Abstract
Purpose
Degenerative cervical myelopathy is a progressive slow-motion spinal cord injury. Surgery is the mainstay of treatment. Baseline disability predicts surgical recovery; therefore, timely treatment is critical to restoring function. However, current challenges mean most patients present with advanced disease and are instead left with life changing disabilities. While short-term mortality is rarely reported, the long-term effects of this on life expectancy are unknown, including whether function could be modifiable with timely treatment. This article investigates the effect of DCM on life expectancy.
Methods
The survival of patients from an observational study of patients undergoing surgery from 1994 to 2007 was compared to their expected survival using a gender- and aged -matched cohort. Comparisons were made by one sample log-rank test and standardised mortality ratios. Factors associated with survival were explored using a Cox regression analysis, including disease severity.
Results
A total of 357 patients were included in the analysis. After a median follow-up of 15.3 years, 135 of 349 patients had died; 114.7 deaths would have been expected. The DCM cohort had an increased risk of death compared to the non-DCM cohort (standardised mortality ratio 1.18 [95% CI: 1.02–1.34]. Age at operation 1.08 (95% CI: 1.07 to 1.1, p < 0.001) and severe DCM 1.6 (95% CI: 1.06 to 2.3, p = 0.02) were associated with worse survival (N = 287). In those surviving at least 2 years after surgery, only severe DCM was associated with conditional survival (HR 1.6, 95% CI 1.04 2.4, p = 0.03).
Conclusion
Life expectancy is reduced in those undergoing surgery for DCM. This is driven by premature mortality among those left with severe disability. As disability can be reduced with timely treatment, these findings reinforce the need for collective and global action to raise awareness of DCM and enable early diagnosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
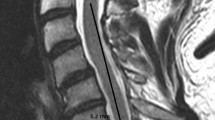
Degenerative cervical myelopathy (DCM) is a form of slow motion and evolving spinal cord injury [20]. It is estimated to affect 1 in 50 adults [66], although today most are never diagnosed. [35, 63] In DCM, spinal cord damage is driven by mechanical stress brought about by degenerative/spondylotic changes to the spine, such as disc prolapse, spondylolisthesis, ligament hypertrophy, or ossification [7]. This can cause a variety of different symptoms [24, 57] and experiences. [44] While changes in dexterity, gait, bladder function, limb pain, and sensation are the focus of current assessments [18, 23, 40], this under represents a disease, which can affect the whole body, from internal organs such as the cardiorespiratory system [11, 13, 47, 48, 74] to perhaps even cranial nerves [14, 15, 24, 54]. This very individual experience of DCM is governed by a likely complex and poorly understand interaction between mechanical stress, time, and an individual’s vulnerability to spinal cord injury [26].
Surgery to remove the mechanical stress on the spinal cord is the mainstay of treatment[31]. It has been shown to stop further spinal cord damage and enable recovery [30]. However, due to the limited capacity of the spinal cord to repair, a ‘full’ recovery is therefore dependent on offering surgery before there is irreversible damage. [68] Today, most patients reach surgeons with advanced disease after years of symptoms. [62] Based on healthcare activity in the UK, it has been recently estimated that ~ 90% of DCM may go undiagnosed, particularly among the elderly [35]. Therefore today, recovery is generally incomplete. Instead, most patients are left with life-long disabilities associated with high levels of dependence and unemployment [62]. A recent report by the DCM charity, Myelopathy.org, has estimated this equates to an average lifetime loss of earnings of ~ £0.5 m for those of working age, with a conservative cost to English society of £0.7bn per year [25].
In the short-term, at least, mortality is rarely reported [18], even among those undergoing surgery [75] but for a group left with multisystem disability, is this true life-long? While some surgical series on DCM have reported longer-term outcomes[3, 31, 59] [4, 33], these rarely stretch beyond 5 years. Moreover the wider implications of a life with DCM are unknown. Further, if we can offer surgery in early stages of the disease, might any such impact be modifiable? In this study, we examine for the first time the effect of DCM on life expectancy.
Methods
Study design and patient population
This was a case–control study. The observed survival of a series of adult patients (> 18 years) who underwent surgical treatment for DCM and were enrolled to a prospective observational study from 1995 to 2007 [4, 46], was compared to their expected survival using a matched cohort of the general population, generated and matched for gender and year of birth using data from the Office for National Statistics, UK [1]. Survival status was retrieved following ethical approval and patient consent on August 1, 2020 using the National Health Service (UK) Spine. We included patients in the DCM surgery group if: were adults enrolled during the study who had follow-up of a minimum of 6 months post-operatively. Patients were excluded if they had missing survival data or if they did not complete the study. This includes the survival status of the UK population accurate to within 6 months.
Outcomes assessed
The following variables were obtained: age, sex, physical functioning domain of the SF36v1 and the Myelopathy Disability Index [MDI], survival at time of search query, and length of follow-up. Disease severity was measured using the MDI and its criteria for mild, moderate, and severe disability. [17]
Statistical analysis
Statistical analysis was performed in R (v3.60 www.r- project.org) using the ‘survival’ and ‘relsurv’packages. [60, 61, 73] To explore survival, a comparable cohort in terms of age and gender was created using annual age- (in 1-year increments) and sex-specific risk of death from the human mortality database for England and Wales [36]. Comparisons between observed and expected survival were then made using Kaplan–Meier survival methods, with a one-sample log-rank test [12] and standardised mortality ratios (SMR) used to detect the difference between groups. Significance was assessed using a chi-squared test on one degree of freedom as per previously published methods. [67]
Variables associated with survival were explored individually and in combination using a Cox regression [38]. Regression co-variates were selected using backward stepwise elimination, based on improving the Akaike Information Criterion (AIC). Alongside age and gender, the co-variates of interest were pre-chosen from the available postoperative outcome measures to represent health status after surgical treatment. Specifically, these were the physical functioning domain of the SF36v1 and the Myelopathy Disability Index [MDI]. Aside from gender, these were therefore continuous or ordinal variables and were categorised for analysis. The MDI was categorised as mild, moderate, or severe based on predefined thresholds [17]. The SF36v1 Physical Functioning Component Score dichotomised as either having achieved the minimal clinically important difference [MCID] or not[6]. The SF36v1 was chosen for this purpose, principally as such a threshold for the Myelopathy Disability Index has not been ascertained [79] and MDI a measure of DCM severity. The best value of outcomes from 12 to 24 months was taken to coincide with the window of peak recovery from surgery and minimise missing data[59]. Analysis of co-variates and regression testing was restricted to complete cases. Statistical significance was set at 5%. This analysis was then repeated using only those who had survived at least 2 years after surgery, referred to as the conditional cohort or conditional survival [61, 67]. This was performed to strengthen the identification of factors that influenced long-term survival.
Results
Study population
Cohort demographics are given in Table 1. A total of 357 patients were included in the DCM cohort. The mean age of the cohort at surgery was 55.8 ± 14.9, and 196 (56%) were male. The disease and treatment characteristics have been reported elsewhere [24, 31, 42], but in short, the original observational study was compiled by the senior author (RJCL), and we included patients with a clinical and imaging diagnosis of DCM who underwent surgical treatment. Patients completed patient-reported outcome measures preoperatively and at 3, 12, 24, and 60 months postoperatively. Outcome measures included the SF-36 (version 1) quality of life measure, the visual analogue scores for arm, neck, and hand pain, and condition-specific outcome measures the Myelopathy Disability Index [MDI] and the Neck Disability Score [NDI]. Most patients were treated via an anterior approach (ACDF- 247, 70.2%), with all others treated with a posterior approach. The median follow-up was 15.3 years after surgery (IQR 7.5, range 0.3–24.9).
Life expectancy estimate
One hundred thirty-five of 349 (38.7%) of patients died within the follow-up period. Average survival was 15.3 years (± interquartile range 7.5) and ranged from 0.3 to 24.9 years. From a corresponding age- and sex-matched sample, 114.7 deaths would have been expected. The standardised mortality ratio was 1.18 (95% confidence interval 1.02–1.34), indicating a significant increased risk of death in the DCM cohort. Figure 1 displays the observed (± 95% confidence intervals) and expected survival curves.
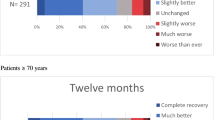
Age at operation and disease severity (chi squared 19.5, p < 0.001) were associated with observed survival. MCID (chi squared 0, p = 0.9) and gender (chi squared 1.9 p = 0.2) were not associated with increased survival. MCID and MDI were available for 262 and 287 patients. However, age and gender did not appear to differ between those with and without missing data (Supporting Information 1). Age was modelled across a range of thresholds, shown here in quartiles (chi squared 137, p < 0.001) (Fig. 2 and Supporting Information 2) [56].
Observed survival based on MDI severity strata. This effect was most marked when dichotimised as severe or not (Supporting Information 2)
Variables met the proportional hazard assumption and were entered into a Cox regression model. Backward stepwise elimination was used for variable reduction. Age at operation 1.08 (95% CI: 1.0 to 1.1, p < 0.001) and severe DCM 1.6 (95% CI: 1.1 to 2.3, p = 0.02) best explained variation in survival (N = 287).
For the conditional analysis performed on those surviving 2 years postoperatively, eight patients died within 2 years of surgery. Severe MDI (Fig. 3) and female gender (Fig. 4) had significantly reduced conditional survival. In a Cox regression, only severe DCM was associated with reduced conditional survival (HR 1.6, 95% CI 1.0–2.4, p = 0.03).
Discussion
This is the first study to explore the impact of DCM on life expectancy. It identified, despite surgical treatment, that people with DCM have a reduced life expectancy. Further within multivariate models, across both observed and conditional survival analyses, this was most likely among patients with severe DCM. Age at time of surgery did not predict conditional survival.
There are some important limitations to this analysis. The analysis was restricted to complete datasets, with potentially important covariates for analysis unmeasured in the original study [5, 16], and therefore unable to be included. Furthermore, expected survival was estimated using national survival data, matching on age and gender alone. This could be markedly different to our regional cohort recognised to have above average survival [77] and/or a cohort with disease and co-morbidities such as ischemic heart disease, hypertension, cancer, and others [2, 16]. The exact differences in co-morbidities between the two groups are unknown, which significantly limits the study findings. Further, the exact cause of death was not available for analysis; therefore, deaths related to DCM specifically cannot be delineated. Finally, the findings of this manuscript are generalised to those patients who underwent surgery. Therefore, it is unclear if patients with DCM managed without surgery have a worse survival than the general population.
All patients were identified between 1995 and 2007. While this is important in ensuring adequate follow-up data, this precludes us from measuring the effect of modern treatments on life expectancy, which may further extend DCM survival beyond what is reported in this study. The impact of these treatments will be known in the future.
That said, there is much to confer confidence in this overall finding. Firstly, this represents long-term follow-up from a single surgeon, prospective observational study; the case mix is therefore broadly anticipated to reflect routine practice. Secondly a ‘dose response’ relationship, i.e. that the effect was more pronounced within those with severe as opposed to milder disease, increases the likelihood of a true relationship [37]. Further, this effect was seen both with conditional and observed survival. Finally, and importantly, it aligns with the limited reports from other spinal cord diseases [51, 52]. For example, using a similar approach, Middleton et al. (2012) demonstrated life expectancy was reduced for traumatic spinal cord injury and associated with severity of injury [52].
So, what are the implications for DCM practice and research? Firstly, this finding reinforces the need to consider the long-term consequences of DCM. This is an aspect which has received little research consideration. For example, with respect to surgery, which has been the focus of DCM research to date, most have excluded recurrent disease and considered relatively short-term outcomes [19, 34, 55]. This may be important. For example, many have adopted surgical procedures such as instrumented fusion over decompression alone due to their hypothesised long-term benefits, but these remain unproven [8, 29, 32, 78].
However, more importantly, perhaps, is the indication that this impact would be modifiable. Reduced life expectancy here was driven by those with severe DCM but not observed in those with milder disease. Modelling from surgical outcome data over the last 15 years has demonstrated that disease severity at surgery and length of time with symptoms are critical determinants of outcome [69,70,71]. As a progressive disease, these factors are likely related [7, 49]. In an updated prediction model, time to treatment within 4 months of symptom onset was predictive of minimal post-operative disability [71]. Put simply, timely treatment could reduce disability in DCM and restore normal life expectancy.
Delivering this however remains a more difficult prospect. Patients today wait, on average, 2 to 5 years for diagnosis, often misdiagnosed and treated for alternative diagnoses first. [10, 28, 41, 62] DCM also often goes undiagnosed [43, 63]; a recent analysis from the UK suggests this could be as much as 90%. [35] Early DCM is also difficult to detect, as DCM can cause a wide variety of symptoms, which may fluctuate, and their frequency or nature in early stages is poorly understood [21, 24, 53, 57]. Further, DCM remains a clinical diagnosis, with MRI only able to support a diagnosis[80], for example, given cord compression is ten times more likely to be incidental [66]. Frontline professionals have received relatively little training on DCM, but even following referral for further investigation, unstructured healthcare pathways and access to MRI mean treatment can still take years [28, 39, 41, 42, 76]. While this remains the greater challenge [27, 43], how and when to offer surgery in mild disease remains a critical knowledge gap. [58, 65] Observational studies have demonstrated that many patients can remain stable for years [3, 9, 64]; consequently, the risks of surgery would seem unwarranted. However, others progress, sometimes quickly. The current guidelines therefore recommend close observation for those managed non-operatively, although exactly what this entails has not been defined. [31] Global research activity is starting to target this knowledge gap, aiming to help stratification through improved diagnostics such as advanced imaging or biomarkers [50], as well as detect disease progression through improved monitoring tools. [72]
The importance of enabling both timely treatment and understanding the long-term implications of DCM and its natural history have been identified as critical research priorities by AO Spine RECODE DCM, a global initiative working to accelerate knowledge discovery in DCM[27]. This process has also formed a minimum dataset, which identified ‘death’ as a core outcome to be measured going forward [22].
The findings of this study therefore reinforce the importance of tackling unexplored aspects of DCM, but in particular, that timely treatment may not just mitigate disability but also save life.
Conclusions
Life expectancy for people with DCM is reduced despite surgical treatment. This is driven by premature mortality among those left with severe disability. Disability in DCM can be reduced with timely diagnosis and treatment, but many multi-disciplinary and system challenges need to be overcome. These findings therefore reinforce the need for collective and global action [45].
Data Availability
The original data is available on request.
References
Deaths registered by single year of age, UK - Office for National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/datasets/deathregistrationssummarytablesenglandandwalesdeathsbysingleyearofagetables. Accessed 14 Apr 2021
Trends in life expectancy and healthy life expectancy. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/464275/gs-15-13-future-ageing-trends-life-expectancy-er12.pdf. Accessed 14 Apr 2021
Adamova B, Kerkovsky M, Kadanka Z, Dusek L, Jurova B, Vlckova E, Bednarik J (2017) Predictors of symptomatic myelopathy in degenerative cervical spinal cord compression. Brain Behav 7(9):e00797
Al-Tamimi YZ, Guilfoyle M, Seeley H, Laing RJ (2013) Measurement of long-term outcome in patients with cervical spondylotic myelopathy treated surgically. Eur SpineJ : Off Publ Eur Spine Soc, Eur Spinal Deformity Soc Eur Sect Cervical Spine Res Soc 22(11):2552–2557
Badhiwala JH, Witiw CD, Nassiri F, Jaja BNR, Akbar MA, Mansouri A, Merali Z, Ibrahim GM, Wilson JR, Fehlings MG (2018) Patient phenotypes associated with outcome following surgery for mild degenerative cervical myelopathy: a principal component regression analysis. Spine J 18(12):2220–2231
Badhiwala JH, Witiw CD, Nassiri F, Akbar MA, Jaja B, Wilson JR, Fehlings MG (2018) Minimum clinically important difference in SF-36 scores for use in degenerative cervical myelopathy. Spine 43(21):E1260–E1266
Badhiwala JH, Ahuja CS, Akbar MA, Witiw CD, Nassiri F, Furlan JC, Curt A, Wilson JR, Fehlings MG (2020) Degenerative cervical myelopathy - update and future directions. Nat Rev Neurol 16(2):108–124
Bajamal AH, Kim S-H, Arifianto MR et al (2019) Posterior surgical techniques for cervical spondylotic myelopathy: WFNS Spine Committee recommendations. Neurospine 16(3):421–434
Bednarik J, Kadanka Z, Dusek L, Kerkovsky M, Vohanka S, Novotny O, Urbanek I, Kratochvilova D (2008) Presymptomatics pondylotic cervical myelopathy: an updated predictive model. Eur Spine J : Off Publ Eur Spine Soc, Eur Spinal Deformity Soc Eur Sect Cervical Spine Res Soc 17(3):421–431
Behrbalk E, Salame K, Regev GJ, Keynan O, Boszczyk B, Lidar Z (2013) Delayed diagnosis of cervical spondylotic myelopathy by primary care physicians. Neurosurg Focus 35(1):E1
Bhagavatula ID, Bhat DI, Sasidharan GM, Mishra RK, Maste PS, Vilanilam GC, Sathyaprabha TN (2016) Subclinical respiratory dysfunction in chronic cervical cord compression: a pulmonary function test correlation. Neurosurg Focus 40(6):E3. https://doi.org/10.3171/2016.3.FOCUS1647
Bland JM, Altman DG (2004) The logrank test Bmj 328(7447):1073
Boerger T, Alsouhibani A, Mowforth O, Hamilton J, Lalkhen A, Davies BM, Kotter MRN (2021) Moving beyond the neck and arm: the pain experience of people with degenerative cervical myelopathy who have pain. Global Spine J 12(7):1434–1442. https://doi.org/10.1177/2192568220986143
Chen Z, Zhao R, Wang Q, et al (2019) Functional connectivity changes of the visual cortex in the cervical spondylotic myelopathy patients: a resting-state fMRI study. Spine Publish Ahead of Print:1
Chen Z, Wang Q, Liang M, Zhao R, Zhu J, Xiong W, Su Z, Yu C, Xue Y (2018) Visual cortex neural activity alteration in cervical spondylotic myelopathy patients: a resting-state fMRI study. Neuroradiol 60(9):921–932
Clark TG, Bradburn MJ, Love SB, Altman DG (2003) Survival analysis part i: basic concepts and first analyses. Brit J Cancer 89(2):232–238
Davies BM, Nourallah B, Venkatesh A, Ali AMS, Guilfoyle M, Francis J, Kotter MRN, Laing RJC (2020) Establishing mild, moderate and severe criteria for the myelopathy disability index in cervical spondylotic myelopathy. Brit J Neurosurg 1–5
Davies BM, McHugh M, Elgheriani A, Kolias AG, Tetreault LA, Hutchinson PJA, Fehlings MG, Kotter MRN (2016) Reported outcome measures in degenerative cervical myelopathy: a systematic review. Plos One 11(8):e0157263
Davies BM, McHugh M, Elgheriani A, Kolias AG, Tetreault L, Hutchinson PJA, Fehlings MG, Kotter MRN (2017) The reporting of study and population characteristics in degenerative cervical myelopathy: a systematic review. PLoS ONE 12(3):e0172564
Davies BM, Mowforth OD, Smith EK, Kotter MR (2018) Degenerative cervical myelopathy. BMJ 360:k186
Davies BM, Munro CF, Kotter M (2018) A novel insight into the challenges of diagnosing degenerative cervical myelopathy using online symptom checkers. J Med Internet Res 21(1):e10868
Davies BM, Khan DZ, Mowforth OD et al (2019) RE-CODE DCM ( REsearch Objectives and Common Data Elements for Degenerative Cervical Myelopathy): A consensus process to improve research efficiency in DCM, through establishment of a standardized dataset for clinical research and the definition of the research priorities. Global Spine J 9(1_suppl):65S-76S
Davies B, Mowforth O, Sadler I et al (2019) Recovery priorities in degenerative cervical myelopathy: a cross-sectional survey of an international, online community of patients. BMJ Open 9(10):e031486
Davies BM, Munro C, Khan DZ, Fitzpatrick SM, Hilton B, Mowforth OD, McNair AGK, Sadler I, Kotter MRN (2020) Outcomes of degenerative cervical myelopathy from the perspective of persons living with the condition: findings of a semistructured interview process with partnered internet survey. Global Spine j 6(22):2192568220953811
Davies BM, Phillips R, Clarke D et al (2022) Establishing the socio-economic impact of degenerative cervical myelopathy is fundamental to improving outcomes [AO Spine RECODE-DCM Research Priority Number 8]. Global Spine J 12(1_suppl):122S-129S. https://doi.org/10.1177/21925682211039835
Davies BM, Mowforth O, Gharooni A-A et al (2022) A new framework for investigating the biological basis of degenerative cervical myelopathy [AO Spine RECODE-DCM Research Priority Number 5]: mechanical stress, vulnerability and time. Global Spine J 12(1_suppl):78S-96S
Davies BM, Kwon BK, Fehlings MG, Kotter MRN (2022) AO Spine RECODE-DCM: why prioritize research in degenerative cervical myelopathy? Global Spine J 12(1_suppl):5S-7S
Davies BM, Mowforth O, Wood H et al (2022) Improving awareness could transform outcomes in degenerative cervical myelopathy [AO Spine RECODE-DCM Research Priority Number 1]. Global Spine J 12(1_suppl):28S-38S
Deora H, Kim S-H, Behari S, Rudrappa S, Rajshekhar V, Zileli M, Parthiban JKBC, Committee WF of NS (WFNS) S (2019) Anterior surgical techniques for cervical spondylotic myelopathy: WFNS Spine Committee recommendations. Neurospine 16(3):408–420
Fehlings MG, Ibrahim A, Tetreault L et al (2015) A global perspective on the outcomes of surgical decompression in patients with cervical spondylotic myelopathy: results from the prospective multicenter AO Spine international study on 479 patients. Spine 40(17):1322–1328
Fehlings MG, Tetreault LA, Riew KD et al (2017) A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Global Spine J 7(3 Suppl):70S-83S
Ghogawala Z, Terrin N, Dunbar MR et al (2021) Effect of ventral vs dorsal spinal surgery on patient-reported physical functioning in patients with cervical spondylotic myelopathy: a randomized clinical trial. JAMA 325(10):942–951.https://doi.org/10.1001/jama.2021.1233
Gornet MF, McConnell JR, Riew KD, Lanman TH, Burkus JK, Hodges SD, Dryer RF, Copay AG, Schranck FW (2018) Treatment of cervical myelopathy: long-term outcomes of arthroplasty for myelopathy versus radiculopathy, and arthroplasty versus arthrodesis for myelopathy. Clin Spine Surg 31(10):420–427. https://doi.org/10.1097/BSD.0000000000000744
Grodzinski B, Bestwick H, Bhatti F, Durham R, Khan M, Sarathi CIP, Teh JQ, Mowforth O, Davies B (2021) Research activity amongst DCM research priorities. Acta Neurochir 1–8
Grodzinski B, Stubbs DJ, Davies BM (2022) Most degenerative cervical myelopathy remains undiagnosed, particularly amongst the elderly: modelling the prevalence of degenerative cervical myelopathy in the United Kingdom. J Neurol 1–9
Guilfoyle MR, Hutchinson PJA, Santarius T (2017) Improved long-term survival with subdural drains following evacuation of chronic subdural haematoma. Acta Neurochir 159(5):903–905
Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A (2011) GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 64(4):380–382
Hidalgo B, Goodman M (2013) Multivariate or multivariable regression? Am J Public Health 103(1):39–40
Hilton B, Tempest-Mitchell J, Davies BM, Kotter MRN Assessment of degenerative cervical myelopathy differs between specialists and may influence time to diagnosis and clinical outcomes. PloS one
Hilton B, Tempest-Mitchell J, Davies B, Kotter M (2018) Assessment of degenerative cervical myelopathy differs between specialists and may influence time to diagnosis and clinical outcomes. PLoS ONE 13(12):e0207709
Hilton B, Tempest-Mitchell J, Davies B, Kotter M (2019) Route to diagnosis of degenerative cervical myelopathy in a UK healthcare system: a retrospective cohort study. BMJ Open 9(5):e027000. https://doi.org/10.1136/bmjopen-2018-027000
Hilton B, Tempest-Mitchell J, Davies BM et al (2019) Cord compression defined by MRI is the driving factor behind the decision to operate in degenerative cervical myelopathy despite poor correlation with disease severity. PLoS ONE 14(12):e0226020
Hilton B, Gardner EL, Jiang Z et al (2022) Establishing diagnostic criteria for degenerative cervical myelopathy [AO Spine RECODE-DCM Research Priority Number 3]. Global Spine J 12(1_suppl):55S-63S
Khan DZ, Fitzpatrick SM, Hilton B, McNair AG, Sarewitz E, Davies BM, Kotter MR, Injury ASKFSC (2020) Prevailing outcome themes reported by people with degenerative cervical myelopathy: findings from a focus group session (Preprint). Jmir Form Res 5(2):e18732
Khan DZ, Hazenbiller O, Gronlund T, Sadler I, Sarewitz EB, Mowforth O, Kotter MRN, Davies BM (2022) The AO Spine RECODE-DCM international collaborative—establishing the foundations for accelerated and patient-centered innovation. Global Spine J 12(1_suppl):159S-171S
Latimer M, Haden N, Seeley HM, Laing RJ (2002) Measurement of outcome in patients with cervical spondylotic myelopathy treated surgically. Brit J Neurosurg 16(6):545–549
Li Z, Zhao Y, Jia W, Wang X, Chen B, Shahbaz M, Nie L, Cheng L (2015) Surgical treatment of cervical spondylotic myelopathy associated hypertension–a retrospective study of 309 patients. Plos One 10(7):e0133828
Lin S-Y, Chen D-C, Lin C-L, Lee H-C, Lin T-C, Wang I-K, Hsu C-Y, Kao C-H (2018) Risk of acute coronary syndrome in patients with cervical spondylosis. Atherosclerosis 271:136–141
Martin AR, Kalsi-Ryan S, Akbar MA, Rienmueller AC, Badhiwala JH, Wilson JR, Tetreault LA, Nouri A, Massicotte EM, Fehlings MG (2021) Clinical outcomes of nonoperatively managed degenerative cervical myelopathy: an ambispective longitudinal cohort study in 117 patients. J Neurosurg Spine 34(6):821–829
Martin AR, Tetreault L, Nouri A et al (2022) Imaging and electrophysiology for degenerative cervical myelopathy [AO Spine RECODE-DCM Research Priority Number 9]. Global Spine J 12(1_suppl):130S-146S
Mealy MA, Kessler RA, Rimler Z, Reid A, Totonis L, Cutter G, Kister I, Levy M (2018) Mortality in neuromyelitis optica is strongly associated with African ancestry. Neurology - Neuroimmunol Neuroinflammation 5(4):e468
Middleton JW, Dayton A, Walsh J, Rutkowski SB, Leong G, Duong S (2012) Life expectancy after spinal cord injury: a 50-year study. Spinal Cord 50(11):803–811
Mizer A, Bachmann A, Gibson J, Donaldson MB (2017) Self-report and subjective history in the diagnosis of painful neck conditions: a systematic review of diagnostic accuracy studies. Musculoskelet Sci Pract 31:30–44
Mowforth OD, Davies BM, Kotter MR (2019) “I am not delusional!” Sensory dysaesthesia secondary to degenerative cervical myelopathy. BMJ case reports 12(4):e229033
Mowforth OD, Davies BM, Goh S, O’Neill CP, Kotter MRN (2019) Research inefficiency in degenerative cervical myelopathy: findings of a systematic review on research activity over the past 20 years. Global Spine J 10(4):476–485. https://doi.org/10.1177/2192568219847439
Nelson SLP, Ramakrishnan V, Nietert PJ, Kamen DL, Ramos PS, Wolf BJ (2017) An evaluation of common methods for dichotomization of continuous variables to discriminate disease status. Commun Statistics - Theory Methods 46(21):10823–10834
Niu S, Anastasio AT, Maidman SD, Faraj RR, Rhee JM (2020) The frequency of various “myelopathic symptoms” in cervical myelopathy. Clin Spine Surg 33(10):E448–E453
Nouri A, Tessitore E, Molliqaj G et al (2022) Degenerative cervical myelopathy: development and natural history [AO Spine RECODE-DCM Research Priority Number 2]. Global Spine J 12(1_suppl):39S-54S
Pandita N, Gupta S, Raina P, Srivastava A, Hakak AY, Singh O, DarokhanMohdA BM (2019) Neurological recovery pattern in cervical spondylotic myelopathy after anterior surgery: a prospective study with literature review. Asian Spine J 13(3):423–431
Perme MP, Pavlic K (2018) Nonparametric relative survival analysis with the R package relsurv. J Stat Softwhttps://doi.org/10.18637/jss.v087.i08
Pohar M, Stare J (2006) Relative survival analysis in R. Comput Meth Prog Bio 81(3):272–278
Pope DH, Mowforth OD, Davies BM, Kotter MRN (2020) Diagnostic delays lead to greater disability in degenerative cervical myelopathy and represent a health inequality. Spine 45(6):368–377
Radcliff KE, Curry EP, Trimba R, Walker JB, Purtill JJ, Austin MS, Parviz J, Vaccaro AR, Hilibrand AS, Albert TJ (2015) High incidence of undiagnosed cervical myelopathy in patients with hip fracture compared to controls. Journal of orthopaedic traumahttps://doi.org/10.1097/bot.0000000000000485
Rhee JM, Shamji MF, Erwin WM et al (2013) Nonoperative management of cervical myelopathy: a systematic review. Spine 38(22 Suppl 1):S55-67
Rodrigues-Pinto R, Montenegro TS, Davies BM et al (2022) Optimizing the application of surgery for degenerative cervical myelopathy [AO Spine RECODE-DCM Research Priority Number 10]. Global Spine J 12(1_suppl):147S-158S
Smith SS, Stewart ME, Davies BM, Kotter MRN (2020) The prevalence of asymptomatic and symptomatic spinal cord compression on magnetic resonance imaging: a systematic review and meta-analysis. Global Spine J 6(8):219256822093449
Stare J, Henderson R, Pohar M (2005) An individual measure of relative survival. J Royal Statistical Soc Ser C Appl Statistics 54(1):115–126
Tetreault LA, Kopjar B, Vaccaro A, Yoon ST, Arnold PM, Massicotte EM, Fehlings MG (2013) A clinical prediction model to determine outcomes in patients with cervical spondylotic myelopathy undergoing surgical treatment: data from the prospective, multi-center AO Spine North America study. J Bone Jt Surg Am 95(18):1659–1666
Tetreault L, Kopjar B, Côté P, Arnold P, Fehlings MG (2015) A clinical prediction rule for functional outcomes in patients undergoing surgery for degenerative cervical myelopathy: analysis of an international prospective multicenter data set of 757 subjects. J Bone Jt Surg Am 97(24):2038–2046
Tetreault L, Ibrahim A, Côté P, Singh A, Fehlings MG (2016) A systematic review of clinical and surgical predictors of complications following surgery for degenerative cervical myelopathy. J Neurosurg Spine 24(1):77–99
Tetreault L, Wilson JR, Kotter MRN, Côté P, Nouri A, Kopjar B, Arnold PM, Fehlings MG (2018) Is preoperative duration of symptoms a significant predictor of functional outcomes in patients undergoing surgery for the treatment of degenerative cervical myelopathy? Neurosurg 38(22 suppl 1):S1-647
Tetreault L, Garwood P, Gharooni A-A et al (2022) Improving assessment of disease severity and strategies for monitoring progression in degenerative cervical myelopathy [AO Spine RECODE-DCM Research Priority Number 4]. Global Spine J 12(1_suppl):64S-77S
Therneau T (2021). A package for survival analysis in R. https://CRAN.R-project.org/package=survival. Accessed 24 Sep 2021
Toyoda H, Nakamura H, Konishi S, Terai H, Takaoka K (2004) Does chronic cervical myelopathy affect respiratory function? J Neurosurg Spine 1(2):175–178
Wang T, Tian X-M, Liu S-K, Wang H, Zhang Y-Z, Ding W-Y (2017) Prevalence of complications after surgery in treatment for cervical compressive myelopathy: a meta-analysis for last decade. Med 96(12):e6421
Waqar M, Wilcock J, Garner J, Davies B, Kotter M (2020) Quantitative analysis of medical students’ and physicians’ knowledge of degenerative cervical myelopathy. BMJ Open 10(1):e028455
Woods LM, Rachet B, Riga M, Stone N, Shah A, Coleman MP (2005) Geographical variation in life expectancy at birth in England and Wales is largely explained by deprivation. J EpidemiolCommun H 59(2):115
Yang X, Gharooni A-A, Dhillon RS et al (2021) The relative merits of posterior surgical treatments for multi-level degenerative cervical myelopathy remain uncertain: findings from a systematic review. J Clin Med 10(16):3653
Zhou F, Zhang Y, Sun Y, Zhang F, Pan S, Liu Z (2015) Assessment of the minimum clinically important difference in neurological function and quality of life after surgery in cervical spondylotic myelopathy patients: a prospective cohort study. Eur Spine J 24(12):2918–2923
Zipser CM, Fehlings MG, Margetis K, Curt A, Betz M, Sadler I, Tetreault L, Davies BM, Group ASRDSC and M of the DCW (2022) Proposing a framework to understand the role of imaging in degenerative cervical myelopathy: enhancement of MRI protocols needed for accurate diagnosis and evaluation. Spine 47(17):1259–1262
Acknowledgements
This research aligns with the AO Spine RECODE DCM, James Lind Alliance top research priority individualizing surgery and awareness selected by people living and working with DCM. For further information on how this process was conducted, why these questions were prioritised, and global updates on currently aligned research, please visit aospine.org/recode/individualizing-surgery or aospine.org/recode/awareness.
Funding
BMD is supported by a NIHR Clinical Doctoral Research Fellowship. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health and Social Care.
DJS is supported by a Wellcome Trust Clinician PhD Fellowship (overarching grant number: 204017/Z/16/Z). This work has arisen from a Wellcome Trust-funded Clinician PhD Fellowship (to DJS) and, as the work was funded, in whole or in part, by the Wellcome Trust (grant number: 204017/Z/16/Z. A CC BY or equivalent license will be applied to any author accepted manuscript (AAM) arising from this submission, in accordance with the grant’s open access conditions.
Author information
Authors and Affiliations
Contributions
BMD: conception, writing, data collection, reviewing, and editing. DJS: conception, writing, data collection, reviewing, and editing. CSG: reviewing and editing. BG: conception, writing, data collection, reviewing, editing, and supervision. AV: reviewing and editing. MG, MRNK, and RL: critical reviewing, editing, supervision, advice; and guarantors. Both BMD and DJS contributed equally and have the right to list their name first in their CV.
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Benjamin M. Davies and Daniel Stubbs are joint first authors.
This article is part of the Topical Collection on Spine degenerative.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Davies, B.M., Stubbs, D., Gillespie, C.S. et al. Life expectancy in patients with degenerative cervical myelopathy is currently reduced but can be restored with timely treatment. Acta Neurochir 165, 1133–1140 (2023). https://doi.org/10.1007/s00701-023-05515-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-023-05515-8