Abstract
Background
Despite improvements in closure techniques by using a vital nasoseptal flap, the use of sealing materials, and improved neurosurgical techniques, cerebrospinal fluid (CSF) leak after transsphenoidal surgery still is a clinically relevant problem. Liqoseal® (Polyganics bv, Groningen, The Netherlands) is a CE-approved bioresorbable sealant patch for use as an adjunct to standard methods of cranial dural closure to prevent CSF leakage. This study aims to evaluate the application of Liqoseal in transsphenoidal surgery ex vivo and in vivo.
Methods
1. We created an ex vivo setup simulating the sphenoidal anatomy, using a fluid pump and porcine dura positioned on a conus with the anatomical dimensions of the sella to evaluate whether the burst pressure of Liqoseal applied to a bulging surface was above physiological intracranial pressure. Burst pressure was measured with a probe connected to dedicated computer software. Because of the challenging transsphenoidal environment, we tested in 4 groups with varying compression weight and time for the application of Liqoseal. 2. We subsequently describe the application of Liqoseal® in 3 patients during transsphenoidal procedures with intraoperative CSF leakage to prevent postoperative CSF leakage.
Results
1. Ex vivo: The overall mean burst pressure in the transsphenoidal setup was 231 (± 103) mmHg. There was no significant difference in mean burst pressure between groups based on application weight and time (p = 0.227). 2. In Vivo: None of the patients had a postoperative CSF leak. No nose passage problems were observed. One patient had a postoperative meningitis and ventriculitis, most likely related to preoperative extensive CSF leakage. Postoperative imaging did not show any local infection, swelling, or other device-related adverse effects.
Conclusions
We assess the use of Liqoseal® to seal a dural defect during an endoscopic transsphenoidal procedure as to be likely safe and potentially effective.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrospinal fluid (CSF) leak is a frequent complication after transsphenoidal surgery (TSS), with an overall prevalence of 3.4% [7]. The prevalence of CSF leak for indications other than pituitary adenomas (i.e., craniopharyngioma, meningioma, Rathke’s cleft cysts) is 7.1%, which is similar to that found for craniotomies [7]. CSF leak is associated with various complications such as meningitis, CSF hypotension syndrome, and intracerebral hemorrhage causing increased morbidity and mortality [4, 8]. Furthermore, hospital costs for patients with CSF leak after TSS are significantly higher than for patients without [4, 11].
Despite improvements in closure techniques by using a vital nasoseptal flap (NSF), the use of sealing materials, and improved neurosurgical techniques, CSF leak after TSS still is a clinically relevant problem, for intradural and invasive lesions, such as craniopharyngiomas or tuberculum sellae meningiomas, especially. Retrospective analyses of the use of a patch sealant, TachoSil (Takeda Pharmaceuticals, Tokyo, Japan), in TSS show variable postoperative CSF leak results ranging from 0.8 to 7.8% [2, 3, 12]. For liquid sealants, Tisseel (Baxter, Deerfield, USA) and DuraSeal (Integra Lifesciences, Princeton, USA), similar results have been reported in retrospective analyses with postoperative CSF leak ranging from 1 to 12.5% [13, 14]. Pereira et al. [14] did not find a statistically significant difference in postoperative CSF leak for the use of Tisseel® or DuraSeal®. To further improve the advancement of TSS effective solutions to prevent postoperative CSF leaks are warranted.
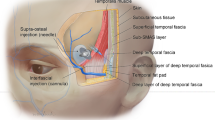
Liqoseal (Polyganics bv, Groningen, The Netherlands) is a CE (Conformité Européenne) approved bioresorbable sealant patch for use as an adjunct to standard methods of cranial dural closure. The patch is composed of a white foam layer containing Polyethylene glycol-N-hydroxysuccinimide, the adhesive component, and buffer salt [10]. The blue layer is made of polyurethane and provides the watertight seal (Fig. 1) [10]. The first in the human study (ENCASE) has shown that the patch is safe and potentially efficacious for reducing CSF leakage after intracranial surgery [10, 15].

Reproduced with permission from the copyright owner [10]: Van Doormaal TPC, Germans MR, Sie M, Brouwers B, Fierstra J, Depauw PRAM, Robe PA, Regli L. Single-arm, open-label, multicenter study to evaluate the safety and performance of dura sealant patch in reducing cerebrospinal fluid leakage following elective cranial surgery: the ENCASE Trial Study Protocol. Neurosurgery. 2020 Feb 1;86(2):E203-E208. Website URL: https://journals.lww.com/neurosurgery/Fulltext/2020/02000/Single_Arm,_Open_Label,_Multicenter_Study_to.36.aspx. Neurosurgery is the official journal of the congress of neurological surgeons. The creative commons license does not apply to this content. Use of the material in any format is prohibited without written permission from the publisher, Wolters Kluwer Health, Inc. Please contact permissions@lww.com for further information
Liqoseal. Length 8 cm, width 8 cm, weight 1600 to 2000 mg.
TSS is regarded as a form of cranial surgery, and thus Liqoseal® application is not off-label [6]. However, the surrounding tissue and dimensions in this approach are different compared to a craniotomy. Therefore, this study evaluates the application of Liqoseal® in TSS in preclinical (ex vivo) settings and 3 endoscopic transsphenoidal cases.
Methods
Ex vivo
Model
We created an ex-vivo transsphenoidal burst pressure model by adapting an earlier published dural sealing model [16, 9] with a conus in the shape of the sella to mimic the application area (Fig. 2A). The dimensions of the conus (17 × 7.5 mm) were based on measurements of the pituitary gland and sella turcica on 23 anonymized MRI scans of patients with pituitary adenomas.
Cranial porcine dura was harvested at an abattoir and cut into circles with a 30 mm diameter. A circular gap of 3 mm was punched out in the center. Liqoseal® was cut into circles of 15 mm in diameter. The dura was clamped above the open pressure chamber and the Liqoseal® was applied manually to cover the gap from the outside with a 5 mm overlap.
Liqoseal® was compressed by equally and continuously applying a standardized weight on a moist gauze for a specified time period. For the cranial application of Liqoseal® a compression time of 2 min with a compression weight of 1 kg was used, to allow optimal adhesion by the formation of amide bonds between the foam layer of the patch and the dura mater [16]. However, the difficult corridor in TSS could, in practice, result in the prescribed application pressure not being met. Therefore, the acute burst pressure was evaluated with a compression weight of 1 kg and 0,25 kg. Furthermore, a shorter compression time would be clinically advantageous. Hence, we compared acute burst pressure for compression times of 2 min and 1 min, respectively.
A fluid pump with a constant flow of 2.0 mL/min of artificial CSF (EcoCyte Bioscience, Germany) was used to increase the pressure in the chamber. The pressure was continuously measured using a blood pressure probe (AD instruments MLT0670 Disposable BP transducer) connected to a computer using LabChart v8.1.14 software (ADInstruments, Australia). Burst pressure was defined as the maximum pressure in millimeters of mercury (mmHg) determined on the continuous measurement in LabChart (Fig. 2B) at the moment of fluid leakage. The aim of these experimental set-ups was to determine if Liqoseal would adhere to the dura with mean burst pressure above the higher end of the physiological intracranial pressure range (> 30 mmHg) [1] on a surface resembling the shape of the sella with varying compression weight and time during application.
Statistics
The required sample size to detect statistically significant differences between groups with an alpha of 0.05 and power of 90% was determined at 23 measurements per subgroup, using the power analysis for One-way Analysis of Variance (ANOVA). Input for sample size calculation was based on the results of the previous cranial and spinal measurements [16]. A total of 3 additional measurements were planned per subgroup to allow for loss of measurements due to experimental failure, so in total 104 measurements were performed. The four groups varying in compression weight (1 kg vs. 0.25 kg) and time (1 min vs. 2 min) were compared using ANOVA. Post hoc Bonferroni correction was applied to adjust for multiple comparisons. Spearman’s rank-order correlation was used to evaluate the association between burst pressure and the interval between measurement and harvesting of the dura. All analyses were performed in SPSS version 27 (IBM).
In vivo
We performed a retrospective evaluation of all transsphenoidal surgeries in which Liqoseal® was used in the University Hospital of Zurich, Switzerland, between the 3rd of January 2020 (when Liqoseal® was approved) and the 1st of March 2022. Three Liqoseal applications were performed in these procedures. Liqoseal® was applied on the outside of the defect in all cases. All 3 patients provided a general informed consent for the use of all clinical data and imaging for research.
Results
Ex vivo
A total of 100 measurements were included in the analysis. Four measurements were excluded from the analysis because leakage in the experimental setup prevented adequate pressure built-up. The overall mean burst pressure in the transsphenoidal setup was 231 (± 103) mmHg (Fig. 3, Table 1). There was no significant difference in mean burst pressure between groups based on application time and weight (p = 0.227).
Spearman’s rank-order correlation showed no significant correlation between mean burst pressure and the interval between experiment and harvesting (rs = 0.031, p = 0.759).
In Vivo
Liqoseal® was applied in 3 endoscopic transsphenoidal surgeries until March 1, 2022.
Case 1
Patient 1 (63 years old male) was diagnosed with a hormone-inactive growing gonadotrophic macroadenoma (Fig. 4, Table 2, Supplementary Information 1). Intraoperatively an evident CSF leak occurred (Fig. 5A). The patient was operated using the mononostril “chopstick” approach with the aim to preserve healthy mucosal tissue [5]. Considering the small size of the defect, preparing an NSF resulting in damage to the nasal mucosa was not considered favorable. Therefore, it was decided to seal with Liqoseal® combined with external lumbar drainage (ELD). A piece of plastic was used to assess the size of the bony defect in the sella. A circular piece of Liqoseal® was cut with 10 mm margin at all sides. After trying several folding options, the piece was folded in 2 with the white side out and parachuted in holding the patch at the front tip to pull the patch forward instead of pushing it. After positioning, a series of small cottonoids was positioned over the Liqoseal® before compressing for 2 min with a 90-degree ring curette. This led to a good adherence over bone and sella region. However, a small bottom part of the sealant was hampered by loose mucosa. The Liqoseal® could be removed with a gentle pulling force via the forceps. The basal bone was cleaned, mucosa removed and a second circular piece of the same patch of Liqoseal® was applied that covered the whole sella defect with a margin of 10 mm (Fig. 5B). Positive end-expiratory pressure (PEEP) test was performed (20 cm H2O for 20 s) showing no leakage. The patch was covered with Tisseel® and to prevent the patch from being exposed to air and Spongostan (Ethicon, Raritan, USA) to further cover the patch and mucosa, to fill up the cavity and provide additional tissue support (Fig. 5C). A nasal packing was put in place to further provide support to the surrounding tissues and to tamponade any small bleeding afterwards. Postoperatively, no rhinoliquorrhea was observed. The ELD was removed at day 6. Patient was discharged day 8 after surgery without complications. Three-month endoscopic control showed complete re-endothelialization (Fig. 5D). At further MRI follow-up (Fig. 6) individual patch recognition was not possible, but no signs of infection or swelling of the patch were observed. During the entire follow-up period of 15 months, there were no nasal complaints and good olfactory function.
Case 2
Patient 2 (54 years old female) was diagnosed with a giant macroadenoma causing bitemporal hemianopsia (Fig. 7, Table 2, Supplementary Information 1). First surgery (day -17) was complicated by postoperative rhinorliquorrhea. A revision surgery was performed using a vascularized NSF to seal the defect and decreasing CSF pressure with ELD (day -7). The leakage continued postoperatively despite increasing CSF drainage volume. During the second revision surgery (day 0) a defect just above the vital NSF was observed (Fig. 8A). As salvage treatment a fat plug was placed in the small defect. Subsequently, Liqoseal was inserted with the same method as described in patient 1 (Fig. 8B–C). PEEP test (20 cm H2O for 20 s) showed no intraoperative leakage. The patch was covered with Tisseel® and Spongostan®. A nasal packing was put in place. No rhinoliquorrhea was observed after this surgery. Patient developed a combined meningitis and ventriculitis at day 4 after the 3rd surgery, which was treated with intravenous antibiotics. The ELD was exchanged for an external ventricular drain (EVD) at this day to treat the infection and resulting hydrocephalus. The treating neurosurgeon did not consider Liqoseal® as the source of the infection, hence the nose was not surgically revised. At day 12 an MRI was made (Fig. 9). Individual Liqoseal® patch recognition was not possible and there were no signs of infection or swelling of the patch. Temporary closure of the EVD resulted repeatedly in hydrocephalus (still without leakage). Therefore, a ventriculoperitoneal shunt was placed at day 40. Patient was discharged at day 44. Final follow-up was 6 months after the surgery in which Liqoseal® was applied. Visual disturbances persisted. Patient-reported no nasal complaints and good olfactory function. She refused further follow-up.
Case 3
Patiënt 3 (7 years old female) presented with an abducens nerve palsy caused by a clivus chordoma (Fig. 10, Table 2, Supplementary Information 1). After resection a large defect in the clivus resulted with a central dural defect (Fig. 11A). A NSF was not prepared and it was considered by the operating surgeon that it would be difficult in this case to make it large enough to cover the total defect appropriately. However, no dural sealants have been CE approved for use in children. So on the discretion of the operating surgeons Liqoseal® was chosen to be used off-label. This application area was deeper and flatter than in the previous 2 patients. This caused the Liqoseal® application to be more difficult and a re-application was necessary. The final positioning showed wrinkles and internal Liqoseal® folds (Fig. 11B). The operating surgeon however decided to leave the patch in place because the dural defect was covered. The Liqoseal® was covered with a fat plug harvested from the periumbilical region (Fig. 11C). Tisseel® and fat were thereafter alternately applied. Finally, the construct was covered with Spongostan® to further fill the cavity and deliver additional tissue support (Fig. 11D). No PEEP test was performed. Because of the high risk of postoperative leakage associated with the dural defect an ELD was placed intraoperatively as well. Postoperatively, no rhinoliquorrhea was observed. The ELD was removed at day 8. No postoperative complications occurred and patient was discharged at day 12 after surgery. Intraoperative and postoperative MRI showed a small chordoma rest at the cavernous sinus which was considered inoperable. The patient was radiated with proton beam 7 weeks after surgery. Latest follow-up was at 7 months after surgery. The abducens paresis persisted. Patient showed good nasal passage and olfactory function up until this time. MRI control at this timepoint showed no swelling of the Liqoseal® patch and slow resolving of the fat plug (Fig. 12).
Discussion
This is the first study that evaluates the application of Liqoseal® during TSS. We report excellent ex vivo and in vivo results. The overall mean burst pressure of Liqoseal® in this transsphenoidal model (231 ± 103 mmHg) and mean burst pressures in individual groups based on compression weight and time were all well above physiological intracranial pressure [1]. Mean burst pressure in this model was shown to be similar to those found in our cranial and spinal model (145 ± 39 mmHg and 233 ± 81 mmHg, respectively) [16].
Liqoseal® was successfully applied during endoscopic endonasal surgery in 3 patients. Given their clinical history, each of these patients can be considered as high risk for postoperative CSF leakage. None of these patients’ postoperative CSF leakage required revision surgery or had nasal passage problems. There was one infectious complication in patient 2 that occurred 4 days after the implantation of the device. This patient was at increased risk for infection because of continuous CSF leakage prior to the surgery in which Liqoseal® was applied, and the infection was treatable with antibiotics [4]. We deem the infection unlikely to be device-related. We found no indications of safety issues for the transsphenoidal application of Liqoseal® based on these 3 patients.
Limitations
The most important limitation of the current study is the small number of TSS cases in which Liqoseal® has been applied which does not allow for any conclusions about efficacy. Moreover, all patients in this study received an intraoperative ELD to decrease the CSF pressure and support the healing of the dura which may have positively contributed to the prevention of CSF leakage and the functioning of the patch. In addition, fibrin glue (Tisseel®) and gelatin sponge (Spongostan®) were used as a coverage. Furthermore, endoscopic inspection of the nasal mucosa (not standard of care) was performed in one patient only, showing re-endothelization.
Finally, the experimental model was designed based on the sella region. This is representative for the majority of transsphenoidal cases, but not all of them. For example, patient 3 had a clivus tumor that grew under the sella and the surface of this region does not resemble the surface of the ex vivo model. Furthermore, the gap size in the dura in the experimental setup was 3 mm in diameter. In clinical practice, the gap size in the dura, especially in cases leading to CSF leak postoperatively, may in fact be larger.
Recommendations
Based on our experience in these first 3 cases, we think that there are a number of technical aspects to take into consideration when applying Liqoseal® in TSS. Firstly, we recommend patch sizing to allow for margins of minimally 5 mm, taking into consideration that a larger sized patch is more difficult to introduce. When fat tissue is placed under Liqoseal®, we recommend a margin of 10 mm as Liqoseal® does not adhere to fat. Secondly, we recommend to fold the patch with the white side (PEG-NHS side) outwards. This has the advantage of easier unfolding, yet does expose the foam layer to possible absorption of blood and damage. Thirdly, the patch should be held at the most distal point with a small rongeur while being introduced in the nose to exert a pulling force on the patch instead of a pushing force. Fourthly, in these 3 cases, compression for 2 min using moistened cottonoids and a patty was performed with a 90-degree bended ring curette. Despite the results of the ex vivo experiments showing that 1 min compression appears to be sufficient, we still recommend to compress for a minimum of 2 min as stated in the instructions for use for security and consistency reasons. Finally, the dural defects in the cases presented in this article were relatively small. Liqoseal® is intended for use on defects with a maximum size of 3 mm. Use over larger defects is thus off-label. We recommend to use Liqoseal® in cases with larger defects with caution and only in combination with a construct allowing endothelization and formation of new dura (i.e., covering the mucosal tissue with muscle tissue or fat). It is important to note that Liqoseal does not adhere to fat tissue and that fat tissue will resorb over time. Considering the relatively fast endothelization we have observed, the primary goal of using Liqoseal® in such cases is to overcome the time until endothelization without CSF leakage.
Conclusion
Data Availability
Data is available from the corresponding author upon reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- CE:
-
Conformité Européenne
- CSF:
-
Cerebrospinal fluid
- ELD:
-
External lumbar drain
- EVD:
-
External ventricular drain
- MRI:
-
Magnetic resonance imaging
- mm:
-
Millimeters
- cm:
-
Centimeters
- mmHg:
-
Millimeters of mercury
- N:
-
Number
- NSF:
-
Nasoseptal flap
- PEEP:
-
Positive end-expiratory pressure
- TSS:
-
Transsphenoidal surgery
- USA:
-
United States of America
References
Albeck MJ, Børgesen SE, Gjerris F, Schmidt JF, Sørensen PS (1991) Intracranial pressure and cerebrospinal fluid outflow conductance in healthy subjects. J Neurosurg. https://doi.org/10.3171/jns.1991.74.4.0597
Hong CK, Kim YB, Hong JB, Lee KS (2015) Sealing of cerebrospinal fluid leakage during conventional transsphenoidal surgery using a fibrin-coated collagen fleece. J Clin Neurosci. https://doi.org/10.1016/j.jocn.2014.10.019
Jiménez Zapata HD, Rodríguez Berrocal V, ViorFernández C, Sánchez FM, GarcíaFernández A (2020) Sellar diaphragm reconstruction with tachosil during endoscopic endonasal surgery: technical note. J Neurol Surg B Skull Base. https://doi.org/10.1055/s-0039-1688781
Parikh A, Adapa A, Sullivan SE, McKean EL (2020) Predictive factors, 30-day clinical outcomes, and costs associated with cerebrospinal fluid leak in pituitary adenoma resection. J Neurol Surg B. https://doi.org/10.1055/s-0039-1679896
Serra C, Staartjes VE, Maldaner N, Holzmann D, Soyka MB, Gilone M, Schmid C, Tschopp O, Regli L (2020) Assessing the surgical outcome of the “chopsticks” technique in endoscopic transsphenoidal adenoma surgery. Neurosurg Focus. https://doi.org/10.3171/2020.3.FOCUS2065
Shah A, Mohamed Elsanafiry MS (2018) Diaphragma sellae: anatomical and surgical implication in surgery for pituitary adenomas - highlighting contributions by Goel. J Craniovertebr Junction Spine. https://doi.org/10.4103/jcvjs.JCVJS_85_18
Slot EMH, Sabaoglu R, Voormolen EHJ, Hoving EW, van Doormaal TPC (2021) Cerebrospinal fluid leak after transsphenoidal surgery: a systematic review and meta-analysis. J Neurol Surg B Skull Base. https://doi.org/10.1055/s-0041-1733918
Van Aken MO, Feelders RA, de Marie S et al (2004) Cerebrospinal fluid leakage during transsphenoidal surgery: postoperative external lumbar drainage reduces the risk for meningitis. Pituitary. https://doi.org/10.1007/s11102-005-5351-3
Van Doormaal T, Kinaci A, van Thoor S, Redegeld S, Bergmann W, van der Zwan A (2018) Usefulness of sealants for dural closure: evaluation in an in vitro model. Operative Neurosurgery. https://doi.org/10.1093/ons/opx260
Van Doormaal TPC, Germans MR, Sie M et al (2019) Single-arm, open-label, multicenter study to evaluate the safety and performance of dura sealant patch in reducing cerebrospinal fluid leakage following elective cranial surgery: the ENCASE trial study protocol. Neurosurgery. https://doi.org/10.1093/neuros/nyz396
Grotenhuis JA (2005) Costs of postoperative cerebrospinal fluid leakage: 1-year, retrospective analysis of 412 consecutive nontrauma cases. Surg Neurol, https://doi.org/10.1016/j.surneu.2005.03.041
Jolly K, Gupta KK, Egbuji O, Naik PP, Ahmed SK (2021) Endoscopic transsphenoidal surgery reconstruction using the fibrin sealant patch Tachosil® British. J Neurosurg, https://doi.org/10.1080/02688697.2021.1905771
Burkett CJ, Patel S, Tabor MH, Padhya T, Vale FL (2011) Polyethylene glycol (PEG) hydrogel dural sealant and collagen dural graft matrix in transsphenoidal pituitary surgery for prevention of postoperative cerebrospinal fluid leaks. J Clin Neurosci. https://doi.org/10.1016/j.jocn.2011.04.005
Pereira EAC, Grandidge CA, Nowak VA, Cudlip SA (2017) Cerebrospinal fluid leaks after transsphenoidal surgery – effect of a polyethylene glycol hydrogel dural sealant. J Clin Neurosci. https://doi.org/10.1016/j.jocn.2017.06.016
Van Doormaal T, Germans MR, Sie M, et al. (2021) Single-arm, open-label, multicentre first in human study to evaluate the safety and performance of dural sealant patch in reducing CSF leakage following elective cranial surgery: the ENCASE trial BMJ Open. https://doi.org/10.1136/bmjopen21-049098
Kinaci A, van Thoor S, Redegeld S, Tooren M, van Doormaal TPC (2021) Ex vivo evaluation of a multilayered sealant patch for watertight dural closure: cranial and spinal models. J Mater Sci: Mater Med, https://doi.org/10.1007/s10856-021-06552-4
Kinaci A, Algra A, Heuts S, O’Donnell D, van der Zwan A, van Doormaal T (2018) Effectiveness of dural sealants in prevention of cerebrospinal fluid leakage after craniotomy: a systematic review world neurosurgery. https://doi.org/10.1016/j.wneu.2018.06.196
Kinaci A, Bergmann W, Bleys RL, van der Zwan A, van Doormaal TP (2020) Histologic comparison of the dura mater among species comp med, https://doi.org/10.30802/AALAS-CM-19- 000022
Kinaci A, Bergmann W, Thoor S, Redegeld S, Zwan A, Doormaal TPC. Safety and biodegradability of a synthetic dural sealant patch (Liqoseal) in a porcine cranial model (2021) Anim Models and Exp Med, https://doi.org/10.1002/ame2.12184
Author information
Authors and Affiliations
Contributions
Conceptualization: Tristan van Doormaal; Methodology: Tristan van Doormaal, Nadia Colmer, Emma Slot, Formal analysis and investigation: Emma Slot, Tristan van Doormaal; Surgeries: Tristan van Doormaal, Carlo Serra, David Holzmann, Luca Regli; Writing—original draft preparation: Emma Slot, Tristan van Doormaal; Writing—review and editing: all authors; Supervision: Tristan van Doormaal.
Corresponding author
Ethics declarations
Ethics approval
All patients provided written informed consent on the use of their data, including video and photo material, for research and reporting purposes.
Informed consent
General informed consent for the use of all clinical data and imaging for research.
Conflict of interest
E.M.H.S. received a research grant through Polyganics b.v.
T.P.C.vD is a consultant for Polyganics b.v.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgical technique evaluation
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file2 (MP4 376654 KB) Video part 1. Summarized videography of the first application in case 1.
Supplementary file3 (MP4 474575 KB) Video part 2. Summarized videography of the second application in case 1.
Supplementary file4 (MP4 391765 KB) Video part 3. Summarized videography of case 2.
Supplementary file5 (MP4 476432 KB) Video part 4. Summarized videography of case 3.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Slot, E.M.H., Colmer, N., Serra, C. et al. Ex vivo and in vivo evaluation of transsphenoidal Liqoseal application to prevent cerebrospinal fluid leakage. Acta Neurochir 165, 1511–1521 (2023). https://doi.org/10.1007/s00701-022-05477-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05477-3