Abstract
Background
Laser interstitial thermal therapy (LITT) is a stereotactic neurosurgical procedure used to treat neoplastic and epileptogenic lesions in the brain. A variety of advanced technological instruments such as frameless navigation systems, robotics, and intraoperative MRI are often described in this context, although the surgical procedure can also be performed using a standard stereotactic setup and a diagnostic MRI suite.
Methods
We report on our experience and a surgical technique using a Leksell stereotactic frame and a diagnostic MRI suite to perform LITT.
Conclusion
LITT can be safely performed using the Leksell frame and a diagnostic MRI suite, making the technique available even to neuro-oncology centers without advanced technological setup.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Relevant surgical anatomy
Laser interstitial thermal therapy (LITT) is a minimally invasive treatment modality for ablation of neoplastic or epileptic lesions by thermal damage. The introduction of reproducible MRI thermometry, with real-time monitoring of thermal damage, allows for a focused ablation while lowering the risk of injury to surrounding structures [2, 4, 6]. LITT offers the advantage to treat an otherwise difficult to reach central nervous system lesion in or near eloquent areas. The potential treatment diameter is around 2–3 cm. With critically located lesions, the precision of laser catheter placement is of utmost importance, to ensure adequate coverage while avoiding collateral damage [6, 8].
Description of the technique
Several stereotactical systems are available for laser catheter placement and the LITT technique is usually associated with an advanced technical setup such as an intraoperative MRI, frameless stereotactic systems, and robotics [2, 8, 3]. Nevertheless, LITT can also be performed using more widely available equipment, such as a stereotactic frame and a diagnostic MRI suite.
The Visualase™ (Medtronic, Inc., Minneapolis MN) LITT device consists of a laser diode (980 nm wavelength, 15-W), laser fiber, and applicator. The diffusing fiber optic comes in two different lengths of energy output: 3 or 10 mm. A cooling channel allows for circulating sterile saline to assure probe tip cooling. A bone anchor is affixed through a 3.2-mm twist drill hole in the skull to retain the laser applicator along the intended trajectory.
The procedure can chronologically be divided into seven steps and is described accordingly in the supplementary video:
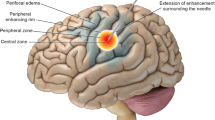
In the first step, (1) preplanning, the lesion is identified on a pre-treatment MRI scan. The images are exported to a neuro-navigation system, along with a preoperative CT scan. Suitable target and entry points are chosen for an optimal trajectory (Fig. 1). During the second step, (2) stereotactic frame placement in the OR, the stereotactic frame is fixed to the patients head under general anesthesia. Imaging for localization with an O arm (multiplane 3D imaging) is performed and coordinates for the target and entry points are retrieved. During step (3) stereotactic arc and laser catheter insertion (Fig. 2), the arc is positioned according to the X, Y, and Z coordinates for the target. A percutaneous burr hole is performed and the dura is punctured. A biopsy needle can be inserted for tissue sampling, if needed. We verify the trajectory before we affix the bone anchor and insert the laser applicator followed by the laser fiber. Finally, the Leksell arc and frame are removed and the patient is transported to the diagnostic MRI suite (Fig. 3). In the fourth step, (4) Pre-treatment MRI, a flex coil is placed around the patient’s head. A gadolinium contrast-enhanced MRI verifies proper positioning of the laser fiber as well as assuring that no complication, such as hemorrhage, has occurred during laser catheter insertion. The MRI is connected to the Visualase system (Fig. 4). Two imaging planes from the temperature map sequence (Tmap) are chosen for continuous thermometry during ablation. The laser fiber and cooling lines are connected to the Visualase console before the fifth step, (5) LITT ablation procedure, is commenced. Temperature markers are set. A low-energy test dose is delivered to confirm heat distribution in the intended area. The energy is then increased for the ablation, with simultaneous irrigation ongoing for cooling of the catheter. The tissue temperature changes as visualized by the Tmap sequence can be seen on the Visualase console, while the lesional damage estimate is calculated by the Visualase system and monitored continuously on the console (Fig. 4). The treatment can be repeated and the catheter can be adjusted along the trajectory as needed to obtain an optimal ablation. During step (6) post treatment MRI to evaluate the final ablation volume and to detect any adverse effects, a diagnostic contrast-enhanced MRI is performed (Fig. 4C). The final step, (7) removal of LITT catheter and subsequent extubation, is performed in the MRI department before transfer to the neurosurgical ward.
Preplanning. A Contrast-enhanced T1 3D volume MRI (BRAVO) sequence shows a tumor recurrence in a patient previously operated for a low-grade glioma in the left fronto-insular region with a new contrast-enhancing lesion near the basal ganglia and cortico-spinal tract (CST). B Preplanning with a volumetry of the lesion (red border), target (T), and entry point (E). A DTI can be incorporated for tractography of the CST (blue), when choosing a suitable entry point for a trajectory and ablation sparing the eloquent areas of the CST. A simulation of the intended ablation can be done by creating a diameter of 10–20 mm to the trajectory (orange)
Stereotactic arc and laser catheter insertion A. A small scalp incision is made, followed by drilling of the bone and puncture of the dura. The entry point should have a favorable angulation to the skull, as perpendicular to the bone surface as possible. After the drilling, the rigid stylet for the bone anchor can be passed intracranially B. We verify the trajectory with the O arm, taking images of the rigid stylet before the bone anchor is fixed to the skull. C. The laser fiber is prepared and D the laser catheter is inserted the predetermined distance and locked in place followed by the insertion and fixation of the laser fiber. E The Leksell arc and frame are removed before the patient is transported to the diagnostic MRI suite
LITT ablation procedure A. High-temperature markers (< 90°) are set in the vicinity of the catheter tip to protect it from overheating and low-temperature markers (< 45–50°) close to critical areas to be protected (in this case the motor fiber tracts). Irrigation is started to ensure cooling of the catheter during treatment. B. A low-energy test dose is delivered to confirm heat distribution in the intended area. The energy is increased for the ablation itself and the tissue temperature changes are followed on the console as color changes on the imaging, while the lesional damage estimate is calculated by the system and monitored continuously on the console. C Contrast-enhanced T1 3D volume MRI (FSPGR) is performed after the ablation and compared to the damage map from the ablation. A contrast-enhancing peripheral ring (in addition to the contrast enhancing tumor) on the post-ablational MRI scan marks the border of the ablated volume which is seen to correspond well with the estimated damage map (orange)
Indications
LITT has been used for the treatment of malignant brain tumors and recurrent and newly diagnosed glioblastoma as well as other high-grade gliomas. The indications in neuro-oncology have continued to expand to include radioresistant brain metastasis and radionecrosis [2, 1, 5]. LITT has also become an established minimally invasive alternative to epilepsy surgery for treating different types of epileptogenic foci, such as cavernoma, mesial temporal lobe sclerosis, focal cortical dysplasia, and hypothalamic hamartoma [7, 10]. At our institution, we have treated both neoplastic and epileptogenic lesions. We find the accuracy of the stereotactic frame to be favorable in the treatment of small lesions in critical areas such as the ablation of hypothalamic hamartomas or lesions near the cortico-spinal tract as illustrated in our video.
Limitations
Performing LITT with the Leksell frame and a diagnostic MRI suite has its advantages but also limitations. The main advantage is the broad applicability of the procedure without the need for further technical setup such as an intraoperative MRI or robotics.
An obvious limitation to performing the ablation in a diagnostic MRI suite is that it does not allow for altering of the trajectory once the Leksell frame has been removed and the patient transported to the diagnostic MRI suite. Other limitations are those inherent to the LITT treatment such as lesion size and geometry or difficult locations without a safe trajectory for catheter placement [2, 6, 8].
How to avoid complications
Meticulous planning of the catheter placement, avoiding trajectories through critical structures and large vessels, is mandatory for a successful laser ablation and to avoid complications such as catheter malplacement and hemorrhage. Another key point to avoid laser misplacement is the angulation to the skull to avoid the drill bit from slipping on the bony curvature [9].
The risk of hemorrhagic complications during placement can further be minimized by adequate durotomy before insertion of the laser catheter.
Hyperthermic complications should be avoided by careful placement of temperature markers close to any critical structures so the laser is automatically deactivated before hyperthermia occurs in these areas.
Finally, pre-treatment imaging used for preplanning should be recent (< 1 week), especially for fast-growing tumors where a potential increase in volume might prevent coverage of the whole lesion. Similarly, attention needs to be paid to the risk of excessive edema increasing with the ablation volume [2, 5].
Specific perioperative considerations
Preoperative workup includes MRI and CT imaging, pre-anesthesia evaluation, and coagulation tests. Postoperatively, the patient is in a recovery unit for 2–4 h before transfer to the neurosurgical ward and discharged after 24 h observation with corticosteroid tapering over the course of 2 weeks.
Specific information for the patient
LITT offers a minimally invasive treatment, a short hospital stay, and fast recovery. However, the patient has to be informed about the possibility of adverse events, i.e., hemorrhage and neurological deficits due to misplacement of the catheter or other adverse events due to hyperthermia in critical/eloquent areas or post-procedural swelling. More importantly, the patient needs to be informed about the limitations of the treatment in terms of ablation volume. Thus, LITT is recommended for patients with lesions of appropriate size, shape, and location, assuring maximal ablation coverage while minimizing the risk of adverse events.
Data Availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
References
Alattar AA, Bartek J Jr, Chiang VL, Mohammadi AM, Barnett GH, Sloan A, Chen CC (2019) Stereotactic laser ablation as treatment of brain metastases recurring after stereotactic radiosurgery: a systematic literature review. World Neurosurg 128:134–142. https://doi.org/10.1016/j.wneu.2019.04.200
Ashraf O, Patel NV, Hanft S, Danish SF (2018) Laser-induced thermal therapy in neuro-oncology: a review. World Neurosurg 112:166–177. https://doi.org/10.1016/j.wneu.2018.01.123
Bartek J Jr, Alattar A, Jensdottir M, Chen CC (2019) Biopsy and ablation of H3K27 glioma using skull-mounted smartframe device: technical case report. World Neurosurg 127:436–441. https://doi.org/10.1016/j.wneu.2019.04.029
Carpentier A, McNichols RJ, Stafford RJ, Guichard JP, Reizine D, Delaloge S, Vicaut E, Payen D, Gowda A, George B (2011) Laser thermal therapy: real-time MRI-guided and computer-controlled procedures for metastatic brain tumors. Lasers Surg Med 43:943–950. https://doi.org/10.1002/lsm.21138
Chen C, Lee I, Tatsui C, Elder T, Sloan AE (2021) Laser interstitial thermotherapy (LITT) for the treatment of tumors of the brain and spine: a brief review. J Neurooncol 151:429–442. https://doi.org/10.1007/s11060-020-03652-z
Jethwa PR, Barrese JC, Gowda A, Shetty A, Danish SF (2012) Magnetic resonance thermometry-guided laser-induced thermal therapy for intracranial neoplasms: initial experience. Neurosurgery 71(133–144):144–135. https://doi.org/10.1227/NEU.0b013e31826101d4
North RY, Raskin JS, Curry DJ (2017) MRI-guided laser interstitial thermal therapy for epilepsy. Neurosurg Clin N Am 28:545–557. https://doi.org/10.1016/j.nec.2017.06.001
Patel NV, Mian M, Stafford RJ, Nahed BV, Willie JT, Gross RE, Danish SF (2016) Laser interstitial thermal therapy technology, physics of magnetic resonance imaging thermometry, and technical considerations for proper catheter placement during magnetic resonance imaging-guided laser interstitial thermal therapy. Neurosurg 79(Suppl 1):S8–S16. https://doi.org/10.1227/NEU.0000000000001440
Pruitt R, Gamble A, Black K, Schulder M, Mehta AD (2017) Complication avoidance in laser interstitial thermal therapy: lessons learned. J Neurosurg 126:1238–1245. https://doi.org/10.3171/2016.3.JNS152147
Zemmar A, Nelson BJ, Neimat JS (2020) Laser thermal therapy for epilepsy surgery: current standing and future perspectives. Int J Hyperthermia 37:77–83. https://doi.org/10.1080/02656736.2020.1788175
Acknowledgments
We acknowledge the help of NOCRiiC with this paper.
Funding
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical considerations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from the patient.
Conflict of interest
Margret Jensdottir and Jiri Bartek Jr. have received speaker’s honoraria from Medtronic. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
1. LITT is a minimally invasive surgical procedure that can be used to treat a variety of neoplastic and epileptogenic lesions.
2. LITT compares favorably with open surgical procedures in terms of overall morbidity, length of hospital stay, and recovery.
3. The Visualase laser system is compatible with several different neurosurgical platforms for stereotaxy, both framebased and frameless, as well as surgical robots.
4. Despite a variety of advanced technical instruments described in literature, the procedure can be performed with a simpler, readily available setup, such as the Leksell stereotactic frame and a diagnostic MRI suite.
5. The accuracy of the stereotaxy is paramount to enable precise laser catheter placement in deep-seated lesions in or near eloquent or critical areas of the brain and to ensure a successful ablation.
6. The laser catheter is secured in its position with a bone anchor that is affixed through a twist drill hole in the skull.
7. The twist drill hole and the bone anchor will define the final trajectory alignment and a favorable angle to the bone (as perpendicular as possible) should always be chosen for the entry point.
8. Meticulous preplanning is mandatory for optimal treatment results and complication avoidance. The patient selection and especially the lesion size and shape are very important.
9. The treatment requires multidisciplinary teamwork approach with neuroradiology, neurosurgery, and neuroanesthesiology.
10. There is mounting retrospective evidence for the efficacy of LITT in treating patients with both tumors and epileptogenic lesions. More prospective and randomized controlled trials are necessary to define the role of LITT in the future.
This article is part of the Topical Collection on Neurosurgery general
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file (MP4 92.5 mb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jensdottir, M., Sandvik, U., Fagerlund, M. et al. Laser interstitial thermal therapy using the Leksell Stereotactic System and a diagnostic MRI suite: how I do it. Acta Neurochir 165, 549–554 (2023). https://doi.org/10.1007/s00701-022-05461-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05461-x