Abstract
Purpose
To study the effect of antithrombotic therapy (ATT) on the outcome of operatively treated chronic subdural hematomas (CSDH).
Methods
A retrospective population-based cohort study from Eastern Finland including all adult patients who underwent a burr-hole craniostomy (BHC) for CSDH during 2016 and 2017. The follow-up time for recurrence was 6 months and for mortality 3 years.
Results
A total of 301 CSDH patients were included in the study. ATT (antithrombotic therapy; antiplatelet or anticoagulant medication) was used by 164 patients (54.5%) at the time of diagnosis. The hematoma was bilateral in 102 patients (33.9%). Forty-seven patients (15.8%) encountered hematoma recurrence. Bilateral CSDHs required reoperations more often than unilateral hematomas (12.6% vs. 22.0%; p = 0.036) regardless of the primary operation (uni- or bilateral). A bivariate logistic regression analysis showed that bilateral hematoma (OR 1.918; 95% CI 1.013–3.630; p = 0.045) and male gender (OR 2.363; 95% CI 1.089–5.128; p = 0.030) independently predicted hematoma recurrence. The overall three-year mortality was 27.9%. The use of ATT was not associated with CSDH recurrence, and the length of the temporary postoperative ATT discontinuation did not correlate with the rate of thromboembolic events.
Conclusions
ATT did not affect CSDH recurrence in our study population, and the duration of the temporary postoperative ATT discontinuation was not associated with the rate of thromboembolic complications. Male gender and bilateral hematomas were more frequently associated with recurrences.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic subdural hematoma (CSDH) is a frequently encountered entity in the aging population. The overall incidence in adults ranges widely between 1.7 and 20.6/100,000/year [53], and in the age group of ≥ 80 years an annual incidence of up to 129.5/100,000 has been reported [40]. CSDH is defined as a pathological, slowly growing encapsuled collection of fluid in the subdural space [31]. It often originates from a preceding head trauma with a certain time interval but the trauma may be mild or even absent [6, 39]. In addition to a head trauma, age, male gender, alcohol abuse and antithrombotic therapy (ATT) with either anticoagulant or antiplatelet medications are perceived as risk factors for CSDH. [19, 31, 40] The pathophysiology of CSDH is attributed to a gradual inflammatory process induced by an initially small hematoma, which leads to fluid accumulation in the subdural space and progressive growth [16]. Surgical treatment is recommended for symptomatic CSDHs, and multiple different operative techniques have been suggested [2, 15, 25, 51]. Most operations can be performed under local anesthesia, which enables surgical treatment even for frail and comorbid patients. Among these patient groups ATT is commonly used, but the effect on the outcome of CSDH is controversial as is the risk of thromboembolic events related to temporarily discontinuing these medications. In this population-based study, we retrospectively collected all patients from Eastern Finland who underwent burr-hole craniostomy (BHC) for CSDH at Kuopio University Hospital during years 2016 and 2017. The aim was to study the effect of ATT on the outcome of operatively treated CSDHs and to identify risk factors for recurrence.
Materials and methods
Kuopio University Hospital (KUH) is responsible for providing all neurosurgical treatment for its geographically defined catchment population (813,000 in 2016) in Eastern Finland. In this population-based cohort study, we identified all patients who were operated due to CSDH at KUH during the years 2016 and 2017.
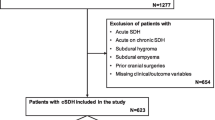
The flow chart of the study is presented in Fig. 1. The final study population consisted of 301 patients. The medical records of all patients were reviewed in detail. In addition to recording demographic and clinical data, several grading scales were reconstructed from the details provided in the patient records. Data on antithrombotic medications were gathered from patient records and national prescription registries. The etiology of the hematoma was considered non-traumatic if no evidence of preceding head trauma, fall or other traumatic event was present in the medical records. Risks for bleeding and thromboembolic events were evaluated by calculating the HAS-BLED [36] and CHA2DS2-VASc [30] scores also for patients without atrial fibrillation diagnosis. HAS-BLED ≥ 3 points indicates high bleeding risk, and CHA2DS2-VASc ≥ 2 points indicates a high risk for thromboembolic events [29]. The Glasgow Coma Scale (GCS) [47] and the Markwalder Grading Scale (MGS) [31] were used to classify the severity of symptoms on admission. The Modified Rankin Scale (mRS)[46] was assessed before surgery and at the latest follow-up.
All patients underwent a single burr-hole craniostomy (uni- or bilateral) with intraoperative saline irrigation followed by the insertion of a closed subdural drainage system. A routine control CT scan was performed 1 month after surgery unless clinical deterioration indicated earlier imaging. The routine radiological follow-up was prolonged beyond 1 month on an individual basis if warranted by a clinically significant residual hematoma. Hematoma recurrence was defined as a radiologically confirmed symptomatic CSDH in the same location as the primary hematoma requiring a new operation within 6 months of the primary operation. If a bilateral hematoma was primarily treated with unilateral BHC, a contralateral-sided BHC was also counted as a reoperation. The follow-up was organized by the treating neurosurgical center. After the temporary discontinuation of ATT, the permission to resume the medication was also given by the same neurosurgical unit. Recurrence data was recorded until 6 months after the primary operation and mortality until 3 years.
Statistical analyses
The data was analyzed using IBM SPSS Statistics software (version 27.0.1.0). The level of statistical significance was set to 0.05. Statistically significant differences (p < 0.05) between groups were calculated using Pearson’s Chi-square test for nominal variables unless the subgroup sample was small (n < 30), in which case Fisher’s exact test was used. Independent samples t test was used for comparing means, but for small (n < 30) subgroups we used independent samples Mann–Whitney U test. A bivariate logistic regression analysis was performed with an enter method using factors which had shown statistically significant difference between patient groups. Adjusted odd ratios (OR) with their 95 percent confidence intervals (CI) were computed. Kaplan–Meier analyses were performed to visualize 3-year survival and 6-month recurrence, but patients who died before the 6-month follow-up were excluded from the latter analysis, unless they experienced hematoma recurrence prior to their death.
Results
A total of 301 patients were included in the final study cohort (Fig. 1). The mean age was 76.6 (± 10.4) years, and the proportion of male patients was 200/301 (66.4%). ATT was used by 164 patients (54.5%) at the time of diagnosis, the largest drug subgroups being warfarin (95 patients) and low-dose ASA (56 patients). Direct oral anticoagulant medication was used by four patients (rivaroxaban or dabigatran) and other antiplatelet therapy (clopidogrel, ticagrelor or a combination of low-dose ASA and dipyridamole) by twenty-one patients. Ten patients were on simultaneous warfarin and antiplatelet therapy. A preceding traumatic event was noted in 203 patients (67.4%). Bilateral hematomas were found in 102 patients (33.9%), and of those thirty-nine (38.2%) were primarily operated with bilateral BHC. The overall 3-year mortality was 27.9% (83 of 298 patients).
Forty-seven patients (15.8%) encountered hematoma recurrence which demanded operative treatment. The characteristics of patients with and without hematoma recurrence are compared in Table 1. ATT was not associated with hematoma recurrence (54.2% vs. 55.3%; p = 0.886). The mean time from primary surgery to reoperation was shorter for patients with ATT as compared to patients without ATT, but the difference was not statistically significant (43.0 days vs. 54.1 days; p = 0.323). The mean time from primary surgery to the resumption of medication was significantly longer in patients who experienced a recurrence as compared to patients who required only one operation (59.7 days vs. 122.0 days; p < 0.001), but there was no difference in the incidence of thromboembolic events between the groups. The HAS-BLED score was not associated with recurrence, and the CHA2DS2-VASc score did not predict thromboembolic events.
Male gender and bilateral hematoma showed statistically significant differences between the recurrence and non-recurrence groups. Furthermore, in a logistic regression analysis bilateral hematoma and male gender independently predicted recurrence (Table 2).
The characteristics of patients diagnosed with either unilateral or bilateral chronic subdural hematoma (bCSDH) (n = 199 and n = 102, respectively) were compared (Table 3). The recurrence rate was higher in the bCSDH group (12.6% vs. 22.0%; p = 0.036) (see Table 3 and Fig. 2), but the proportion of patients requiring more than one reoperation did not differ. Patients’ comorbidity profiles did not differ between the groups. The outcomes were worse for patients with unilateral hematomas in terms of 3-year mortality (31.8% vs. 20.0%; p = 0.032) (see Table 3 and Fig. 3).
Seventeen patients (5.7%) experienced a postoperative thromboembolic complication (thirteen strokes/TIAs, two acute myocardial infarctions and three deep vein thrombosis/pulmonary embolisms). Patients on ATT due to previously diagnosed atrial fibrillation did not have an increased risk for postoperative stroke/TIA as compared to patients without a history of atrial fibrillation (6.6% vs. 3.5%; p = 0.240). However, the risk for postoperative stroke/TIA was increased for patients with previous stroke/TIA (2.5% vs. 15.2%; p = 0.001). Only one postoperative stroke/TIA occurred in the recurrence group, and this patient was not on ATT preoperatively. Six other types of postoperative complications were reported in seven patients: two acute subdural hematomas, one intracerebral hemorrhage, seven seizures, one wound infection, one meningitis and two pneumonias.
Of the 102 patients with bCSDH, 63 (61.8%) were primarily operated with unilateral BHC. The recurrence rate did not depend on the primary operation (uni- or bilateral BHC, 22.2% vs. 21.6%; p = 0.944), and the need of more than one reoperation was not higher in the unilateral BHC group (21.4% vs. 12.5%; p = 1.000) (Table 4). The mortality rate was higher in patients with bCSDH who were operated with bilateral BHC (37.8% vs. 9.5%; p < 0.001).
Three patients were lost from follow-up due to their permanent place of residence within the catchment area of another university hospital. For six patients the primary and for twenty patients, the follow-up radiological imaging data was insufficient. For forty-four patients, the indication for ATT was unclear, the use of ATT was sporadic or they died shortly after the operation. Hence, the ATT resumption time could not be reliably determined for these patients.
Discussion
The recurrence rate of operated CSDHs in this population-based cohort was 15.8%, which is in line with previous studies reporting a recurrence risk from 6 to 29% [4, 8,9,10, 12,13,14, 17, 20, 21, 28, 41, 43, 44, 52, 54]. A regression analysis revealed that male gender and a bilateral hematoma are independent risk factors for recurrence, latter of which has been generally recognized also in previous literature [32]. Male gender has previously been reported to predispose to CSDH [53] and was associated with higher recurrence rate in a Danish population-based study in 2015 [42].
The role of antithrombotic therapy in CSDH recurrence is under debate. Several studies have shown ATT to be a risk factor for recurrence [12, 13, 18, 27, 44, 50], whereas a number of studies have come to the opposite conclusion [6, 14, 17, 22, 33, 45, 49]. In addition, different results have been reported between the effect of anticoagulant and antiplatelet medications. In a systematic review, it has been suggested that anticoagulant medication is associated with an increased recurrence risk, whereas antiplatelet medication is not [34]. In our study cohort, neither anticoagulant nor antiplatelet therapy was associated with an increased recurrence risk. The proportion of patients on ATT prior to surgery was 54.8%, which seems to be one of the highest rates reported.
Following surgery, the clinical decision making on ATT continuation is balanced individually between the risk of CSDH recurrence and the risk of thromboembolic complications [37]. The evidence on this issue is rather limited, and clinical guidelines do not exist. Previously, it has been demonstrated that the number of thromboembolic events tends to increase if the discontinuation of ATT is prolonged, and thus, generally prompt resumption is recommended [3, 17, 22]. However, no clear-cut evidence on the optimal duration of the length of the postoperative discontinuation exists [11, 35, 37]. In our study cohort, the ATT discontinuation was relatively long, but the results suggest that even long-term discontinuation may be safe (regardless of the indication of ATT) in terms of thromboembolic events, since their rate was similar in patients who did not experience hematoma recurrence (mean length of discontinuation 59.7 days) and in patients whose discontinuation was prolonged due to recurrence (mean length of discontinuation 122.0 days) (8.3% vs. 8.7%; p = 1.000). However, based on the current study conclusions cannot be drawn on whether a shorter ATT discontinuation period would be sufficient or whether a longer discontinuation would further reduce the recurrence risk. A multicenter randomized controlled trial is warranted to solve this issue.
The use of ATT did not differ between patients with unilateral and bilateral hematomas (Table 3) nor was there a difference in the subgroup of patients with bilateral hematomas, who were operated either unilaterally or bilaterally (Table 4). Previous studies focusing on bCSDH are strikingly limited considering the high frequency and the clinical significance of this condition. The clinical course of the disease may be milder than in unilateral cases, which possibly leads to a delay in the treatment [23]. On the other hand, rapid symptom aggravation can occur [1, 26]. The limited invasiveness of BHC for treating CSDH enables simultaneous evacuation of bilateral hematomas in most patients, although it is not known whether this leads to a better outcome as opposed to treating only the side with the larger hematoma. Bilateral (BHC) treatment was recommended by a Danish group in 2017 based on a hypothesis that the decrease in intracranial pressure caused by unilateral surgery would explain the growth of the contralateral unoperated hematoma [5]. In accordance with this, Zolfaghari and colleagues suggested to consider bilateral evacuation even if the diameter of the contralateral hematoma is below 15 mm [55].
Our data suggests that in bCSDHs, unilateral BHC would be the treatment method-of-choice if the diameter of contralateral hematoma is relatively small. In this study cohort, the mean diameter of the unoperated contralateral hematoma was 9.2 mm, which can be considered as a possible cutoff point in future studies. Furthermore, we argue that it is feasible to consider a unilateral surgical approach even in larger hematomas, since in our results the recurrence rates did not differ between the uni- and bilateral BHC subgroups, and the 3-year mortality appeared to be even higher among the bilaterally operated patients.
The annual incidence of CSDHs requiring surgical evacuation in this population-based cohort was 20.3/100 000 including all patient groups and etiologies. This is in line with recent reports from Finland, which have shown an increasing incidence of CSDHs over the last decades [38, 40, 48], and similar incidences have been reported also in other developed countries. [7, 24] This has been attributed to the widespread use of CT imaging, increased life expectancy and physical activity of elderly people as well as the use of antithrombotic medications. The increasing incidence of CSDHs leads to an increasing socio-economical burden and warrants future randomized studies to optimize treatment algorithms.
Limitations
This is a retrospective register study which is predisposed to biases of observational research. The indications for the use of ATT were partly unclear, and some patients lacked radiological imaging data, which reduced the number of patients in some statistical analyses. Reoperations for recurrent hematomas were performed only for symptomatic cases. However, the routine follow-up CT imaging may have led to reoperations in some cases with very mild clinical symptoms. The strength of this study lies within the population-based, non-selected cohort of consecutive patients, all of whom were treated in a single tertiary center and followed up with a similar protocol.
Conclusions
In this population-based register study, we found that preoperative antithrombotic therapy did not increase the recurrence risk of chronic subdural hematomas. Male gender and bilateral hematomas were more frequently associated with recurrences.
Abbreviations
- SDH:
-
Subdural hematoma
- CSDH:
-
Chronic subdural hematoma
- bCSDH:
-
Bilateral chronic subdural hematoma
- ATT:
-
Antithrombotic therapy
- BHC:
-
Burr-hole craniostomy
- ASDH:
-
Acute subdural hematoma
- ICH:
-
Intracerebral hemorrhage,
- TIA:
-
Transient ischemic attack
References
Agawa Y, Mineharu Y, Tani S, Adachi H, Imamura H, Sakai N (2016) Bilateral chronic subdural hematoma is associated with rapid progression and poor clinical outcome. Neurol Med Chir (Tokyo) 56(4):198–203
Almenawer SA, Farrokhyar F, Hong C et al (2014) Chronic subdural hematoma management: a systematic review and meta-analysis of 34,829 patients. Ann Surg 259(3):449–457
Amano T, Takahara K, Maehara N, Shimogawa T, Mukae N, Sayama T, Arihiro S, Arakawa S, Morioka T, Haga S (2016) Optimal perioperative management of antithrombotic agents in patients with chronic subdural hematoma. Clin Neurol Neurosurg 151:43–50
Andersen-Ranberg NC, Debrabant B, Poulsen FR, Bergholt B, Hundsholt T, Fugleholm K (2019) The Danish chronic subdural hematoma study-predicting recurrence of chronic subdural hematoma. Acta Neurochir (Wien) 161(5):885–894
Andersen-Ranberg NC, Poulsen FR, Bergholt B, Hundsholt T, Fugleholm K (2017) Bilateral chronic subdural hematoma: unilateral or bilateral drainage? J Neurosurg 126(6):1905–1911
Aspegren OP, Åstrand R, Lundgren MI, Romner B (2013) Anticoagulation therapy a risk factor for the development of chronic subdural hematoma. Clin Neurol Neurosurg 115(7):981–984
Balser D, Farooq S, Mehmood T, Reyes M, Samadani U (2015) Actual and projected incidence rates for chronic subdural hematomas in United States Veterans Administration and civilian populations. J Neurosurg 123(5):1209–1215
Bartek JJ, Sjåvik K, Kristiansson H, Ståhl F, Fornebo I, Förander P, Jakola AS (2017) Predictors of recurrence and complications after chronic subdural hematoma surgery: a population-based study. World Neurosurg 106:609–614
Bartek JJ, Sjåvik K, Ståhl F, Kristiansson H, Solheim O, Gulati S, Sagberg LM, Förander P, Jakola AS (2017) Surgery for chronic subdural hematoma in nonagenarians: a Scandinavian population-based multicenter study. Acta Neurol Scand 136(5):516–520
Borger V, Vatter H, Oszvald Á, Marquardt G, Seifert V, Güresir E (2012) Chronic subdural haematoma in elderly patients: a retrospective analysis of 322 patients between the ages of 65–94 years. Acta Neurochir (Wien) 154(9):1549–1554
Chari A, Clemente Morgado T, Rigamonti D (2014) Recommencement of anticoagulation in chronic subdural haematoma: a systematic review and meta-analysis. Br J Neurosurg 28(1):2–7
Choi J, Pyen J, Cho S, Kim J, Koo Y, Whang K (2020) Influence of antithrombotic medication on the risk of chronic subdural hematoma recurrence after burr-hole surgery. J Korean Neurosurg Soc 63(4):513–518
Chon K-H, Lee J-M, Koh E-J, Choi H-Y (2012) Independent predictors for recurrence of chronic subdural hematoma. Acta Neurochir (Wien) 154(9):1541–1548
Cofano F, Pesce A, Vercelli G et al (2020) Risk of recurrence of chronic subdural hematomas after surgery: a multicenter observational cohort study. Front Neurol 11:1448
Ducruet AF, Grobelny BT, Zacharia BE, Hickman ZL, DeRosa PL, Andersen KN, Sussman E, Carpenter A, Connolly ESJ (2012) The surgical management of chronic subdural hematoma. Neurosurg Rev 35(2):155–69 (discussion 169)
Edlmann E, Giorgi-Coll S, Whitfield PC, Carpenter KLH, Hutchinson PJ (2017) Pathophysiology of chronic subdural haematoma: inflammation, angiogenesis and implications for pharmacotherapy. J Neuroinflammation 14(1):108
Fornebo I, Sjåvik K, Alibeck M, Kristiansson H, Ståhl F, Förander P, Jakola AS, Bartek JJ (2017) Role of antithrombotic therapy in the risk of hematoma recurrence and thromboembolism after chronic subdural hematoma evacuation: a population-based consecutive cohort study. Acta Neurochir (Wien) 159(11):2045–2052
Forster MT, Mathé AK, Senft C, Scharrer I, Seifert V, Gerlach R (2010) The influence of preoperative anticoagulation on outcome and quality of life after surgical treatment of chronic subdural hematoma. J Clin Neurosci 17(8):975–979
Gaist D, García Rodríguez LA, Hellfritzsch M, Poulsen FR, Halle B, Hallas J, Pottegård A (2017) Association of antithrombotic drug use with subdural hematoma risk. JAMA 317(8):836–846
Gazzeri R, Laszlo A, Faiola A, Colangeli M, Comberiati A, Bolognini A, Callovini G (2020) Clinical investigation of chronic subdural hematoma: relationship between surgical approach, drainage location, use of antithrombotic drugs and postoperative recurrence. Clin Neurol Neurosurg 191:105705
Gelabert-González M, Iglesias-Pais M, García-Allut A, Martínez-Rumbo R (2005) Chronic subdural haematoma: surgical treatment and outcome in 1000 cases. Clin Neurol Neurosurg 107(3):223–229
Guha D, Coyne S, Macdonald RL (2016) Timing of the resumption of antithrombotic agents following surgical evacuation of chronic subdural hematomas: a retrospective cohort study. J Neurosurg 124(3):750–759
Huang Y-H, Yang K-Y, Lee T-C, Liao C-C (2013) Bilateral chronic subdural hematoma: what is the clinical significance? Int J Surg 11(7):544–548
Karibe H, Kameyama M, Kawase M, Hirano T, Kawaguchi T, Tominaga T (2011) Epidemiology of chronic subdural hematomas. No Shinkei Geka 39(12):1149–1153
Kolias AG, Chari A, Santarius T, Hutchinson PJ (2014) Chronic subdural haematoma: modern management and emerging therapies. Nat Rev Neurol 10(10):570–578
Kurokawa Y, Ishizaki E, Inaba K-I (2005) Bilateral chronic subdural hematoma cases showing rapid and progressive aggravation. Surg Neurol 64(5):444–9 (discussion 449)
Leroy H-A, Aboukaïs R, Reyns N, Bourgeois P, Labreuche J, Duhamel A, Lejeune J-P (2015) Predictors of functional outcomes and recurrence of chronic subdural hematomas. J Clin Neurosci 22(12):1895–1900
Licci M, Kamenova M, Guzman R, Mariani L, Soleman J (2018) Influence of postoperative thrombosis prophylaxis on the recurrence of chronic subdural hematoma after burr-hole drainage. Crit Care Med 46(1):e26–e32
Lip GYH (2011) Implications of the CHA(2)DS(2)-VASc and HAS-BLED scores for thromboprophylaxis in atrial fibrillation. Am J Med 124(2):111–114
Lip GYH, Nieuwlaat R, Pisters R, Lane DA, Crijns HJGM (2010) Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on atrial fibrillation. Chest 137(2):263–272
Markwalder TM (1981) Chronic subdural hematomas: a review. J Neurosurg 54(5):637–645
Miah IP, Tank Y, Rosendaal FR, Peul WC, Dammers R, Lingsma HF, den Hertog HM, Jellema K, van der Gaag NA (2021) Radiological prognostic factors of chronic subdural hematoma recurrence: a systematic review and meta-analysis. Neuroradiology 63(1):27–40
Motoie R, Karashima S, Otsuji R, Ren N, Nagaoka S, Maeda K, Ikai Y, Uno J, Gi H (2018) Recurrence in 787 patients with chronic subdural hematoma: retrospective cohort investigation of associated factors including direct oral anticoagulant use. World Neurosurg 118:e87–e91
Nathan S, Goodarzi Z, Jette N, Gallagher C, Holroyd-Leduc J (2017) Anticoagulant and antiplatelet use in seniors with chronic subdural hematoma: systematic review. Neurology 88(20):1889–1893
Phan K, Abi-Hanna D, Kerferd J, Lu VM, Dmytriw AA, Ho Y-T, Fairhall J, Reddy R, Wilson P (2018) Resumption of antithrombotic agents in chronic subdural hematoma: a systematic review and meta-analysis. World Neurosurg 109:e792–e799
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJGM, Lip GYH (2010) A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest 138(5):1093–1100
Prior A, Fiaschi P, Iaccarino C, Stefini R, Battaglini D, Balestrino A, Anania P, Prior E, Zona G (2021) How do you manage ANTICOagulant therapy in neurosurgery? The ANTICO survey of the Italian Society of Neurosurgery (SINCH). BMC Neurol 21(1):98
Rauhala M, Helén P, Huhtala H, Heikkilä P, Iverson GL, Niskakangas T, Öhman J, Luoto TM (2020) Chronic subdural hematoma-incidence, complications, and financial impact. Acta Neurochir (Wien) 162(9):2033–2043
Rauhala M, Helén P, Seppä K, Huhtala H, Iverson GL, Niskakangas T, Öhman J, Luoto TM (2020) Long-term excess mortality after chronic subdural hematoma. Acta Neurochir (Wien) 162(6):1467–1478
Rauhala M, Luoto TM, Huhtala H, Iverson GL, Niskakangas T, Öhman J, Helén P (2019) The incidence of chronic subdural hematomas from 1990 to 2015 in a defined Finnish population. J Neurosurg 132(4):1147–1157
Ridwan S, Bohrer A-M, Grote A, Simon M (2019) Surgical treatment of chronic subdural hematoma: predicting recurrence and cure. World Neurosurg 128:e1010–e1023
Schmidt L, Gørtz S, Wohlfahrt J, Melbye M, Munch TN (2015) Recurrence of subdural haematoma in a population-based cohort—risks and predictive factors. PLoS One 10(10):e0140450
Schwarz F, Loos F, Dünisch P, Sakr Y, Al SD, Kalff R, Ewald C (2015) Risk factors for reoperation after initial burr hole trephination in chronic subdural hematomas. Clin Neurol Neurosurg 138:66–71
Shen J, Yuan L, Ge R, Wang Q, Zhou W, Jiang XC, Shao X (2019) Clinical and radiological factors predicting recurrence of chronic subdural hematoma: a retrospective cohort study. Injury 50(10):1634–1640
Stanisic M, Lund-Johansen M, Mahesparan R (2005) Treatment of chronic subdural hematoma by burr-hole craniostomy in adults: influence of some factors on postoperative recurrence. Acta Neurochir (Wien) 147(12):1247–1249
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19(5):604–607
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness A practical scale. Lancet (London, England) 2(7872):81–84
Tommiska P, Luostarinen T, Kaprio J, Korja M, Lönnrot K, Kivisaari R, Raj R (2022) Incidence of surgery for chronic subdural hematoma in Finland during 1997–2014: a nationwide study. J Neurosurg 136(4):1186–1193
Torihashi K, Sadamasa N, Yoshida K, Narumi O, Chin M, Yamagata S (2008) Independent predictors for recurrence of chronic subdural hematoma: a review of 343 consecutive surgical cases. Neurosurgery 63(6):1125–9 (discussion 1129)
Wada M, Yamakami I, Higuchi Y, Tanaka M, Suda S, Ono J, Saeki N (2014) Influence of antiplatelet therapy on postoperative recurrence of chronic subdural hematoma: a multicenter retrospective study in 719 patients. Clin Neurol Neurosurg 120:49–54
Waqas M, Vakhari K, Weimer PV, Hashmi E, Davies JM, Siddiqui AH (2019) Safety and effectiveness of embolization for chronic subdural hematoma: systematic review and case series. World Neurosurg 126:228–236
Yamamoto H, Hirashima Y, Hamada H, Hayashi N, Origasa H, Endo S (2003) Independent predictors of recurrence of chronic subdural hematoma: results of multivariate analysis performed using a logistic regression model. J Neurosurg 98(6):1217–1221
Yang W, Huang J (2017) Chronic subdural hematoma: epidemiology and natural history. Neurosurg Clin N Am 28(2):205–210
You W, Zhu Y, Wang Y, Liu W, Wang H, Wen L, Yang X (2018) Prevalence of and risk factors for recurrence of chronic subdural hematoma. Acta Neurochir (Wien) 160(5):893–899
Zolfaghari S, Bartek JJ, Djärf F, Wong S-S, Strom I, Ståhl N, Jakola AS, Nittby Redebrandt H (2021) Risk factors for need of reoperation in bilateral chronic subdural haematomas. Acta Neurochir (Wien). https://doi.org/10.1007/s00701-021-04811-5
Funding
Open access funding provided by University of Eastern Finland (UEF) including Kuopio University Hospital.
Author information
Authors and Affiliations
Contributions
Tuomas Puhakka contributed to the data collection. Tuomas Selander was consulted with the statistical analyses.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
An ethical approval for this study was given by the Ethics Committee of the Hospital District of Northern Savo in February 2018 (286/13.00.00/2018). For this type of study, formal informed consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Brain trauma
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kerttula, S., Huttunen, J., Leinonen, V. et al. The effect of antithrombotic therapy on the recurrence and outcome of chronic subdural hematoma after burr-hole craniostomy in a population-based cohort. Acta Neurochir 164, 2699–2708 (2022). https://doi.org/10.1007/s00701-022-05337-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05337-0