Abstract
Background
Over the past two decades, the management of hydrocephalus has witnessed the addition of endoscopic third ventriculostomy with or without choroid plexus cauterization (ETV ± CPC) to the traditional methods including ventriculoperitoneal shunt insertion (VPSI). We conducted this study to assess mortality and complications with surgical implications associated with the two procedures in children with hydrocephalus.
Methods
We reviewed our operating theater registry to identify children below 17 years old who underwent hydrocephalus surgery for the first time in 2016. The patients were followed for up to 1 year from the date of the initial operation. Their vital status was confirmed by follow-up visits by a community nurse. Descriptive analyses were used to describe the characteristics of the patients and evaluate the study outcomes (i.e., mortality and complications).
Results
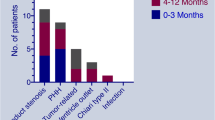
One hundred fifty-three patients were eligible for the study; 56% were males and 73.2% had primary ETV ± CPC. Complete 1-year follow-up data was available for 79 patients, and 73.4% of these had ETV ± CPC. One-year success (event-free) rates for ETV and VPSI were similar at 67.4% and 66.7%, respectively. ETVs in infants under 6 months performed poorly; failing in half the infants, who were subsequently converted to VPS. Shunt sepsis was very high, 21.4% (95% CI 10.3–36.8). The majority of surgical complications (81.8%) occurred within 3 months of surgery.
Conclusion
ETV ± CPC and VPSI carry a similar frequency of mortality and complications in our setting, and therefore, both should be considered as a treatment option for patients with hydrocephalus. As VP shunt is still used for managing most of the patients, there is still a need to prioritize measures to reduce shunt infections.
Similar content being viewed by others
Abbreviations
- CPC:
-
Choroid plexus cauterization
- CSF:
-
Cerebrospinal fluid
- EVD:
-
External ventricular drain
- ETV:
-
Endoscopic third ventriculostomy
- IQR:
-
Inter-quartile range
- VPSI:
-
Ventriculoperitoneal shunt insertion
References
Aschoff A, Kremer P, Hashemi B (1999) The scientific history of hydrocephalus and its treatment. Neurosurg Rev 22:67–933
Burton A (2017) Training non-physicians as neurosurgeons in sub-Saharan Africa. Lancet Neurol 16(9):684–685
Dewan MC, Rattani A, Mekary R, Glancz LJ, Yunusa I, Baticulon RE et al (2018) Global hydrocephalus epidemiology and incidence: systematic review and meta-analysis. J Neurosurg 130(4):1065–1079
Forte D, Peraio S, Huttunen TJ, James G, Thompson D, Aquilina K (2021) Ventriculo-atrial and ventriculo-pleural shunts as second-line surgical treatment have equivalent revision, infection, and survival rates in paediatric hydrocephalus. Childs Nerv Syst 37(2):481–489
Fritsch MJ, Kienke S, Ankermann T, Padoin M, Mehdorn HM (2005) Endoscopic third ventriculostomy in infants. J Neurosurg Pediatr 103(1):50–53
Gilard V, Chadie A, Ferracci FX, Brasseur-Daudruy M, Proust F, Marret S et al (2018) Post hemorrhagic hydrocephalus and neurodevelopmental outcomes in a context of neonatal intraventricular hemorrhage: an institutional experience in 122 preterm children. BMC Pediatr 18(1):1–8
Hagerty V, Galvin C, Maharaj A, Vrionis F (2022) Ventriculo-atrial shunts as an alternate therapy in patients with normal pressure hydrocephalus refractory to ventriculoperitoneal shunts: a case series. Interdiscip Neurosurg 27:101433. https://doi.org/10.1016/j.inat.2021.101433
He Z, An C, Zhang X, He X, Li Q (2015) The efficacy analysis of endoscopic third ventriculostomy in infantile hydrocephalus. J Korean Neurosurg Soc 57(2):119
Idowu O, Olumide A (2011) Etiology and cranial CT scan profile of nontumoral hydrocephalus in a tertiary black African hospital. Neurosurg Pediatr 7:397–400. https://doi.org/10.3171/2011.1.PEDS10481
Jallo GI, Kothbauer KF, Abbott IR (2005) Endoscopic third ventriculostomy. Neurosurgery. Focus 19(6):E11
Javadpour M, Mallucci C, Brodbelt A, Golash A, May P (2001) The impact of endoscopic third ventriculostomy on the management of newly diagnosed hydrocephalus in infants. Pediatr Neurosurg 35(3):131–135
Kamalo P (2013) Point of view: exit ventriculoperitoneal shunt; enter endoscopic third ventriculostomy (ETV): contemporary views on hydrocephalus and their implications on management. Malawi Med J 25(September):78–82
Khan F, Shamim MS, Rehman A, Bari ME (2013) Analysis of factors affecting ventriculoperitoneal shunt survival in pediatric patients. Childs Nerv Syst 29:791–802. https://doi.org/10.1007/s00381-012-2004-5
Koch D, Wagner W (2004) Endoscopic third ventriculostomy in infants of less than 1 year of age: which factors influence the outcome? Child’s Nerv Syst 20:405–411
Kulkarni AV, Schiff SJ, Mbabazi-Kabachelor E, Mugamba J, Ssenyonga P, Donnelly R et al (2017) Endoscopic treatment versus shunting for infant hydrocephalus in Uganda. N Engl J Med 377(25):2456–2524
Laeke T, Tirsit A, Biluts H, Murali D, Wester K (2017) Pediatric hydrocephalus in Ethiopia: treatment failures and infections: a hospital-based, retrospective study. World Neurosurg 100:30–37. https://doi.org/10.1016/j.wneu.2016.12.112
Lepard JR, Dewan MC, Chen SH, Bankole OB, Mugamba J, Ssenyonga P et al (2020) The CURE Protocol: evaluation and external validation of a new public health strategy for treating paediatric hydrocephalus in low-resource settings. BMJ Glob Health 5:e002100. https://doi.org/10.1136/bmjgh-2019-002100
Limbrick DD, Baird LC, Klimo P, Riva-Cambrin J, Flannery AM (2014) Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 4: cerebrospinal fluid shunt or endoscopic third ventriculostomy for the treatment of hydrocephalus in children. J Neurosurg: Pediatr 14(Supplement_1):30–4
Massimi L, Paternoster G, Fasano T, Rocco C (2009) On the changing epidemiology of hydrocephalus. Childs Nerv Syst 25:795–800
McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ (2003) Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis 36(7):858–862
Niu H, Wu H, Luo W, Wang K, Zhao L, Wang Y (2021) Ventriculoatrial shunt as a feasible regimen for certain patients of hydrocephalus: clinical features and surgical management. Acta Neurol Belg 121(2):403–408
Oliveras LM, Ortega JL, Leidinger A, Haji MA, Genovés MP, Belloch JP (2020) Infant hydrocephalus in sub-Saharan Africa: impact of perioperative care in the Zanzibar archipelago. Neurocirugía (English Edition) 31(5):223–30
Reid T, Grudziak J, Rodriguez-Ormaza N, Maine RG, Msiska N, Quinsey C et al (2019) Complications and 3-month outcomes of children with hydrocephalus treated with ventriculoperitoneal shunts in Malawi. J Neurosurg Pediatr 24:120–127. https://doi.org/10.3171/2019.2.peds18325
Riva-Cambrin J, Kestle JR, Holubkov R, Butler J, Kulkarni AV, Drake J et al (2016) Risk factors for shunt malfunction in pediatric hydrocephalus: a multicenter prospective cohort study. J Neurosurg Pediatr 17(4):382–390
Robertson FC, Esene IN, Kolias AG, Khan T, Rosseau G, Gormley WB et al (2020) Global perspectives on task shifting and task sharing in neurosurgery. World Neurosurg X 6:100060. https://doi.org/10.1016/j.wnsx.2019.100060
Rush J, Paľa A, Kapapa T, Mayer B, Micah-Bonongwe A, Kamalo P et al (2021) Assessing neurodevelopmental outcome in children with hydrocephalus in Malawi. A pilot study. Clin Neurol Neurosurg 212:107091. https://doi.org/10.1016/j.clineuro.2021.107091
Rutala WA, Weber DJ (2001) New disinfection and sterilization methods. Emerg Infect Dis 7(2):348–353
Salvador SF, Henriques JC, Munguambe M, Vaz RC, Barros HP (2014) Hydrocephalus in children less than 1 year of age in northern Mozambique. Surg Neurol Int 5:175
Schwartz TH, Ho B, Prestigiacomo CJ, Bruce JN, Feldstein NA, Goodman RR (1999) Ventricular volume after third ventriculostomy. J Neurosurg 91(20–25):0728572201
Sobana M, Halim D, Aviani JK, Gamayani U, Achmad TH (2021) Neurodevelopmental outcomes after ventriculoperitoneal shunt placement in children with non-infectious hydrocephalus: a meta-analysis. Childs Nerv Syst 37(4):1055–1065
Spector R, Keep RF, Snodgrass SR, Smith QR, Johanson CE (2015) A balanced view of choroid plexus structure and function: focus on adult humans. Exp Neurol 1(267):78–86
Thompson D (2005) Hydrocephalus and shunts. In: Moore AJ, Newell DW (eds) Neurosurgery Principles and Practice. Springer, London, pp p425-442
Uche EO, Onyia E, Mezue UC, Okorie E, Ozor II, Chikani MC (2013) Determinants and outcomes of ventriculoperitoneal shunt infections in Enugu. Nigeria Pediatric Neurosurg 49(2):75–80. https://doi.org/10.1159/000357384
Waluza J, Borgstein E (2005) Management of hydrocephalus using the Chabbra shunt. Malawi Med J 17:7–8. https://doi.org/10.4314/mmj.v17i1.10861
Warf B, Ondoma S, Kulkarni A, Donnelly R, Ampeire M, Akona J et al (2009) Neurocognitive outcome and ventricular volume in children with myelomeningocele treated for hydrocephalus in Uganda. J Neurosurg Pediatr 4:564–570
Warf BC (2010) Pediatric hydrocephalus in East Africa: prevalence, causes, treatments, and strategies for the future. World Neurosurg 73(4):296–300
Weil AG, Westwick H, Wang S, Alotaibi NM, Elkaim L, Ibrahim GM et al (2016) Efficacy and safety of endoscopic third ventriculostomy and choroid plexus cauterization for infantile hydrocephalus: a systematic review and meta-analysis. Childs Nerv Syst 32(11):2119–2131
Acknowledgements
We acknowledge Favour Kaunda for her assistance through the community nursing service and Linda Kalirani-Phiri for her assistance with (language) editing and proofreading.
Author information
Authors and Affiliations
Contributions
CM—research conception, literature review, data collection, data analysis, manuscript preparation, and approval of the final draft
HC—data analysis, first draft preparation and literature review, editing of further drafts, and approval of the final draft
PK—research conception, data analysis, manuscript preparation, editing of all drafts, and preparation of the final draft
The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors
Research involving human participants and/or animals
None
Informed consent
No informed consent
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on CSF Circulation
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chimaliro, S., Hara, C. & Kamalo, P. Mortality and complications 1 year after treatment of hydrocephalus with endoscopic third ventriculostomy and ventriculoperitoneal shunt in children at Queen Elizabeth Central Hospital, Malawi. Acta Neurochir 165, 61–69 (2023). https://doi.org/10.1007/s00701-022-05392-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05392-7