Abstract
Background
Entrustable professional activities (EPAs) represent an assessment framework with an increased focus on competency-based assessment. Originally developed and adopted for undergraduate medical education, concerns over resident ability to practice effectively after graduation have led to its implementation in residency training but yet not in vascular neurosurgery. Subjective assessment of resident or fellow performance can be problematic, and thus, we aim to define core EPAs for neurosurgical vascular training.
Methods
We used a nominal group technique in a multistep interaction between a team of experienced neurovascular specialists and a medical educator to identify relevant EPAs. Panel members provided feedback on the EPAs until they reached consent.
Results
The process produced seven core procedural EPAs for vascular residency and fellowship training, non-complex aneurysm surgery, complex aneurysm surgery, bypass surgery, arteriovenous malformation resection, spinal dural fistula surgery, perioperative management, and clinical decision-making.
Conclusion
These seven EPAs for vascular neurosurgical training may support and guide the neurosurgical society in the development and implementation of EPAs as an evaluation tool and incorporate entrustment decisions in their training programs.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Background
The treatment strategy for intracranial vascular pathologies has changed over the past 3 decades due to advances in endovascular and radiosurgical techniques. This transformation poses challenges to the future of microsurgery due to a significant decrease of surgical procedures. Experts nevertheless foresee a lasting role for open microsurgery in vascular neurosurgery [2, 4]. Microsurgery is of particular value in the treatment of arteriovenous malformations, complex aneurysms, and revascularization or flow replacement strategies, but there will be an equilibrium on non-ruptured aneurysms as well. This means a reduction in caseload and a shift towards more complex pathology.
Due to the growing complexity and centralization of care, a good microvascular neurosurgeon will have to function in a collaborative team of endovascular specialists and vascular neurologists in a tertiary care setting. These developments will require adaptation for vascular training since traditional training and examination methods of timed exposure and knowledge assessment cannot fully measure and guarantee the required competencies. Medical education has shifted to a competency-based system over the years, to educate and evaluate trainees more effectively and efficiently. Competencies are defined in so-called entrustable professional activities (EPAs). The Royal College of Physicians and Surgeons of Canada has defined two vascular EPAs: “Performing surgery for patients with an intracranial aneurysm” and “Performing surgery for patients with spontaneous intracerebral hemorrhage with or without an underlying vascular malformation” [5]. However, they do not include EPAs on complex vascular pathology, which presents a significant part of the surgical spectrum. The integration of the competency-based system into the traditional training would provide additional possibilities to ensure a high level of competency and skilled vascular neurosurgeons in the near future. Hence, the aim of this work is to develop a competency-based framework for general and complex vascular pathology to assist in resident and fellowship training.
Methods
Definitions
Entrustable professional activities
In order to operationalize a competency-based medical education program, curriculum development is based around EPAs. Where competencies describe the qualities of an individual person, EPAs describe the work that the professional must do [7]. EPAs require the professional to integrate multiple competencies from several domains that focus on individuals and their knowledge, skills, and attitudes.
Entrustment level scale
The entrustment level scale evaluates to what extend a trainee can be trusted to execute the EPA which is the focus of assessment. Although adjusted versions exist, a five-level entrustment scale is most commonly used [1, 7]:
-
1.
Observation but no execution, even with direct supervision
-
2.
Execution with direct, proactive supervision
-
3.
Execution with reactive supervision, i.e., on request and quickly available
-
4.
Supervision at a distance and/or post hoc
-
5.
Supervision provided by the trainee to more junior colleagues
Nominal group technique
We convened a group of cerebrovascular specialists in a six-stage approach to gain consensus on the EPAs [3]. (1) The first group consisted of two neurosurgeons (JHVL, HJS), one medical education specialist (BM), and a hybrid neurosurgeon (HB), who participated in a nominal group technique on the identification of the EPAs. (2) Each specialist was involved in direct patient care, worked with residents or fellows, and was an experienced medical educator. This was followed by a group discussion of each EPA and its competencies until agreement among the experts was reached. (3) Two authors (JHVL, HB) drafted the EPAs based on analysis of the collected data. (4) Subsequently, a cerebrovascular specialist (DH) independently reviewed the EPAs and competencies in direct communication with the corresponding author (JHVL). (5) A multidisciplinary international group of cerebrovascular specialists (panel members of the EANS vascular section) reviewed the EPAs and competencies. (6) The first group of specialists then refined and finalized the EPAs based on the feedback. The finalized EPAs were approved by all specialists.
Results
Phases 1 to 3
There were eight candidate activities that were reduced to five during the first round of discussion and eventually increased to six after revision in the final round resulted in the aneurysm surgery activity being split. We excluded the following EPAs: “professional development” because it does not entail a unit of work and therefore does not qualify as an EPA and “spinal arteriovenous malformations” due to the low incidence.
Phases 4 and 5
The multidisciplinary international group of cerebrovascular specialists (panel members of the EANS vascular section) revised all six activities. Of these activities, none required major revisions to the description, but all six required minor changes. The reviewers suggested adding a separate EPA for spinal dural fistulas. The reviewers did not discard any activities.
Phase 6 (Final review)
The first group of specialists reviewed the work of the reviewer in detail, made minor changes to all six activities, and added an EPA for spinal dural fistulas. The authors unanimously agreed to accept the seven activities as EPAs.
We have defined the following six EPAs:
-
EPA 1: Non-complex aneurysm surgery
-
EPA 2: Complex aneurysm surgery
-
EPA 3: Bypass surgery
-
EPA 4: Arteriovenous malformation resection
-
EPA 5: Spinal dural fistula
-
EPA 6: Perioperative management
-
EPA 7: Clinical decision-making
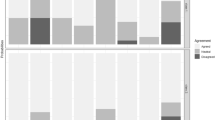
Figures 1, 2, 3, 4, 5, 6, and 7 present a detailed description of each EPA.
Discussion
We identified seven EPAs based upon their particular value in vascular microsurgery, for which we foresee a continuing role in vascular microsurgery. The present manuscript presents an attempt to add a competency-based system to traditional training in vascular neurosurgery.
Although this concept was initially developed to operationalize competency-based postgraduate medical education, it is now widely applied in health professions education [6, 8]. The Accreditation Council for Graduate Medical Education and the American Board of Surgery both have identified the need for competency-based skills assessments in surgical training, based upon a reported lack of confidence of surgical residents at the time of graduation [9]. By definition, EPAs allow for residents and fellows to achieve competence at different rates to increase surgical autonomy. This transition from traditional training and examination methods seems particular relevant for vascular microneurosurgery since technical advances in endovascular treatment modalities result in a reduction of caseload, whereas governments and patients increasingly demand metrics of competency for operative performance. EPAs present us with a possible framework for these metrics and can be added to residency and fellowship programs [9]. So far, there exists no threshold of competency metrics within the essential EPAs, but it is possible that governing bodies in the future will determine such a threshold for accredited residency and fellowship programs.
A recent study evaluated the appropriateness of the EPA “performing intracranial aneurysm surgery” for general residency and found that it was more suitable for a fellowship [8]. Since most of these activities are nowadays acquired during dedicated fellowships, these specialized EPAs are more suitable for this setting. The more general EPA’s numbers six and seven are also suitable for neurosurgery residency.
We are reasonably confident that this list of EPAs represents the core of vascular microsurgery. The EPAs proposed in the present article however are not meant to be infallible, and it is possible that other vascular specialists identify other relevant EPAs not included in this manuscript. The EPAs may also not fully reflect national or institutional priorities and may be adjusted to fit local vascular units.
These EPAs represent the core professional acts of vascular microsurgeons to provide safe and effective neurosurgical care. They thus are the activities that teachers should trust residents of vascular fellows to perform under varying degrees of supervision, and the supervision should ask whether he or she trusts the resident or fellow to perform these activities under what level of supervision. Medical educators should rate resident or fellow performance on EPAs using the before-mentioned entrustment scales. We do not aim to define training outcomes but rather focus on reaching an agreement on how to describe the stage a trainee is at for a given procedure. Continuing work would describe in more detail what a modern European cerebrovascular neurosurgeon should resemble in terms of experience. The neurosurgical society will need to determine the best methods of implementing the EPAs within vascular neurosurgery fellowship programs. [2] This study presents a foundation for the use and further development of specific EPAs for competency-based training of neurovascular microsurgical residents and fellows.
Conclusion
These EPAs aid to focus on authentic professional work of vascular neurosurgeons and will represent the basis for assessment in vascular neurosurgery training.
References
Chen HC, van den Broek WE, ten Cate O (2015) The case for use of entrustable professional activities in undergraduate medical education. Acad Med 90:431–436. https://doi.org/10.1097/ACM.0000000000000586
Haeren R, Schwartz C, Satopaa J, Lehecka M, Niemela M (2021) Letter: Training of microsurgical aneurysm clipping in the endovascular era: towards structured fellowship programs in Europe. Neurosurgery 88:E465–E466. https://doi.org/10.1093/neuros/nyab011
Kwan J, Crampton R, Mogensen LL, Weaver R, van der Vleuten CP, Hu WC (2016) Bridging the gap: a five stage approach for developing specialty-specific entrustable professional activities. BMC Med Educ 16:117. https://doi.org/10.1186/s12909-016-0637-x
Lawton MT, Lang MJ (2019) The future of open vascular neurosurgery: perspectives on cavernous malformations, AVMs, and bypasses for complex aneurysms. J Neurosurg 130:1409–1425. https://doi.org/10.3171/2019.1.JNS182156
Rabski JE, Saha A, Cusimano MD (2020) Setting standards of performance expected in neurosurgery residency: a study on entrustable professional activities in competency-based medical education. Am J Surg. https://doi.org/10.1016/j.amjsurg.2020.12.014
ten Cate O (2005) Entrustability of professional activities and competency-based training. Med Educ 39:1176–1177. https://doi.org/10.1111/j.1365-2929.2005.02341.x
Ten Cate O (2013) Nuts and bolts of entrustable professional activities. J Grad Med Educ 5:157–158. https://doi.org/10.4300/JGME-D-12-00380.1
Ten Cate O, Chen HC, Hoff RG, Peters H, Bok H, van der Schaaf M (2015) Curriculum development for the workplace using Entrustable Professional Activities (EPAs): AMEE Guide No. 99. Med Teach 37:983–1002. https://doi.org/10.3109/0142159X.2015.1060308
Wagner JP, Lewis CE, Tillou A, Agopian VG, Quach C, Donahue TR, Hines OJ (2018) Use of entrustable professional activities in the assessment of surgical resident competency. JAMA Surg 153:335–343. https://doi.org/10.1001/jamasurg.2017.4547
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery Training
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van Lieshout, J.H., Malzkorn, B., Steiger, HJ. et al. Defining activities in neurovascular microsurgery training: entrustable professional activities for vascular neurosurgery. Acta Neurochir 165, 27–37 (2023). https://doi.org/10.1007/s00701-022-05372-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05372-x