Abstract
Purpose
Overdrainage (OD) is one of the most frequent complications related to drainage of the cerebrospinal fluid (CSF). It is mostly associated with valve-bearing shunt systems but should probably be considered as a risk factor in any type of CSF diversion procedure. There is extreme variation in the reported incidence of OD due to the lack of consensus on defining criteria and an unclear perception of the pathophysiology. Hence, OD is probably underreported and underestimated. The objective of this paper was to establish a definition of OD, based on a systematic review of the literature.
Methods
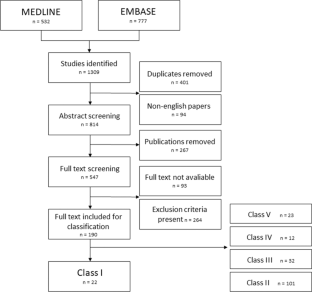
A systematic search was conducted in MEDLNE and EMBASE. Studies providing a definition or a description of diagnostic findings related to OD in ventriculoperitoneal shunt treated hydrocephalus were included. Non-English titles, abstracts and manuscripts were excluded. Extracted descriptions were graded into five groups (class I-V studies) based on how precise the terminology used to describe OD was. Class I studies were included for further analysis and characteristics of OD were extracted. The quality of included descriptions was assessed by a clinical expert panel.
Results
A total of 1309 studies were screened, 190 were graded into groups, and 22, which provided specific definitions or descriptions of OD, were graded as class I studies. We extracted 32 different characteristics consistent with OD (e.g., clinical symptoms, radiological signs, and syndromes).
Conclusion
There was an overall agreement that CSF overdrainage following implantation of a ventriculoperitoneal shunt in a mixed pediatric and adult population is characterized as a persistent condition with clinically manifestations as postural dependent headache, nausea, and vomiting and/or radiological signs of slim ventricles and/or subdural collections.

Similar content being viewed by others
References
Becker DP, Nulsen FE (1968) Control of hydrocephalus by valve-regulated venous shunt: avoidance of complications in prolonged shunt maintenance. J Neurosurg 28(3):215–226
Beni-Adani L, Siomin V, Segev Y, Beni S, Constantini S (2000) Increasing chronic subdural hematoma after endoscopic III ventriculostomy. Child’s Nerv Syst 16(7):402–405
Chan SM, Chodakiewitz YG, Maya MM, Schievink WI, Moser FG (2019) Intracranial hypotension and cerebrospinal fluid leak. Neuroimaging Clin N Am 29(2):213–226
Chari A, Dasgupta D, Smedley A, Craven C, Dyson E, Matloob S, Thompson S, Thorne L, Toma AK, Watkins L (2017) Intraparenchymal intracranial pressure monitoring for hydrocephalus and cerebrospinal fluid disorders. Acta Neurochir (Wien) 159(10):1967–1978
Decq P, Barat J-L, Duplessis E, Leguerinel C, Gendrault P, Keravel Y (1995) Shunt failure in adult hydrocephalus: flow-controlled shunt versus differential pressure shunts—a cooperative study in 289 patients. Surg Neurol 43(4):333–339
Desai VR, Sadrameli SS, Jenson AV, Asante SK, Daniels B, Trask TW, Britz G (2020) Ventriculoperitoneal shunt complications in an adult population: a comparison of various shunt designs to prevent overdrainage. Surg Neurol Int 11:269
Di Rocco C (1994) Is the slit ventricle syndrome always a slit ventricle syndrome? Child’s Nerv Syst 10(1):49–58
Diesner N, Freimann F, Clajus C, Kallenberg K, Rohde V, Stockhammer F (2016) Female gender predisposes for cerebrospinal fluid overdrainage in ventriculoperitoneal shunting. Acta Neurochir (Wien) 158(7):1273–1278
Feletti A, D’Avella D, Wikkelsø C et al (2019) Ventriculoperitoneal shunt complications in the European idiopathic normal pressure hydrocephalus multicenter study. Oper Neurosurg 17(1):97–102
Fouyas IP, Casey ATH, Thompson D, Harkness WF, Hayward RD (1996) Use of intracranial pressure monitoring in the management of childhood hydrocephalus and shunt-related problems. Neurosurgery 38(4):726–732
Freimann FB, Sprung C (2012) Shunting with gravitational valves - Can adjustments end the era of revisions for overdrainage-related events? J Neurosurg 117(6):1197–1204
Hall BJ, Gillespie CS, Hennigan D, Bagga V, Mallucci C, Pettorini B (2021) Efficacy and safety of the Miethke programmable differential pressure valve (proGAV®2.0): a single-centre retrospective analysis. Child’s Nerv Syst 37(8):2605–2612
Henderson D, Budu A, Zaki H, Sinha S, de Lacy P, McMullan J, Ushewokunze S (2020) A comparison between flow-regulated and adjustable valves used in hydrocephalus during infancy. Child’s Nerv Syst 36(9):2013–2019
Hung AL, Vivas-Buitrago T, Adam A, Lu J, Robison J, Elder BD, Goodwin CR, Jusué-Torres I, Rigamonti D (2017) Ventriculoatrial versus ventriculoperitoneal shunt complications in idiopathic normal pressure hydrocephalus. Clin Neurol Neurosurg 157(February):1–6
Hung C-W, Lin W-C, Chang W-N et al (2018) Risk factors and outcomes of cerebrospinal fluid overdrainage in HIV-negative patients with cryptococcal meningitis after the ventriculoperitoneal shunting procedure. J Microbiol Immunol Infect 51(4):545–551
Iglesias S, Ros B, Martín Á et al (2017) Factors related to shunt survival in paediatric hydrocephalus. Could failure be avoided? Neurocirugia 28(4):159–166
Kajimoto Y, Ohita T, Miyake H, Matsukawa M, Ogawa D, Nagao K, Kuroiwa T (2000) Posture-related changes in the pressure environment of the ventriculoperitoneal shunt system. J Neurosurg 93:614–617
Kestle JRW (2003) Pediatric hydrocephalus: current management. Neurol Clin 21(4):883–895
Khan QU, Wharen RE, Grewal SS, Thomas CS, Deen HG, Reimer R, Van Gerpen JA, Crook JE, Graff-Radford NR (2013) Overdrainage shunt complications in idiopathic normal-pressure hydrocephalus and lumbar puncture opening pressure. J Neurosurg 119(6):1498–1502
Kiefer M, Eymann R, Meier U (2002) Five years experience with gravitational shunts in chronic hydrocephalus of adults. Acta Neurochir (Wien) 144(8):755–767
Kimura T, Schulz M, Shimoji K, Miyajima M, Arai H, Thomale U-W (2016) In vitro performance of the fixed and adjustable gravity-assisted unit with and without motion-evidence of motion-induced flow. Acta Neurochir (Wien) 158(10):2011–2018
Kondageski C, Thompson D, Reynolds M, Hayward RD (2007) Experience with the Strata valve in the management of shunt overdrainage. J Neurosurg 106(2 SUPPL.):95–102
Kraemer MR, Sandoval-Garcia C, Bragg T, Iskandar BJ (2017) Shunt-dependent hydrocephalus: management style among members of the American Society of Pediatric Neurosurgeons. J Neurosurg Pediatr 20(3):216–224
Krahulik D, Vaverka M, Hrabalek L, Hampl M, Halaj M, Jablonsky J, Langova K (2020) Ventriculoperitoneal shunt in treating of idiopathic normal pressure hydrocephalus—single-center study. Acta Neurochir (Wien) 162(1):1–7
Lee W-C, Seo D-H, Choe I-S, Park S-C, Ha Y-S, Lee KC (2010) A comparative result of ventriculoperitoneal shunt, focusing mainly on gravity-assisted valve and programmable valve. J Korean Neurosurg Soc 48(3):251–258
Lemcke J, Meier U, Müller C et al (2013) Safety and efficacy of gravitational shunt valves in patients with idiopathic normal pressure hydrocephalus: a pragmatic, randomised, open label, multicentre trial (SVASONA). J Neurol Neurosurg Psychiatry 84(8):850–857
Meier U, Kiefer M, Sprung C (2002) The Miethke Dual-Switch Valve in patients with normal pressure hydrocephalus. Neurosurg Q 12(2):114–121
Meier U, Kiefer M, Sprung C (2004) Evaluation of the Miethke dual- switch valve in patients with normal pressure hydrocephalus. Surg Neurol 61(2):118–119
Meier U, Stengel D, Müller C et al (2013) Predictors of subsequent overdrainage and clinical outcomes after ventriculoperitoneal shunting for idiopathic normal pressure hydrocephalus. Neurosurgery 73(6):1054–1060
Mokri B, Atkinson JL, Piepgras DG (2000) Absent headache despite CSF volume depletion (intracranial hypotension). Neurology 55(11):1722–1724
Naftel RP, Argo JL, Shannon CN et al (2011) Laparoscopic versus open insertion of the peritoneal catheter in ventriculoperitoneal shunt placement: Review of 810 consecutive cases. J Neurosurg 115(1):151–158
Norager NH, Olsen MH, Pedersen SH, Riedel CS, Czosnyka M, Juhler M (2021) Reference values for intracranial pressure and lumbar cerebrospinal fluid pressure: a systematic review. Fluids Barriers CNS 18(1):1–10
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev 5(1):210
Panagopoulos D, Karydakis P, Themistocleous M (2021) Slit ventricle syndrome: historical considerations, diagnosis, pathophysiology, and treatment review. Brain Circ 7(3):167
Panagopoulos D, Stranjalis G, Gavra M, Boviatsis E, Korfias S (2022) Shunt over-drainage, slit ventricle syndrome, programmable valves and anti-siphon devices. A narrative review of a multifactorial and intractable problem. J Integr Neurosci 21(3):84
Pedersen SH, Lilja-Cyron A, Andresen M, Juhler M (2018) The relationship between intracranial pressure and age—chasing age-related reference values. World Neurosurg 110:e119–e123
Pudenz RH, Foltz EL (1991) Hydrocephalus: overdrainage by ventricular shunts. A review and recommendations. Surg Neurol 35(3):200–212
Qvarlander S, Sundstrom N, Malm J, Eklund A (2013) Postural effects on intracranial pressure: modeling and clinical evaluation. J Appl Physiol 115(10):1474–1480
Rekate HL (1993) Classification of slit-ventricle syndromes using intracranial pressure monitoring. Pediatr Neurosurg 19(1):15–20
Rekate HL (2004) The slit ventricle syndrome: advances based on technology and understanding. Pediatr Neurosurg 40(6):259–263
Ros B, Iglesias S, Martín Á, Carrasco A, Ibáñez G, Arráez MA (2018) Shunt overdrainage syndrome: review of the literature. Neurosurg Rev 41(4):969–981
Ros B, Iglesias S, Linares J, Cerro L, Casado J, Arráez MA (2021) Shunt overdrainage: reappraisal of the syndrome and proposal for an integrative model. J Clin Med. https://doi.org/10.3390/jcm10163620
Sainz LV, Hockel K, Schuhmann MU (2018) Chronic overdrainage syndrome: pathophysiological insights based on ICP analysis: a case-based review. Child’s Nerv Syst 34(3):401–408
Saukkonen AL, Serlo W, von Wendt L (1988) Electroencephalographic findings and epilepsy in the slit ventricle syndrome of shunt-treated hydrocephalic children. Childs Nerv Syst 4(6):344–347
Serlo W, Heikkinen E, Saukkonen AL, von Wendt L (1985) Classification and management of the slit ventricle syndrome. Child’s Nerv Syst 1(4):194–199
Sklar FH, Nagy L, Robertson BD (2012) The use of abdominal binders to treat over-shunting headaches. J Neurosurg Pediatr 9(6):615–620
Tan K, Meiri A, Mowrey WB, Abbott R, Goodrich JT, Sandler AL, Suri AK, Lipton ML, Wagshul ME (2018) Diffusion tensor imaging and ventricle volume quantification in patients with chronic shunt-treated hydrocephalus: a matched case-control study. J Neurosurg 129(6):1611–1622
Toma AK, Tarnaris A, Kitchen ND, Watkins LD (2010) Investigating shunt function using continuous intracranial pressure monitoring in adults: single center experience - clinical article. J Neurosurg 113(6):1326–1330
Trinh VT, Duckworth EAM (2013) Revision to an adjustable non-siphon control valve in low pressure hydrocephalus: Therapeutic siphoning and a new perspective on NPH. Clin Neurol Neurosurg 115(2):175–178
Tschan CA, Antes S, Huthmann A et al (2014) Overcoming CSF overdrainage with the adjustable gravitational valve proSA. Acta Neurochir (Wien) 156(4):767–776
Weinzweig J, Bartlett SP, Chen JC, Losee J, Sutton L, Duhaime A-C, Whitaker LA (2008) Cranial vault expansion in the management of postshunt craniosynostosis and slit ventricle syndrome. Plast Reconstr Surg 122(4):1171–1180
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The manuscript does not contain clinical patient data; thus, an ethical approval was not necessary to conduct the study.
Consent to participate
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery general
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pedersen, S.H., Prein, T.H., Ammar, A. et al. How to define CSF overdrainage: a systematic literature review. Acta Neurochir 165, 429–441 (2023). https://doi.org/10.1007/s00701-022-05469-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05469-3




