Abstract
Purpose
To determine the association between optic nerve sheath diameter (ONSD) and outcome in patients with traumatic brain injury (TBI) who undergo hematoma removal (HR).
Methods
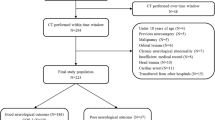
This study was a retrospective analysis of data from a single center between 2016 and 2021. Adult patients with TBI who underwent HR within 24 h after admission were included in this study. Preoperative and postoperative ONSD of the surgical side and the mean ONSD of both sides were measured for analysis. The primary outcome was mortality at 30 days. Receiver operating characteristic curve analysis was performed to calculate the area under the curve (AUC) and 95% confidence interval (CI) for 30 days mortality.
Results
Sixty-one patients were enrolled in the study. Among them, 48 (78.7%) survived for 30 days after admission. The AUC and 95% CI of the postoperative mean ONSD on both sides and postoperative/preoperative mean of the ONSD ratio on both sides were 0.884 [0.734–0.955] and 0.875 [0.751–0.942], respectively. The postoperative mean of both ONSDs of 6.0 mm had high accuracy as a cut-off value with a sensitivity of 85%, specificity of 83%, positive likelihood ratio (LR) of 5.0, and negative LR- of 0.18.
Conclusion
This study demonstrated that postoperative ONSD and the postoperative/preoperative ONSD ratio were associated with postoperative outcome in patients with TBI who underwent HR.



Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the Saiseikai Research group, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
References
Amini A, Kariman H, Arhami Dolatabadi A, Hatamabadi HR, Derakhshanfar H, Mansouri B, Safari S, Eqtesadi R (2013) Use of the sonographic diameter of optic nerve sheath to estimate intracranial pressure. Am J Emerg Med 31(1):236–239
Bekerman I, Sigal T, Kimiagar I, Ben EA, Vaiman M (2016) American Journal of Emergency Medicine The quantitative evaluation of intracranial pressure by optic nerve sheath diameter / eye diameter CT measurement ☆, ☆☆. Am J Emerg Med 34(12):2336–2342
Bland JM, Altman DG (1997) Cronbach’s alpha. BMJ 314(7080):572
Carney N, Totten AM, O’Reilly C et al (2017) Guidelines for the management of severe traumatic brain injury. Fourth Edition Neurosurgery 80(1):6–15
Choi YH, Lim TK, Lee SG (2017) Clinical features and outcomes of bilateral decompression surgery for immediate contralateral hematoma after craniectomy following acute subdural hematoma. Korean J Neurotrauma 13(2):108–112
Du J, Deng Y, Li H, Qiao S, Yu M, Xu Q, Wang C (2020) Ratio of optic nerve sheath diameter to eyeball transverse diameter by ultrasound can predict intracranial hypertension in traumatic brain injury patients: a prospective study. Neurocrit Care 32(2):478–485
Fletcher-Sandersjöö A, Thelin EP, Maegele M, Svensson M, Bellander BM (2021) Time course of hemostatic disruptions after traumatic brain injury: a systematic review of the literature. Neurocrit Care 34(2):635–656
Fujiwara G, Murakami M, Ishii W, Maruyama D, Iizuka R, Murakami N, Hashimoto N (2022) Effectiveness of administration of fibrinogen concentrate as prevention of hypofibrinogenemia in patients with traumatic brain injury with a higher risk for severe hyperfibrinolysis: single center before-and-after study. Neurocrit Care. https://doi.org/10.1007/s12028-022-01626-9
Fujiwara G, Okada Y, Sakakibara T, Yamaki T, Hashimoto N (2021) The association between D - dimer levels and long - term neurological outcomes of patients with traumatic brain injury : an analysis of a nationwide observational neurotrauma database in Japan. Neurocrit Care. https://doi.org/10.1007/s12028-021-01329-7
Grimes DA, Schulz KF (2005) Refining clinical diagnosis with likelihood ratios. Lancet 365(9469):1500–1505
Hanafi MG, Verki MM, Parei SN (2019) Ultrasonic assessment of optic nerve sheath to detect increased intracranial pressure. J Med Ultrasound 27(2):69–74
Hansen HC, Helmke K (1996) The subarachnoid space surrounding the optic nerves An ultrasound study of the optic nerve sheath. Surg Radiol Anat 18(4):323–328
Hayakawa M, Maekawa K, Kushimoto S et al (2016) High D-dimer levels predict a poor outcome in patients with severe trauma, even with high fibrinogen levels on arrival. Shock 45(3):308–314
Hayakawa M, Maekawa K, Kushimoto S et al (2016) High D-dimer levels predict a poor outcome in patients with severe trauma, even with high fibrinogen levels on arrival: a multicenter retrospective study. Shock 45(3):308–314
Jenjitranant P, Tunlayadechanont P, Prachanukool T, Kaewlai R (2020) Correlation between optic nerve sheath diameter measured on imaging with acute pathologies found on computed tomography of trauma patients. Eur J Radiol 125:108875
Jeon SB, Kwon SU, Park JC et al (2016) Reduction of midline shift following decompressive hemicraniectomy for malignant middle cerebral artery infarction. J Stroke 18(3):328–336
Juratli TA, Zang B, Litz RJ, Sitoci K-H, Aschenbrenner U, Gottschlich B, Daubner D, Schackert G, Sobottka SB (2014) Early hemorrhagic progression of traumatic brain contusions: frequency, correlation with coagulation disorders, and patient outcome: a prospective study. J Neurotrauma 31(17):1521–1527
Kaur A, Gautam PL, Sharma S, Singh VP, Sharma S (2021) Bedside ultrasonographic assessment of optic nerve sheath diameter as a means of detecting raised intracranial pressure in neuro-trauma patients: a cross-sectional study. Ann Indian Acad Neurol 24(1):63–68
Kavi T, Gupta A, Hunter K, Schreiber C, Shaikh H, Turtz AR (2018) Optic nerve sheath diameter assessment in patients with intracranial pressure monitoring. Cureus. https://doi.org/10.7759/cureus.3546
Kurland D, Hong C, Aarabi B, Gerzanich V, Simard JM (2012) Hemorrhagic progression of a contusion after traumatic brain injury: A review. J Neurotrauma 29(1):19–31
Lee SJ, Choi MH, Lee SE, Park JH, Park B, Lee JS, Hong JM (2020) Optic nerve sheath diameter change in prediction of malignant cerebral edema in ischemic stroke: an observational study. BMC Neurol 20(1):1–10
Liugan M, Xu Z, Zhang M (2017) Reduced free communication of the subarachnoid space within the optic canal in the human. Am J Ophthalmol 179:25–31
Lochner P, Czosnyka M, Naldi A, Lyros E, Pelosi P, Mathur S, Fassbender K, Robba C (2019) Optic nerve sheath diameter: present and future perspectives for neurologists and critical care physicians. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol 40(12):2447–2457
Mallett S, Halligan S, Matthew Thompson GP, Collins GS, Altman DG (2012) Interpreting diagnostic accuracy studies for patient care. BMJ 345(7871):1–7
Mathews A, Cattamanchi S, Panneerselvam T, Trichur RV (2020) Evaluation of bedside sonographic measurement of optic nerve sheath diameter for assessment of raised intracranial pressure in adult head trauma patients. J Emerg Trauma Shock 13(3):190–195
Matsuno A, Katayama H, Wada H, Morikawa K, Tanaka K, Tanaka H, Murakami M, Fuke N, Nagashima T (2003) Significance of consecutive bilateral surgeries for patients with acute subdural hematoma who develop contralateral acute epi- or subdural hematoma. Surg Neurol 60(1):23–30 (discussion 30)
Nakae R, Takayama Y, Kuwamoto K, Naoe Y, Sato H, Yokota H (2016) Time course of coagulation and fibrinolytic parameters in patients with traumatic brain injury. J Neurotrauma 33(7):688–695
Ohle R, McIsaac SM, Woo MY, Perry JJ (2015) Sonography of the optic nerve sheath diameter for detection of raised intracranial pressure compared to computed tomography: a systematic review and meta-analysis. J Ultrasound Med Off J Am Inst Ultrasound Med 34(7):1285–1294
Rafay M, Gulzar F, Iqbal N, Sharif S (2020) Prognostic computed tomography scores in traumatic brain injury. Clin Neurol Neurosurg 195(April):105957
Robba C, Graziano F, Rebora P et al (2021) Intracranial pressure monitoring in patients with acute brain injury in the intensive care unit (SYNAPSE-ICU): an international, prospective observational cohort study. Lancet Neurol 20(7):548–558
Robba C, Santori G, Czosnyka M, Corradi F, Bragazzi N, Padayachy L, Taccone FS, Citerio G (2018) Optic nerve sheath diameter measured sonographically as non-invasive estimator of intracranial pressure: a systematic review and meta-analysis. Intensive Care Med 44(8):1284–1294
Sekhon MS, McBeth P, Zou J, Qiao L, Kolmodin L, Henderson WR, Reynolds S, Griesdale DEG (2014) Association between optic nerve sheath diameter and mortality in patients with severe traumatic brain injury. Neurocrit Care 21(2):245–252
Selhorst JB, Chen Y (2009) The optic nerve. Semin Neurol 29(1):29–35
Sheth S, Branstetter BF 4th, Escott EJ (2009) Appearance of normal cranial nerves on steady-state free precession MR images. Radiogr a Rev Publ Radiol Soc North Am Inc 29(4):1045–1055
Sitanaya SN, Kamayanti F, Nugroho HA, Prabowo B (2022) Comparing ultrasonographic optic nerve sheath diameter to head computed tomography scan to predict intracranial pressure elevation. SAGE Open Med 10:205031212210778
Tian HL, Chen H, Wu BS, Cao HL, Xu T, Hu J, Wang G, Gao WW, Lin ZK, Chen SW (2010) D-dimer as a predictor of progressive hemorrhagic injury in patients with traumatic brain injury: analysis of 194 cases. Neurosurg Rev 33(3):359–366
Ueda T, Ishida E, Kojima Y, Yoshikawa S, Yonemoto H (2015) Sonographic optic nerve sheath diameter: a simple and rapid tool to assess the neurologic prognosis after cardiac arrest. J Neuroimaging 25(6):927–930
Verweij BH, Muizelaar JP, Vinas FC (2001) Hyperacute measurement of intracranial pressure, cerebral perfusion pressure, jugular venous oxygen saturation, and laser Doppler flowmetry, before and during removal of traumatic acute subdural hematoma. J Neurosurg 95(4):569–572
Waheed S, Baig MA, Siddiqui E, Jamil D, Bashar M, Feroze A (2018) Prognostic significance of optic nerve sheath diameter on computed tomography scan with severity of blunt traumatic brain injury in the emergency department. J Pak Med Assoc 68(2):268–271
Wang J, Li K, Li H, Ji C, Wu Z, Chen H, Chen B (2020) Ultrasonographic optic nerve sheath diameter correlation with ICP and accuracy as a tool for noninvasive surrogate ICP measurement in patients with decompressive craniotomy. J Neurosurg 133(2):514–520
Zhang J, He M, Song Y, Xu J (2018) Prognostic role of D-dimer level upon admission in patients with traumatic brain injury. Medicine (Baltimore) 97(31):e11774
Zhang X, Medow JE, Iskandar BJ, Wang F, Shokoueinejad M, Koueik J, Webster JG (2017) Invasive and noninvasive means of measuring intracranial pressure: a review. Physiol Meas 38(8):R143–R182
Zhao D-D, Guo Z-D, He S, Yin C (2020) High intracranial pressure may be the initial inducer of elevated plasma D-dimer level after aneurysmal subarachnoid haemorrhage. Int J Neurosci 130(7):694–699
Author information
Authors and Affiliations
Contributions
GF conceived the idea of this study. GF developed the statistical analysis plan and conducted statistical analyses. MM and DM contributed to the interpretation of the results. GF drafted the original manuscript. NM supervised this study. All authors reviewed the draft manuscript and revised it critically for intellectual content. All authors have approved the final version of the manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Clinical Research Ethics Committee of the Japanese Red Cross Society, Kyoto Daini Hospital (Approval ID Sp2022-12).
Informed consent
The ethics committee waived the requirement for informed consent because of the anonymity of data.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain trauma
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Fujiwara, G., Murakami, M., Maruyama, D. et al. Optic nerve sheath diameter as a quantitative parameter associated with the outcome in patients with traumatic brain injury undergoing hematoma removal. Acta Neurochir 165, 281–287 (2023). https://doi.org/10.1007/s00701-022-05479-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05479-1