurosurg 34(1):84–87. https://doi.org/10.1017/s0317167100005849
Koizumi S, Hayasaka T, Goto-Inoue N, Doi K, Setou M, Namba H (2012) Imaging mass spectrometry evaluation of the effects of various irrigation fluids in a rat model of postoperative cerebral edema. World Neurosurg 77(1):153–159. https://doi.org/10.1016/j.wneu.2011.03.039
Kuwabara M, Sadatomo T, Yuki K et al (2017) The effect of irrigation solutions on recurrence of chronic subdural hematoma: a consecutive cohort study of 234 patients. Neurol Med Chir 57(5):210–216. https://doi.org/10.2176/nmc.oa.2016-0228
Laumer R, Schramm J, Leykauf K (1989) Implantation of a reservoir for recurrent subdural hematoma drainage. Neurosurgery 25(6):991–996. https://doi.org/10.1097/00006123-198912000-00026
Liu W, Bakker NA, Groen RJ (2014) Chronic subdural hematoma: a systematic review and meta-analysis of surgical procedures. J Neurosurg 121(3):665–673. https://doi.org/10.3171/2014.5.JNS132715
Mehta V, Harward SC, Sankey EW, Nayar G, Codd PJ (2018) Evidence based diagnosis and management of chronic subdural hematoma: a review of the literature. J Clin Neurosci 50:7–15. https://doi.org/10.1016/j.jocn.2018.01.050
Ministry of Health LaW (2016) Labour and Welfare Statistical Surveys 2016. Japan Ministry of Health [Available from: mhlw.go.jp/stf/seisakunitsuite/bunya/open_data.html
Ohbe H, Sasabuchi Y, Yamana H, Matsui H, Yasunaga H (2021) Intensive care unit versus high-dependency care unit for mechanically ventilated patients with pneumonia: a nationwide comparative effectiveness study. Lancet Reg Health West Pac 13:100185. https://doi.org/10.1016/j.lanwpc.2021.100185
Oka K, Yamamoto M, Nonaka T (1996) Tomonaga M (1996) The significance of artificial cerebrospinal fluid as perfusate and endoneurosurgery. Neurosurgery 38(4):733–736
Quan H, Li B, Couris CM et al (2011) Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173(6):676–682. https://doi.org/10.1093/aje/kwq433
Quan H, Sundararajan V, Halfon P et al (2005) Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care 43(11):1130–1139. https://doi.org/10.1097/01.mlr.0000182534.19832.83
Rauhala M, Helén P, Huhtala H et al (2020) Chronic subdural hematoma-incidence, complications, and financial impact. Acta Neurochir (Wien). 162(9):2033–2043. https://doi.org/10.1007/s00701-020-04398-3
Santarius T, Kirkpatrick PJ, Ganesan D et al (2009) Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: a randomised controlled trial. Lancet 374(9695):1067–1073. https://doi.org/10.1016/S0140-6736(09)61115-6
Tahsim-Oglou Y, Beseoglu K, Hänggi D, Stummer W, Steiger HJ (2012) Factors predicting recurrence of chronic subdural haematoma: the influence of intraoperative irrigation and low-molecular-weight heparin thromboprophylaxis. Acta Neurochir 154:1063–1068. https://doi.org/10.1007/s00701-012-1334-0
Takayama M, Terui K, Oiwa Y (2012) Retrospective statistical analysis of clinical factors of recurrence in chronic subdural hematoma: correlation between univariate and multivariate analysis. No Shinkei geka. Neuro Surg 40(10):871–876
Tatsuya N, Tomo O, Takehiro T, Horoshi O, Tamotsu M (2011) Benefits of Artcereb® on the irrigation of chronic subdural hematoma. Traumatology 34:167–171
Toi H, Fujii Y, Iwama T et al (2019) Determining if cerebrospinal fluid prevents recurrence of chronic subdural hematoma: a multi-center prospective randomized clinical trial. J Neurotrauma 36(4):559–564. https://doi.org/10.1089/neu.2018.5821
Tommiska P, Raj R, Schwartz C et al (2020) Finnish study of intraoperative irrigation versus drain alone after evacuation of chronic subdural haematoma (FINISH): a study protocol for a multicentre randomised controlled trial. BMJ Open 10(6):e038275. https://doi.org/10.1136/bmjopen-2020-038275
WHO Expect Consultation (2004) Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363(9403):157–163. https://doi.org/10.1016/S0140-6736(03)15268-3
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H (2017) Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol 27(10):476–482. https://doi.org/10.1016/j.je.2016.09.009
Yumoto T, Naito H, Yorifuji T, Aokage T, Fujisaki N, Nakao A (2019) Association of Japan Coma Scale score on hospital arrival with in-hospital mortality among trauma patients. BMC Emerg Med 19(1):65. https://doi.org/10.1186/s12873-019-0282-x
Funding
Open access funding provided by The University of Tokyo. This work was supported by grants from the Ministry of Health, Labour and Welfare, Japan (19AA2007 and H30-Policy-Designated-004), and the Ministry of Education, Culture, Sports, Science and Technology, Japan (17H04141).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study protocol was approved by the Institutional Review Board of the University of Tokyo (approval number: 3501-3; December 25, 2017). This study was performed in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The requirement of informed consent from the patients was waived due to the retrospective nature of this observational study that analyzed de-identified data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shibahashi, K., Ohbe, H. & Yasunaga, H. Artificial cerebrospinal fluid use during burr-hole surgery and reoperation rate in patients with chronic subdural hematoma: an analysis using a nationwide inpatient database. Acta Neurochir 165, 1289–1296 (2023). https://doi.org/10.1007/s00701-023-05570-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05570-1