Abstract
Introduction
Elderly patients receiving antithrombotic treatment have a significantly higher risk of developing an intracranial hemorrhage when suffering traumatic brain injury (TBI), potentially contributing to higher mortality rates and worse functional outcomes. It is unclear whether different antithrombotic drugs carry a similar risk.
Objective
This study aims to investigate injury patterns and long-term outcomes after TBI in elderly patients treated with antithrombotic drugs.
Methods
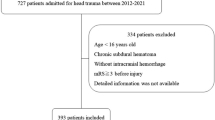
The clinical records of 2999 patients ≥ 65 years old admitted to the University Hospitals Leuven (Belgium) between 1999 and 2019 with a diagnosis of TBI, spanning all injury severities, were manually screened.
Results
A total of 1443 patients who had not experienced a cerebrovascular accident prior to TBI nor presented with a chronic subdural hematoma at admission were included in the analysis. Relevant clinical information, including medication use and coagulation lab tests, was manually registered and statistically analyzed using Python and R. In the overall cohort, 418 (29.0%) of the patients were treated with acetylsalicylic acid before TBI, 58 (4.0%) with vitamin K antagonists (VKA), 14 (1.0%) with a different antithrombotic drug, and 953 (66.0%) did not receive any antithrombotic treatment. The median age was 81 years (IQR = 11). The most common cause of TBI was a fall accident (79.4% of the cases), and 35.7% of the cases were classified as mild TBI. Patients treated with vitamin K antagonists had the highest rate of subdural hematomas (44.8%) (p = 0.02), hospitalization (98.3%, p = 0.03), intensive care unit admissions (41.4%, p < 0.01), and mortality within 30 days post-TBI (22.4%, p < 0.01). The number of patients treated with adenosine diphosphate (ADP) receptor antagonists and direct oral anticoagulants (DOACs) was too low to draw conclusions about the risks associated with these antithrombotic drugs.
Conclusion
In a large cohort of elderly patients, treatment with VKA prior to TBI was associated with a higher rate of acute subdural hematoma and a worse outcome, compared with other patients. However, intake of low dose aspirin prior to TBI did not have such effects. Therefore, the choice of antithrombotic treatment in elderly patients is of utmost importance with respect to risks associated with TBI, and patients should be counselled accordingly. Future studies will determine whether the shift towards DOACs is mitigating the poor outcomes associated with VKA after TBI.

Similar content being viewed by others
References
Asghar M, Adhiyaman V, Greenway MW, Bhowmick BK, Bates A (2002) Chronic subdural haematoma in the elderly–a North Wales experience. J R Soc Med 95(6):290–2
Batchelor JS, Grayson A (2013) A meta-analysis to determine the effect of preinjury antiplatelet agents on mortality in patients with blunt head trauma. Br J Neurosurg 27(1):12–8
Berwaerts J, Webster J (2000) Analysis of risk factors involved in oral-anticoagulant-related intracranial haemorrhages. QJM 93(8):513–21
Bullock RM, Chestnut RM, Clifton LG, Ghajar J, Marion DW, Narayan RK et al (2000) Part 1: guidelines for the management of severe traumatic brain injury. J Neurotrauma 17:499–553
Chestnut RM, Ghajar J, Maas A, Marion DW, Franco S, Teasdale G et al (2000) Part 2: early indicators of prognosis in severe traumatic brain injury. J Neurotrauma 17:555–627
Cohen DB, Rinker C, Wilberger JE (2006) Traumatic brain injury in anticoagulated patients. J Trauma 60(3):553–7
Colombo G, Bonzi M, Fiorelli E, Jachetti A, Bozzano V, Casazza G et al (2021) Incidence of delayed bleeding in patients on antiplatelet therapy after mild traumatic brain injury: a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 29(1):123
Cull JD, Sakai LM, Sabir I, Johnson B, Tully A, Nagy K et al (2015) Outcomes in traumatic brain injury for patients presenting on antiplatelet therapy. Am Surg 81(2):128–32
Depreitere B, Meyfroidt G, Roosen G, Ceuppens J, Grandas FG (2012) Traumatic brain injury in the elderly: a significant phenomenon. Acta Neurochir Suppl 114:289–94
Dossett LA, Riesel JN, Griffin MR, Cotton BA (2011) Prevalence and implications of preinjury warfarin use: an analysis of the national trauma databank. Arch Surg [Internet] 146(5):565–70. https://doi.org/10.1001/archsurg.2010.313
Dunham CM, Hoffman DA, Huang GS, Omert LA, Gemmel DJ, Merrell R (2014) Traumatic intracranial hemorrhage correlates with preinjury brain atrophy, but not with antithrombotic agent use: a retrospective study. PLoS One 9(10):e109473
Dutton RP, Stansbury LG, Leone S, Kramer E, Hess JR, Scalea TM (2010) Trauma mortality in mature trauma systems: are we doing better? An analysis of trauma mortality patterns, 1997–2008. J Trauma 69(3):620–6
Eastridge BJ, Mabry RL, Seguin P, Cantrell J, Tops T, Uribe P et al (2012) Death on the battlefield (2001–2011): implications for the future of combat casualty care. J Trauma Acute Care Surg 73(6 Suppl 5):S431-7
Fakhry SM, Morse JL, Garland JM, Wilson NY, Shen Y, Wyse RJ et al (2021) Antiplatelet and anticoagulant agents have minimal impact on traumatic brain injury incidence, surgery, and mortality in geriatric ground level falls: a multi-institutional analysis of 33,710 patients. J Trauma Acute Care Surg 90(2):215–23
Fang MC, Chang Y, Hylek EM, Rosand J, Greenberg SM, Go AS et al (2004) Advanced age, anticoagulation intensity, and risk for intracranial hemorrhage among patients taking warfarin for atrial fibrillation. Ann Intern Med 141(10):745–52
Faul M, Xu L, Wald MM, Coronado V, Dellinger AM (2010) Traumatic brain injury in the United States: national estimates of prevalence and incidence, 2002{\textendash}2006. Inj Prev [Internet]. 16(Suppl 1):A268--A268. Available from: https://injuryprevention.bmj.com/content/16/Suppl_1/A268.1
Feeney JM, Neulander M, DiFiori M, Kis L, Shapiro DS, Jayaraman V et al (2017) Direct oral anticoagulants compared with warfarin in patients with severe blunt trauma. Injury. 48(1):47–50
Franko J, Kish KJ, O’Connell BG, Subramanian S, Yuschak JV (2006) Advanced age and preinjury warfarin anticoagulation increase the risk of mortality after head trauma. J Trauma 61(1):107–10
Hecht JP, LaDuke ZJ, Cain-Nielsen AH, Hemmila MR, Wahl WL (2020) Effect of preinjury oral anticoagulants on outcomes following traumatic brain injury from falls in older adults. Pharmacotherapy 40(7):604–13
Hukkelhoven CWPM, Steyerberg EW, Rampen AJJ, Farace E, Habbema JDF, Marshall LF et al (2003) Patient age and outcome following severe traumatic brain injury: an analysis of 5600 patients. J Neurosurg 99(4):666–73
Hylek EM, Singer DE (1994) Risk factors for intracranial hemorrhage in outpatients taking warfarin. Ann Intern Med 120(11):897–902
Jones K, Sharp C, Mangram AJ, Dunn EL (2006) The effects of preinjury clopidogrel use on older trauma patients with head injuries. Am J Surg 192(6):743–5
Julien J, Alsideiri G, Marcoux J, Hasen M, Correa JA, Feyz M et al (2017) Antithrombotic agents intake prior to injury does not affect outcome after a traumatic brain injury in hospitalized elderly patients. J Clin Neurosci Off J Neurosurg Soc Australas 38:122–5
Karibe H, Hayashi T, Narisawa A, Kameyama M, Nakagawa A, Tominaga T (2017) Clinical characteristics and outcome in elderly patients with traumatic brain injury: for establishment of management strategy. Neurol Med Chir (Tokyo) 57(8):418–25
Karni A, Holtzman R, Bass T, Zorman G, Carter L, Rodriguez L et al (2001) Traumatic head injury in the anticoagulated elderly patient: a lethal combination. Am Surg 67(11):1098–100
Kennedy DM, Cipolle MD, Pasquale MD, Wasser T (2000) Impact of preinjury warfarin use in elderly trauma patients. J Trauma. 48(3):451–3
Kobayashi L, Barmparas G, Bosarge P, Brown CV, Bukur M, Carrick MM et al (2017) Novel oral anticoagulants and trauma: the results of a prospective American Association for the Surgery of Trauma Multi-Institutional Trial. J Trauma Acute Care Surg 82(5):827–35
Li J, Brown J, Levine M (2001) Mild head injury, anticoagulants, and risk of intracranial injury. Vol. 357, Lancet (London, England). England pp 771–2
Mahaffey KW, Hager R, Wojdyla D, White HD, Armstrong PW, Alexander JH et al (2015) Meta-analysis of intracranial hemorrhage in acute coronary syndromes: incidence, predictors, and clinical outcomes. J Am Heart Assoc 4(6):e001512
Mahmood H, Siddique I, McKechnie A (2020) Antiplatelet drugs: a review of pharmacology and the perioperative management of patients in oral and maxillofacial surgery. Ann R Coll Surg Engl 102(1):9–13
Mathieu F, Güting H, Gravesteijn B, Monteiro M, Glocker B, Kornaropoulos EN et al (2020) Impact of antithrombotic agents on radiological lesion progression in acute traumatic brain injury: a CENTER-TBI propensity-matched cohort analysis. J Neurotrauma 37(19):2069–80
Maung AA, Bhattacharya B, Schuster KM, Davis KA (2016) Trauma patients on new oral anticoagulation agents have lower mortality than those on warfarin. J Trauma Acute Care Surg 81(4):652–7
Parmar KA, Rao S, Abu-Zidan FM (2006) Head injuries in warfarinised patients. Singapore Med J [Internet]. 47(8):676—678. Available from: http://europepmc.org/abstract/MED/16865206
Pieracci FM, Eachempati SR, Shou J, Hydo LJ, Barie PS (2007) Degree of anticoagulation, but not warfarin use itself, predicts adverse outcomes after traumatic brain injury in elderly trauma patients. J Trauma 63(3):525–30
Posti JP, Ruuskanen JO, Sipilä JOT, Luoto TM, Rautava P, Kytö V (2022) Impact of oral anticoagulation and adenosine diphosphate inhibitor therapies on short-term outcome of traumatic brain injury. Neurology 99(11):e1122-30
Pozzessere A, Grotts J, Kaminski S (2015) Dabigatran use does not increase intracranial hemorrhage in traumatic geriatric falls when compared with warfarin. Am Surg 81(10):1039–42
Prexl O, Bruckbauer M, Voelckel W, Grottke O, Ponschab M, Maegele M et al (2018) The impact of direct oral anticoagulants in traumatic brain injury patients greater than 60-years-old. Scand J Trauma Resusc Emerg Med 26(1):20
Saab M, Gray A, Hodgkinson D, Irfan M (1996) Warfarin and the apparent minor head injury. J Accid Emerg Med 13(3):208–9
Sauter TC, Ziegenhorn S, Ahmad SS, Hautz WE, Ricklin ME, Leichtle AB et al (2016) Age is not associated with intracranial haemorrhage in patients with mild traumatic brain injury and oral anticoagulation. J Negat Results Biomed 15(1):12
Smith K, Weeks S (2012) The impact of pre-injury anticoagulation therapy in the older adult patient experiencing a traumatic brain injury: a systematic review. JBI Libr Syst Rev 10(58):4610–21
Steyerberg EW, Wiegers E, Sewalt C, Buki A, Citerio G, De Keyser V et al (2019) Case-mix, care pathways, and outcomes in patients with traumatic brain injury in CENTER-TBI: a European prospective, multicentre, longitudinal, cohort study. Lancet Neurol 18(10):923–34
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet (London, England) 2(7872):81–4
Toorop MMA, van Rein N, Nierman MC, Vermaas HW, Huisman MV, van der Meer FJM et al (2020) Switching from vitamin K antagonists to direct oral anticoagulants: Treatment satisfaction and patient concerns. J Thromb Haemost 18(6):1390–7
Turcato G, Zannoni M, Zaboli A, Zorzi E, Ricci G, Pfeifer N et al (2019) Direct oral anticoagulant treatment and mild traumatic brain injury: risk of early and delayed bleeding and the severity of injuries compared with vitamin K antagonists. J Emerg Med 57(6):817–24
Wojcik R, Cipolle MD, Seislove E, Wasser TE, Pasquale MD (2001) Preinjury warfarin does not impact outcome in trauma patients. J Trauma 51(6):1142–7
Wood B, Nascimento B, Rizoli S, Sholzberg M, McFarlan A, Phillips A et al (2017) The anticoagulated trauma patient in the age of the direct oral anticoagulants: a Canadian perspective. Scand J Trauma Resusc Emerg Med 25(1):76
Acknowledgements
The authors would like to thank Marius Brusselmans for his statistical advice.
Funding
This work was supported by the Fund for Scientific Research – Flanders (FWO) and Helaers Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This project was approved by the Research Ethics Committee UZ/KU Leuven. IRB waived the need for informed consent.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Laic, R.A.G., Verhamme, P., Vander Sloten, J. et al. Long-term outcomes after traumatic brain injury in elderly patients on antithrombotic therapy. Acta Neurochir 165, 1297–1307 (2023). https://doi.org/10.1007/s00701-023-05542-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05542-5