Abstract
Purpose
By using data from the Norwegian Registry for Spine Surgery, we wanted to develop and validate prediction models for non-success in patients operated with anterior surgical techniques for cervical degenerative radiculopathy (CDR).
Methods
This is a multicentre longitudinal study of 2022 patients undergoing CDR surgery and followed for 12 months to find prognostic models for non-success in neck disability and arm pain using multivariable logistic regression analysis. Model performance was evaluated by area under the receiver operating characteristic curve (AUC) and a calibration test. Internal validation by bootstrapping re-sampling with 1000 repetitions was applied to correct for over-optimism. The clinical usefulness of the neck disability model was explored by developing a risk matrix for individual case examples.
Results
Thirty-eight percent of patients experienced non-success in neck disability and 35% in arm pain. Loss to follow-up was 35% for both groups. Predictors for non-success in neck disability were high physical demands in work, low level of education, pending litigation, previous neck surgery, long duration of arm pain, medium-to-high baseline disability score and presence of anxiety/depression. AUC was 0.78 (95% CI, 0.75, 0.82). For the arm pain model, all predictors for non-success in neck disability, except for anxiety/depression, were found to be significant in addition to foreign mother tongue, smoking and medium-to-high baseline arm pain. AUC was 0.68 (95% CI, 0.64, 0.72).
Conclusion
The neck disability model showed high discriminative performance, whereas the arm pain model was shown to be acceptable. Based upon the models, individualized risk estimates can be made and applied in shared decision-making with patients referred for surgical assessment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical degenerative radiculopathy (CDR) is caused by nerve root compression by a herniated or bulging disc and/or ligament hypertrophy and bony spurs. The incidence rate is reported to be approximately 80 per 100,000 people [32], and surgical treatment is usually offered to patients with persistent arm pain and/or paresis [10]. With the introduction of modern operative techniques like anterior cervical discectomy and fusion or disc arthroplasty, treatment safety and effectiveness have increased dramatically [10]. Currently, day surgery is practiced in many clinics worldwide [14, 20]. Still, far from all patients improve after surgery [5,6,7, 12]. Many studies have investigated what predicts a beneficial outcome [21, 31], but there is current lack of evidence concerning factors associated with unfavourable or non-successful outcomes. A high body mass index [47], mental health problems [1, 19] and lower social class [15] are individual patient characteristics that have been linked to poor treatment outcomes after cervical degenerative surgery. Predictive models can aid in calibrating surgeons’ and patients’ expectations prior to intervention, thus enhancing clinical decision-making and patient selection for surgical intervention.
The primary objective of this study was to develop and validate a prediction model for non-success in neck disability 12 months after surgery for CDR. Secondary objectives were to provide the same analysis for arm pain and to develop a risk matrix for the primary outcome to exemplify the use of the model in a clinical setting.
Methods
Design and ethics
This is a multicentre longitudinal study following the recommendations for reporting in observational studies, STROBE criteria [44] and the methodological framework proposed by the PROGRESS framework [33, 40]. The manuscript is reported according to the Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD) guidelines [9]. We used the Prediction model Risk Of Bias Assessment Tool (PROBAST) to minimize the risk of bias [27, 45]
Our research protocol was approved by the Norwegian Committee for Medical and Health Research Ethics Midt (2014/344). Written informed consent was obtained from all patients.
Patients and surgical treatment
Data from the Norwegian Registry for Spine Surgery (NORspine) from 2011 to 2016 was used. NORspine is a government-funded comprehensive clinical registry receiving no industry funding and used for quality assessment and research. Informed consent is obtained from all patients before they enter the registry. Currently, all centres performing cervical spine surgery in Norway report data to NORspine (coverage = 100%), and the operation recording rate is 78% (completeness) [3]. Patients who had undergone anterior cervical discectomy and fusion or arthroplasty surgery due to cervical degenerative radiculopathy in the period were included. For both groups, baseline characteristics and 12-month outcome data were similar, except from baseline Neck Disability Index and neck pain scores, which were slightly higher in the arthroplasty group (p = 0.02 and p = 0.002, respectively). Also, arthroplasty patients were operated in significantly lower number of levels (p < 0.001). Patients undergoing posterior cervical procedures due to CDR, as well as all patients operated for myelopathy symptoms, were excluded. Patients operated for tumours, fractures and primary infections are not included in NORspine.
Patients completed data at admission for surgery (baseline), after 3 and 12 months. Surgeon’s forms containing information about diagnosis, treatment and comorbidity were completed during the hospital stay. Only cohort participants responding to the 12-month questionnaire were included in the present study. Follow-up was conducted by the central registry unit without involvement of the treating hospital. The patients responded by questionnaires sent and returned by mail. One reminder with a new form was sent to non-respondents within 2 weeks.
Outcome definitions
For the primary outcome, the Neck Disability Index (NDI) (0–100), non-success was defined as an absolute score of > 26 at 12-month follow-up. For the secondary outcome, arm pain intensity assessed by numerical rating scale (NRS-AP) (0–10), non-success was defined as a score ≥ 3 at 12-month follow-up. These estimates are based on a previous study for patients undergoing CDR surgery in Norway [25].
Candidate predictors
Candidate predictors for non-success were selected from the comprehensive NORspine questionnaire administered before surgery, which consists of information about sociodemographic factors, lifestyle, work and clinical variables in addition to patient-reported outcome measures (PROMs). Data from the surgeons’ forms were used for information about diagnosis, treatment, comorbidity, the American Society of Anaesthesiologists physical status (ASA), surgical indication and type of operation. The selection of the final set of predictors was made after a thorough literature review where we identified the factors that have been found to be significantly and consistently associated with outcomes after CDR surgery.
The following predictors were selected for the model: gender, age groups (below 40 years, between 40 and 60 years or above 60 years), work status prior to operation (on sick leave, retired or disabled; on rehabilitation, out of work or on work return training; student, fully working or housewife/househusband), physical demands in work (working with computers, sitting, light physical work or hard physical work), educational level (high school or less, less than 4 years university or 4 or more years of university), mother tongue (Norwegian or non-native speaker), pending litigation (yes/no) (pending litigation defined as unresolved claims or litigation issues against the Norwegian Public Welfare Agency Fund concerning permanent disability pension or compensation claims against private insurance companies or the public Norwegian System of Compensation to Patients), duration of arm pain (less than 3 months, 3 to 12 months or more than 12 months), duration of pre-operative paresis (no paresis, less than 3 months or more than 3 months), body mass index (BMI) (equal to or below 30 or above 30), smoking (yes/no), comorbidities (yes/no), previous neck surgery (yes/no), number of surgical levels (one or more than one), daily use of analgetic drugs (yes/no), ASA level (level 1–2 or level 3–4), arm pain neck pain ratio (above 1 or below or equal to 1) [30] and anxiety/depression by the item on the EuroQol-5D-3L (EQ-5D) questionnaire (“moderate” to “extremely” anxious or depressed or “not anxious or depressed”). In addition, baseline outcome scores were included as potential predictors; the baseline scores were categorized into low, medium and high by percentile distribution.
Sample size considerations
Since no consensus on sample size in prognostic modelling exists, we chose to follow the recommendations by Steyerberg [38]: (a) aiming for at least 100 events as a minimum for reliable estimation of the average risk and (b) aiming for at least 10 events per variable (EPV) and preferably 20, for reliable prediction modelling if the event rate is < 20% and higher EPV values if the event rate is between 20 and 80%. In the present material, approximately 700 cases had non-success at 12-month follow-up, and with this large number of EPV, we had nearly 40 cases per event and good statistical power for the prediction model analyses. The large EPV will reduce the potential for overfitting and optimism of the final models. Overfitting is defined as fitting a statistical model with too many effective degrees of freedom in the modelling process. Estimation bias is defined as the overestimation of effects of predictors because selection of the effects withstood a statistical test, whereas optimism is defined as the difference between true performance (performance in the underlying population, e.g. external validation sample) and apparent performance (development sample) [38].
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics version 26 for Windows and the STATA version 16 for Windows. Missing data was checked for all variables and are reported together with descriptive data. Frequencies were used for categorical data and mean and standard deviation (SD) for continuous data. Continuous variables, such as baseline disability, were categorized to be adapted into a risk matrix. The distribution of baseline and 12-month scores of the two outcome measures are presented by mean scores and SD.
First, a univariable analysis of the candidate predictors was performed to assess the crude association between each candidate predictors and the two outcomes. Associations between outcomes and predictors are expressed as odd ratios (OR) with a 95% confidence interval (CI). Predictors reaching p < 0.1 in these analyses were entered into two multivariable logistic regression models (for primary and secondary outcome), where a stepwise backward elimination method was used. Variables that were not statistically significant (p > 0.05) in the multivariable models were removed from the model. The performance of the two final models was evaluated with (1) the explained variance by Nagelkerke’s R2, (2) the Hosmer–Lemeshow test p > 0.05) and (3) the discriminative ability of the model (the likelihood that the model allocates higher predicted risks to patients who achieve non-substantial improvement and lower predicted risks to those who do not) assessed by calculating the area under the receiver operating curves (AUC), also often referred to as the c-index [41]. The larger the AUC, the greater is the discriminative ability of the model. The discriminative performance of the models was considered acceptable if the AUC was ≥ 0.7 and good if the AUC was ≥ 0.8 (the c-criterion).
Internal validation was conducted by a bootstrap procedure (1000 samples) to estimate the amount of optimism in the two final models [26, 39]. A slope value was calculated (the closer to 1.0, the less over-optimism) and used to correct and shrink the regression coefficients, the R2 and the c-index.
Clinical usefulness (risk matrix)
We assessed the potential clinical utility of the final prediction model for non-success in neck disability by developing a risk matrix for two hypothetical patient case profiles with few and many predictors present. Regression coefficients from the final disability model were converted into probabilities, and a risk score for each of the two individual case profiles was calculated by the sum of the products of individual values of each predictor variable and its regression coefficient. Depending on the presence or absence of the risk factors, the matrix was then calculated as probability for a non-substantial improvement after 12 months for each of the patients.
Results
There were 3142 patients who had undergone either anterior discectomy and fusion (3109) or arthroplasty (33) due to CDR during the study period. Out of these, 2022 (64.4%) completed 12-month follow-up and were included in the analyses (2020 for the NDI analysis and 1980 for the NRS-AP analysis). Compared to responders at 12-month follow-up, non-responders were less likely to be female, significantly younger, had higher neck disability, more neck pain, lower quality of life, were less educated and more likely to be smoking.
Demographic and clinical characteristics at baseline for the included participants are summarized in Table 1, including the missing values for each variable. Gender distribution was equal (50%), and the average age at baseline was 51 years. Most patients were on sick leave before surgery. Approximately 40% of the patients reported that their job involved hard physical work, and only 17% had high level of education. Nearly half of the patients had experienced neck pain for more than 1 year. Only 5% of the patients had an ASA level of 3 or more prior to surgery. There were few missing values for the candidate predictor variables, except for physical demands in work, pending litigation, duration of pre-operative paresis, previous neck surgery and arm/neck pain ratio (Table 1).
The mean scores of the NDI and NRS arm pain at 12-month follow-up was 23.4 (SD 18.8) and 2.9 (SD 2.8), respectively. A total of 38.0% had non-successful outcomes in neck disability and 35.3% in arm pain.
Table 2 presents the univariable analysis of all candidate predictors. Most candidate predictors showed a statistical univariate relationship to the two outcomes: female gender, being retired or receiving disability or rehabilitation pension, high physical demands in work, low education level, being a non-native speaker, having a pending litigation, smoking, presence of comorbidity, having undergone previous neck surgery, having long duration of arm pain or long duration of paresis prior to surgery, high ASA level, daily use of analgetic drugs, arm pain worse than neck pain, presence of anxiety/depression or high baseline scores of NDI or arm pain. Age, obesity and number of surgical levels were not significantly associated to any of the two outcomes.
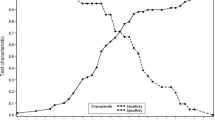
Table 3 shows the results from the multivariable analyses. Seven predictors (hard physical demands in work, low level of education, pending litigation, previous neck surgery, duration of arm pain > 3 months, medium or high levels of baseline disability and anxiety/depression) showed statistically significant association with non-success in neck disability. The model displayed good overall performance with Nagelkerke R2 of 28.3%, non-significant Hosmer–Lemeshow test and AUC 0.78 (95% CI 0.75, 0.82). The prediction model for non-success in arm pain included six of the same predictors (hard physical demands in work, low level of education, pending litigation, previous neck surgery, duration of arm pain > 3 months, medium or high levels of baseline disability) in addition to foreign mother tongue, smoking and medium or high levels of arm pain. This model showed acceptable performance with Nagelkerke R2 of 15.5% and AUC of 0.68 (95% CI 0.64, 0.72). The calibration plots for the two models are displayed in Figs. 1 and 2. Both models had high calibration slopes of 1.0, indicating no overfitting of the models.
Two risk matrices were developed for cases with low and high risk for non-success in neck disability, respectively. “Low-risk” was defined as having three out of the eleven risk factors in the prognostic model, while “high-risk” was defined as having six out of the eleven factors. The matrices are displayed in Table 4 and show that a low-risk individual the risk for non-success was 13%, whereas for a high-risk individual, the risk for non-success was 92%.
Discussion
In this study, we found that more than one third of the patients reported non-successful outcome in neck disability or arm pain at 12-month follow-up after surgery for cervical degenerative radiculopathy. Patients with high risk for non-success in neck disability were characterized by physical demanding work, low level of education, pending litigation, previous neck surgery, duration of arm pain > 3 months and medium-to-high levels of baseline disability as well as anxiety/depression. The predictors for non-success in arm pain were foreign mother tongue, smoking, medium-to-high levels of baseline arm pain and all neck disability model predictors except for anxiety/depression.
The discriminative performance of the neck disability model was found to be good with an AUC of 0.78, whereas the arm pain model was slightly less accurate but still acceptable (0.68). A recent study on patients undergoing elective cervical spine surgery by Archer et al. reports slightly lower AUCs for a predictive model of worse NDI scores (0.64–0.69) and of worse arm pain scores (0.63–0.65) 1 year after intervention [2]. There is a large overlap of significant predictors between our two studies. For example, Archer et al. found that worsening of NDI and arm pain scores were significantly associated with longer symptom duration, workers’ compensation claims and higher baseline NDI — all of which are included in our two present models. In accordance with our results, Archer et al. found depression only to be significantly associated with worse NDI scores. Several other studies have shown a negative impact of mental health on outcomes after surgery for CDR [1, 11, 19, 23]. Further, Archer et al. found no association between worsening of scores and smoking or pre-operative pain level. In the present study, both factors were significantly associated with non-success in arm pain.
There exists conflicting evidence regarding gender and its impact on PROMs and other outcomes, such as length of hospital stay and complication rates after degenerative neck surgery [4, 18, 34]. Archer et al. found that female sex was among the predictors for worse neck disability scores but not for worse arm pain scores. In another multivariate analysis, Scerrati et al. found that female sex and two-level surgery (vs. one-level surgery) correlated with worse outcomes in NDI, as well as the use of postoperative collars, while BMI only was shown to be significant in an univariate analysis [34]. In the present model, neither gender, number of surgical levels nor obesity did show significant association with non-success in neck disability or arm pain. There are also conflicting results in literature regarding the impact of obesity on neck disability. For example, similar to our results, Sielatycki et al. found no correlation between a high BMI and cut-offs for several PROMs, including NDI [35], whereas Zhang et al. found that high BMI was associated with longer hospital stay, duration of surgery and higher postoperative complication rates [47].
The present study could not find that high age was a predictor of non-success in neither neck disability nor arm pain. This is supported by other multivariate studies [2, 29, 34]. Further, both comorbidity and ASA level only came out as significant predictors for non-success in the present univariate analyses but not in the final multivariate analysis. In a study of risk factors for failure to achieve a minimal clinically important difference (MCID) in NDI 12 months after surgery for cervical radiculopathy, a higher burden of comorbidity was found to be the most significant predictor [29]. Other studies have emphasized the significance of age and pre-operative functional status as a predictor of complications and mortality after cervical degenerative surgery [24, 28]. Since changing demographics are likely to significantly increase the age and frailty of those who seek operative care for cervical degenerative disease in the coming years, further research is warranted in relation to these aspects.
Impact of findings
In the current healthcare environment, value-based thinking has brought more focus on quality and appropriateness of care. Also, as degenerative neck surgery is becoming increasingly safe and efficient, there is a need for more knowledge about which patients are not improving from surgery. The two present models can be used in a clinical setting to predict which patients will benefit from a surgical intervention and who will be better off being treated conservatively. To exemplify how these models can be used in a surgical practice, we produced a risk matrix constituted of two hypothetical patient scenarios for disability; one where the patient had several of the risk factors and another where the patient had only a few risk factors (Table 4). The patients with few predictors had low probability for non-success (0.13), while several predictors involved a high risk for non-success (0.92). According to our model, a patient with similar characteristics and symptomatology as described in the case study with few predictors should be reassured that surgery is a safe option in terms of improving from baseline arm pain and disability. Patients with a similar clinical picture as patient 2 with several positive predictors, on the other hand, should be counselled about alternative treatment strategies.
The present models can be further developed into a risk calculator to assess the probability of success or failure to achieve substantial change for every patient in a surgical practice. However, the model will first need to be further validated in other study populations. The feasibility of a risk calculator should also be evaluated.
Strengths and limitations
An advantage of the present study is the large sample size of data captured in a national registry. NORspine was designed to prospectively capture important candidate predictors and PROMs prior to and during the year following surgery. The registry covers all the hospitals and private clinics conducting surgery on spinal disorders in Norway. A total of 78% of the operations are recorded in the registry [36]. Furthermore, our two models were well balanced with respect to the risk of overfitting, in particular the disability model which showed high accuracy with only seven included predictors.
In our study, we chose to include patients operated with both arthroplasty and fusion. The baseline characteristics and 12-month outcome data were similar between the groups, except for slightly higher NDI and NRS-NP scores for the arthroplasty patients at baseline, as well as a lower number of operated levels. There is no current consensus about the use of arthroplasty vs fusion in patients with degenerative cervical disease [8, 13, 16, 17, 42, 46]. One may question whether the results of the fusion group in our study can be generalized to the arthroplasty group since there are only 1% of arthroplasty patients in our cohort. Further studies are warranted to elucidate this issue.
Loss to follow-up was 35.6% at 12-month follow-up and could represent a selection bias. However, two recent Scandinavian spine registry studies based on similar cohorts have found that a loss to follow-up did not bias conclusions about treatment effects [22, 37].
Another potential limitation is related to the cut-off estimates of the applied PROMs. In the present study, we decided to use estimates of non-success instead of the concept of MCID. The main reason is that MCID often show to be less than measurement errors or estimates for smallest detectable change [43], making it difficult for a patient and/or a clinician to judge the clinical meaningfulness of these estimates. By using stricter estimates reflecting a substantial rather than minimal change, we argue that these cut-offs are better suited for use in the development of prediction models for non-success (or success).
The major limitation of the present study is that we did not externally validate the final models. External validation is necessary before these models can be further developed into a risk calculator used in clinical settings. Risk calculators may help inform discussions of surgical treatment options between surgeons and patients and lead to more accurate judgement of operative risk. In a clinical decision-making process, the probability of successful or non-successful outcomes of conservative treatment strategies also needs to be taken into consideration. The present study only investigated outcomes after surgical treatment and cannot be generalized to outcomes after non-surgical treatment options. Thus, there is a large need for exploring prediction models for both surgical and non-surgical treatment trajectories and outcomes.
Conclusions
The final prediction model for non-successful outcome in neck disability 12 months after CDR surgery showed high discriminative performance, whereas the prediction model for arm pain was slightly less predictive. Based upon the two prediction models, individualized risk estimates can be made and used in shared decision-making with patients referred for surgical assessment. The models need to be externally validated and further tested in a clinical setting.
Change history
25 March 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00701-024-06045-7
References
Alvin MD, Miller JA, Lubelski D, Nowacki AS, Scheman J, Mathews M, McGirt MJ, Benzel EC, Mroz TE (2016) The impact of preoperative depression and health state on quality-of-life outcomes after anterior cervical diskectomy and fusion. Global Spine J 6:306–313. https://doi.org/10.1055/s-0035-1562932
Archer KR, Bydon M, Khan I, Nian H, Pennings JS, Harrell FE Jr, Sivaganesan A, Chotai S, McGirt MJ, Foley KT, Glassman SD, Mummaneni PV, Bisson EF, Knightly JJ, Shaffrey CI, Asher AL, DEVIN CJ (2020) Development and validation of cervical prediction models for patient-reported outcomes at 1 year after cervical spine surgery for radiculopathy and myelopathy. Spine (Phila Pa 1976) 45:1541–1552. https://doi.org/10.1097/brs.0000000000003610
Austevoll IM, Gjestad R, Brox JI, Solberg TK, Storheim K, Rekeland F, Hermansen E, Indrekvam K, Hellum C (2017) The effectiveness of decompression alone compared with additional fusion for lumbar spinal stenosis with degenerative spondylolisthesis: a pragmatic comparative non-inferiority observational study from the Norwegian Registry for Spine Surgery. Eur Spine J 26:404–413. https://doi.org/10.1007/s00586-016-4683-1
Basques BA, Hijji FY, Khechen B, Haws BE, Mayo BC, Massel DH, Louie PK, Cardinal KL, Guntin JA, Singh K (2018) Sex differences for anterior cervical fusion: complications and length of stay. Spine (Phila Pa 1976) 43:1025–1030. https://doi.org/10.1097/brs.0000000000002512
Bertalanffy H, Eggert HR (1988) Clinical long-term results of anterior discectomy without fusion for treatment of cervical radiculopathy and myelopathy. A follow-up of 164 cases. Acta Neurochir (Wien) 90:127–135. https://doi.org/10.1007/bf01560567
Burkus JK, Traynelis VC, Haid RW Jr, Mummaneni PV (2014) Clinical and radiographic analysis of an artificial cervical disc: 7-year follow-up from the Prestige prospective randomized controlled clinical trial: Clinical article. J Neurosurg Spine 21:516–528. https://doi.org/10.3171/2014.6.Spine13996
Buttermann GR (2018) Anterior cervical discectomy and fusion outcomes over 10 years: a prospective study. Spine (Phila Pa 1976) 43:207–214. https://doi.org/10.1097/brs.0000000000002273
Byvaltsev VA, Stepanov IA, Riew DK (2020) Mid-term to long-term outcomes after total cervical disk arthroplasty compared with anterior diskectomy and fusion: a systematic review and meta-analysis of randomized controlled trials. Clin Spine Surg 33:192–200. https://doi.org/10.1097/bsd.0000000000000929
Collins GS, Reitsma JB, Altman DG, Moons KG (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD). Ann Intern Med 162:735–736. https://doi.org/10.7326/l15-5093-2
Dakwar E, Deukmedjian A, Ritter Y, Dain Allred C, Rechtine GR (2016) Chapter 16 - Spinal pathology, conditions, and deformities: surgical intervention. In: Magee DJ, Zachazewski JE, Quillen WS, Manske RC (eds) Pathology and intervention in musculoskeletal rehabilitation (second edition). Elsevier, Maryland Heights, MO, pp 584–611. https://doi.org/10.1016/B978-0-323-31072-7.00016-6
Diebo BG, Lavian JD, Liu S, Shah NV, Murray DP, Beyer GA, Segreto FA, Maffucci F, Poorman GW, Cherkalin D, Torre B, Vasquez-Montes D, Yoshihara H, Cukor D, Naziri Q, Passias PG, Paulino CB (2018) The impact of comorbid mental health disorders on complications following cervical spine surgery with minimum 2-year surveillance. Spine (Phila Pa 1976) 43:1455–1462. https://doi.org/10.1097/brs.0000000000002651
Engquist M, Löfgren H, Öberg B, Holtz A, Peolsson A, Söderlund A, Vavruch L, Lind B (2013) Surgery versus nonsurgical treatment of cervical radiculopathy: a prospective, randomized study comparing surgery plus physiotherapy with physiotherapy alone with a 2-year follow-up. Spine (Phila Pa 1976) 38:1715–1722. https://doi.org/10.1097/BRS.0b013e31829ff095
Gao X, Yang Y, Liu H, Meng Y, Zeng J, Wu T, Hong Y (2018) A comparison of cervical disc arthroplasty and anterior cervical discectomy and fusion in patients with two-level cervical degenerative disc disease: 5-year follow-up results. World Neurosurg. https://doi.org/10.1016/j.wneu.2018.10.231
Gennari A, Mazas S, Coudert P, Gille O, Vital JM (2018) Outpatient anterior cervical discectomy: a French study and literature review. Orthop Traumatol Surg Res 104:581–584. https://doi.org/10.1016/j.otsr.2018.04.014
Godlewski B, Stachura MK, Twardowska-Staszek E, Czepko RA, Czepko R (2018) Effect of social factors on surgical outcomes in cervical disc disease. Anesth Pain Med 8:e84140. https://doi.org/10.5812/aapm.84140
Goldstein ZH, Boody B, Sasso R (2020) Two-level anterior cervical discectomy and fusion versus cervical disc arthroplasty-long-term evidence update. Int J Spine Surg 14:36–40. https://doi.org/10.14444/7089
Gornet MF, Lanman TH, Burkus JK, Dryer RF, McConnell JR, Hodges SD, Schranck FW (2019) Two-level cervical disc arthroplasty versus anterior cervical discectomy and fusion: 10-year outcomes of a prospective, randomized investigational device exemption clinical trial. J Neurosurg Spine 21:1–11. https://doi.org/10.3171/2019.4.SPINE19157
Gruskay JA, Fu M, Basques BA, Bohl DD, Buerba RA, Webb ML, Grauer JN (2016) Factors affecting length of stay and complications after elective anterior cervical discectomy and fusion: a study of 2164 patients from the American College of Surgeons National Surgical Quality Improvement Project Database (ACS NSQIP). Clin Spine Surg 29:E34-42. https://doi.org/10.1097/bsd.0000000000000080
He J, Xiong W, Li F, Luo W, Gao SC (2017) Depression influences pain and function after cervical disc arthroplasty. J Neurosurg Sci 61:39–45. https://doi.org/10.23736/s0390-5616.16.03032-0
Helseth Ø, Lied B, Heskestad B, Ekseth K, Helseth E (2019) Retrospective single-centre series of 1300 consecutive cases of outpatient cervical spine surgery: complications, hospital readmissions, and reoperations. Br J Neurosurg 33:613–619. https://doi.org/10.1080/02688697.2019.1675587
Hermansen A, Hedlund R, Vavruch L, Peolsson A (2013) Positive predictive factors and subgroup analysis of clinically relevant improvement after anterior cervical decompression and fusion for cervical disc disease: a 10- to 13-year follow-up of a prospective randomized study: clinical article. J Neurosurg Spine 19:403–411. https://doi.org/10.3171/2013.7.Spine12843
Hojmark K, Stottrup C, Carreon L, Andersen MO (2016) Patient-reported outcome measures unbiased by loss of follow-up. Single-center study based on DaneSpine, the Danish spine surgery registry. Eur Spine J 25:282–286. https://doi.org/10.1007/s00586-015-4127-3
McNeely EL, Sachdev R, Rahman R, Zhang B, Skolasky RL (2021) Associations of depression and sociodemographic characteristics with patient activation among those presenting for spine surgery. J Orthop 26:8–13. https://doi.org/10.1016/j.jor.2021.06.001
Minhas SV, Mazmudar AS, Patel AA (2017) Pre-operative functional status as a predictor of morbidity and mortality after elective cervical spine surgery. Bone Joint J 99-b:824–828. https://doi.org/10.1302/0301-620x.99b6.Bjj-2016-1149.R1
Mjåset C, Zwart J-A, Goedmakers CMW, Smith TR, Solberg TK, Grotle M (2020) Criteria for success after surgery for cervical radiculopathy; estimates for a substantial amount of improvement in core outcome measures. Spine J 20:1413–1421. https://doi.org/10.1016/j.spinee.2020.05.549
Moons KG, Altman DG, Reitsma JB, Ioannidis JP, Macaskill P, Steyerberg EW, Vickers AJ, Ransohoff DF, Collins GS (2015) Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): explanation and elaboration. Ann Intern Med 162:1–73. https://doi.org/10.7326/m14-0698
Moons KGM, Wolff RF, Riley RD, Whiting PF, Westwood M, Collins GS, Reitsma JB, Kleijnen J, Mallett S (2019) PROBAST: a tool to assess risk of bias and applicability of prediction model studies: explanation and elaboration. Ann Intern Med 170:1–33. https://doi.org/10.7326/m18-1377
Narain AS, Hijji FY, Haws BE, Khechen B, Kudaravalli KT, Yom KH, Singh K (2020) Risk factors for medical and surgical complications after 1-2- level anterior cervical discectomy and fusion procedures. Int J Spine Surg 14:286–293. https://doi.org/10.14444/7038
Narain AS, Hijji FY, Khechen B, Haws BE, Patel DV, Bohl DD, Yom KH, Kudaravalli KT, Singh K (2019) Risk factors associated with failure to reach minimal clinically important difference in patient-reported outcomes following anterior cervical discectomy and fusion. Int J Spine Surg 13:262–269. https://doi.org/10.14444/6035
Passias PG, Hasan S, Radcliff K, Isaacs R, Bianco K, Jalai CM, Poorman GW, Worley NJ, Horn SR, Boniello A, Zhou PL, Arnold PM, Hsieh P, Vaccaro AR, Gerling MC (2018) Arm pain versus neck pain: a novel ratio as a predictor of post-operative clinical outcomes in cervical radiculopathy patients. Int J Spine Surg 12:629–637. https://doi.org/10.14444/5078
Peolsson A, Vavruch L, Oberg B (2006) Predictive factors for arm pain, neck pain, neck specific disability and health after anterior cervical decompression and fusion. Acta Neurochir 148:167–173. https://doi.org/10.1007/s00701-005-0660-x
Radhakrishnan K, Litchy WJ, O'Fallon WM, Kurland LT (1994) Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 117:325–335. https://doi.org/10.1093/brain/117.2.325
Riley RD, Hayden JA, Steyerberg EW, Moons KGM, Abrams K, Kyzas PA, Malats N, Briggs A, Schroter S, Altman DG, Hemingway H, Group P (2013) Prognosis research strategy (PROGRESS) 2: prognostic factor research. PLoS Med 10:e1001380–e1001380. https://doi.org/10.1371/journal.pmed.1001380
Scerrati A, Germano A, Montano N, Visani J, Cacciola F, Raffa G, Ghetti I, Pignotti F, Cavallo MA, Olivi A, de Bonis P (2021) Factors affecting functional outcome after anterior cervical discectomy and fusion: a multicenter study. J Craniovertebr Junction Spine 12:144–148. https://doi.org/10.4103/jcvjs.jcvjs_1_21
Sielatycki JA, Chotai S, Kay H, Stonko D, McGirt M, Devin CJ (2016) Does obesity correlate with worse patient-reported outcomes following elective anterior cervical discectomy and fusion? Neurosurgery 79:69–74. https://doi.org/10.1227/neu.0000000000001252
Solberg T, Olsen L, Berglund M (2019) Nasjonalt kvalitetsregister for ryggkirugi (NKR). Årsrapport for 2018 med plan for forbedringstiltak https://unn.no/Documents/Kvalitetsregistre/Nasjonalt%20kvalitetsregister%20for%20ryggkirurgi/Årsrapporter/Årsrapport_NKR_2018%20.pdf. Accessed 5 May 2021
Solberg TK, Sorlie A, Sjaavik K, Nygaard OP, Ingebrigtsen T (2011) Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop 82:56–63. https://doi.org/10.3109/17453674.2010.548024
Steyerberg E (2009) Clinical prediction models: a practical approach to development, validation, and updating. Spinger-Verlag New York, New York, NY, Statistics for Biology and Health. https://doi.org/10.1007/978-0-387-77244-8
Steyerberg EW, Harrell FE Jr (2016) Prediction models need appropriate internal, internal-external, and external validation. J Clin Epidemiol 69:245–247. https://doi.org/10.1016/j.jclinepi.2015.04.005
Steyerberg EW, Moons KGM, van der Windt DA, Hayden JA, Perel P, Schroter S, Riley RD, Hemingway H, Altman DG, Group P (2013) Prognosis research strategy (PROGRESS) 3: prognostic model research. PLoS Med 10:e1001381–e1001381. https://doi.org/10.1371/journal.pmed.1001381
Steyerberg EW, Vergouwe Y (2014) Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J 35:1925–1931. https://doi.org/10.1093/eurheartj/ehu207
Sundseth J, Fredriksli OA, Kolstad F, Johnsen LG, Pripp AH, Andresen H, Myrseth E, Muller K, Nygaard OP, Zwart JA (2017) The Norwegian Cervical Arthroplasty Trial (NORCAT): 2-year clinical outcome after single-level cervical arthroplasty versus fusion-a prospective, single-blinded, randomized, controlled multicenter study. Eur Spine J 26:1225–1235. https://doi.org/10.1007/s00586-016-4922-5
Terwee CB, Roorda LD, Knol DL, De Boer MR, De Vet HC (2009) Linking measurement error to minimal important change of patient-reported outcomes. J Clin Epidemiol 62:1062–1067. https://doi.org/10.1016/j.jclinepi.2008.10.011
Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M (2007) Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 4:e297. https://doi.org/10.1371/journal.pmed.0040297
Wolff RF, Moons KGM, Riley RD, Whiting PF, Westwood M, Collins GS, Reitsma JB, Kleijnen J, Mallett S (2019) PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann Intern Med 170:51–58. https://doi.org/10.7326/m18-1376
Xie L, Liu M, Ding F, Li P, Ma D (2016) Cervical disc arthroplasty (CDA) versus anterior cervical discectomy and fusion (ACDF) in symptomatic cervical degenerative disc diseases (CDDDs): an updated meta-analysis of prospective randomized controlled trials (RCTs). Springerplus 5:1188. https://doi.org/10.1186/s40064-016-2851-8
Zhang GA, Zhang WP, Chen YC, Hou Y, Qu W, Ding LX (2020) Impact of elevated body mass index on surgical outcomes for patients undergoing cervical fusion procedures: a systematic review and meta-analysis. Orthop Surg 12:3–15. https://doi.org/10.1111/os.12572
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine degenerative.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mjåset, C., Solberg, T.K., Zwart, JA. et al. Anterior surgical treatment for cervical degenerative radiculopathy: a prediction model for non-success. Acta Neurochir 165, 145–157 (2023). https://doi.org/10.1007/s00701-022-05440-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05440-2