Abstract
Background
As the volume and fidelity of magnetic resonance imaging (MRI) of the brain increase, observation of incidental findings may also increase. We performed a systematic review and meta-analysis to determine the prevalence of various incidental findings.
Methods
PubMed/MEDLINE, EMBASE and SCOPUS were searched from inception to May 24, 2021. We identified 6536 citations and included 35 reports of 34 studies, comprising 40,777 participants. A meta-analysis of proportions was performed, and age-stratified estimates for each finding were derived from age-adjusted non-linear models.
Results
Vascular abnormalities were observed in 423/35,706 participants (9.1/1000 scans, 95%CI 5.2–14.2), ranging from 2/1000 scans (95%CI 0–7) in 1-year-olds to 16/1000 scans (95%CI 1–43) in 80-year-olds. Of these, 204/34,306 were aneurysms (3.1/1000 scans, 95%CI 1–6.3), which ranged from 0/1000 scans (95%CI 0–5) at 1 year of age to 6/1000 scans (95%CI 3–9) at 60 years. Neoplastic abnormalities were observed in 456/39,040 participants (11.9/1000 scans, 95%CI 7.5–17.2), ranging from 0.2/1000 scans (95%CI 0–10) in 1-year-olds to 34/1000 scans (95%CI 12–66) in 80-year-olds. Meningiomas were the most common, in 246/38,076 participants (5.3/1000 scans, 95%CI 2.3–9.5), ranging from 0/1000 scans (95%CI 0–2) in 1-year-olds to 17/1000 scans (95%CI 4–37) in 80-year-olds. Chiari malformations were observed in 109/27,408 participants (3.7/1000 scans, 95%CI 1.8–6.3), pineal cysts in 1176/32,170 (9/1000 scans, 95%CI 1.8–21.4) and arachnoid cysts in 414/36,367 (8.5/1000 scans, 95%CI 5.8–11.8).
Conclusion
Incidental findings are common on brain MRI and may result in substantial resource expenditure and patient anxiety but are often of little clinical significance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past three decades, rapid technological advances have led to increased access and application of magnetic brain imaging (MRI) and computed tomography (CT) in clinical practice and research. As a consequence of improved image resolution, and a rapid rise in demand, detection of incidental findings have increased in both clinical and research context [9, 56]. Intracranial incidental findings are unintended asymptomatic abnormalities diagnosed such as brain neoplasms, aneurysms and vascular malformations [72]. Their clinical significance ranges from normal anatomical variants to pathologies that may require urgent medical or surgical interventions [49].
The prevalence of incidental findings was reported to be 18% in the first large-scale study in 1999, performed on 1000 asymptomatic volunteers (age, 3–83 years) [41]. Previous meta-analyses have reported the prevalence of incidental findings on high-resolution MRI to be 2.7% in adults and 16.4% in children [16]. Although there are some guidelines in place for managing these incidentalomas, clinicians have expressed ambivalence about the ideal management [20, 30]. When participants in the study are healthy volunteers, incidental findings can pose various practical and ethical concerns [31, 34]. The detection of these findings is potentially detrimental, as treatments are often not benign, with potentially harmful consequences [55].
A systematic review was designed to investigate estimates of the prevalence of incidental findings on brain MRI, with or without intravenous contrast, performed for clinical, commercial or research purposes in the general population. We also explored the demographic characteristics, imaging parameters and their influence on the findings. Relatively few studies have explored incidental findings on MRI in a diverse demographic including children and adults. In this review, we explore the nature, incidence and implications of intracranial incidental findings across various imaging modalities to inform patient counselling and further investigation.
Methods
A systematic review and meta-analysis was performed according to the PRISMA guidelines [59] to determine the rate of incidental findings on brain MRI scans.
Inclusion criteria
Studies reporting the prevalence of incidental findings on MR imaging were eligible for inclusion. Studies with significant confounding populations were excluded, such as in patients with neurosurgical referral, evidence of focal neurologic deficit or neuropsychiatric disorder. Given the well-documented associations between many incidental findings and age/gender, we excluded studies not reporting the proportions of males and females scanned and their mean/median age. Studies with scanning indications unlikely to be confounding were included, such as patients referred for assessment of headache or head trauma. In these studies, only definite incidental findings were included in our analysis. Studies which involved only healthy volunteers were examined separately as a sensitivity analysis to test the effect of this criterion, by examining the effect of including studies comprising patients with a clinical indication for brain MRI. Healthy volunteers were defined as patients with no overt neurological complaint being investigated as part of research or a screening process.
Search strategy and selection process
PubMed, Ovid MEDLINE, EMBASE and SCOPUS were searched from inception until May 24, 2021, using the strategies in Supplementary Methods I. Citations were deduplicated using fuzzy logic matching in revtools [78] for R v4.0.2. Abstracts were then independently screened by three authors (DES, EDWT, MAB) using Rayyan QCRI [58], with conflicts solved by discussion with a fourth author (MA or JH). Data was extracted by three authors (DES, EDWT, MAB).
Data abstraction
We sought data on all neoplastic, vascular or other findings identified in the included studies. Lesions identified as meningiomas by the study authors or lesions with a description consistent with a meningioma such as “calcified dural-based lesion” were considered meningiomas. Pituitary lesions include any lesion considered radiographically consistent with an adenoma, which includes micro- and macroadenomas as identified by the study authors. Undifferentiated sellar or suprasellar lesions were recorded separately. Meningiomas, gliomas and pituitary adenomas were enumerated separately given their commonality. The total number of neoplasms includes the above and any other neoplastic findings identified by the study authors, reported in the “any neoplastic” category. Neoplasms not fitting the above categories were enumerated in the “other neoplastic” category.
Cerebral aneurysms were those identified as such by the study authors and included “probable” aneurysms and thrombosed aneurysms where these were reported. We additionally enumerated cavernomas separately. The vascular category includes all vascular malformations, including aneurysms and cavernomas, reported as “any vascular”. Vascular findings not fitting the above were reported as “other vascular”. These included arteriovenous malformations (AVMs) and dural arteriovenous fistulas (dAVFs). Developmental venous anomalies/venous angiomas were excluded. Stenosis of a major vessel was included. In addition to vascular and neoplastic findings, we quantified the number of pineal cysts, arachnoid cysts, and Chiari malformations identified in the included studies.
Morris et al. [55] additionally found that white matter hyperintensities were the most common finding. We did not assess these because we found that the threshold for their reporting appeared to vary and was often poorly described. White matter hyperintensities exist on a spectrum from a clinically insignificant finding to pathologic white matter disease [24], but reporting thresholds are poorly standardised. This issue is exemplified in the findings of Wang et al. [76], who reported the prevalence of hyperintensities stratified into grades in 579 patients. At the lowest threshold, white matter intensities were observed in 566/579 patients (97.8%) [76]. Thus, we did not pool these findings.
Risk of bias assessment
We assessed risk of bias within the included studies by adapting the tool proposed by Hoy et al. [32] for prevalence studies. We assessed the risk of bias in 4 domains relating to external validity and 4 domains relating to internal validity, as shown in Table 1. We assessed between-study bias using funnel plots. Conventional funnel plots using the standard error as a measure of precision may produce false-positive identification of publication bias, and thus, we generated funnel plots of log odds against sample size as suggested by Hunter et al. [33].
Statistical analysis
All statistical analysis was performed using R v4.0.2 [61]. As the primary outcome, we report the age-stratified prevalence (findings per 1000 scans) of the various categories of findings described above. We report crude prevalence as the secondary outcome but consider these estimates of limited value because of the extreme variation in incidences across ages. Crude estimates were derived from random effects meta-analyses of proportions with inverse variance weighting. We did not report the total prevalence of all incidental findings as an aggregate, because studies frequently described the total without fully describing the findings that contribute to it, with varying thresholds for inclusion and consequently incomparable data. We fitted mixed effects restricted cubic spline non-linear mixed effects meta-regression models, with the restricted maximum likelihood (REML) estimator using metafor [73]. Age-stratified estimates were then derived as fitted estimates for each age point. Fitted estimates were derived for ages 1, 2, 5 and 10 years and each decade thereafter. The continuous relationship between age and effect size was also depicted by graphing age versus the fitted spline estimates.
We also fitted linear models and reported the regression coefficient (β) and its 95% confidence interval (95%CI). The summary measure was the back-transformed Freeman-Tukey double arcsine-transformed proportion [50], which was chosen to stabilise variance given that findings are rare. Heterogeneity was quantified by τ2 and its impact by I2 and was derived from the random effects unadjusted crude estimates.
Additional analyses
To assess the impact of including studies in patients with potentially neurological complaints or indications for scanning, a sensitivity analysis was performed wherein estimates were derived as described above from studies recruiting exclusively healthy volunteers/controls. As further sensitivity analyses, we also repeated the analysis using conventional weighted least squares linear regression models, both univariable models and multivariable models including both age and gender. For multivariable models, we computed fitted estimates under the assumption of an equal number of male and female participants. We also examined the effect of publication year and the use of intravenous contrast using meta-regression models, which were additionally adjusted for age. Proportions discussed in relation to these models relate to the median age in the analysis.
Assessment of certainty
We assessed our certainty in the included findings using the GRADE framework, which downgrades certainty qualitatively based on a number of factors including the statistical effect size, its precision, the presence of heterogeneity and within-study bias.
Results
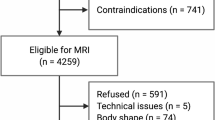
A total of 6356 citations were identified, of which 106 full texts were assessed and 35 reports of 34 studies were included (Fig. 1), comprising 40,777 participants. Some studies which may appear to meet the inclusion criteria were excluded because they were published in a non-English language [5, 75] or did not report sufficient demographic detail [27, 39, 45, 46, 67, 69, 83]. Characteristics of the included studies are provided in Table 2.
Characteristics of the included studies
Risk of bias in each domain is summarised in Fig. 2. Studies were typically at high risk of bias in domains relating to external validity, as samples were often convenience samples or based upon self-referral. Bias relating to internal validity was generally low, because scans were by nature directly sampled from patients and MRI is sensitive and specific for the detection of intracranial abnormalities. Findings for each study are shown in Supplementary Figure I.
Substantial heterogeneity is apparent in our analysis, which is easily appreciated by examining the vertical dispersion of effect sizes in Figs. 3, 4, 5 and 6 and forest plots in Supplementary Figure I. This may be a result of rare findings examined in relatively small sample sizes but may also be a result of differences in methodology and enrolled populations. Magnet strength and sequence differed between studies. The most frequently used strengths were 1.0 T [57, 70, 77], 1.5 T [9, 10, 14, 26, 31, 44, 51, 64, 65, 68, 71, 72, 81], and 3.0 T [3, 12, 25, 28, 29, 40, 42, 48, 49, 76], while some studies used more than one strength (1.5 T and 3 T) [15, 41, 43, 52, 62]. Imaging scans were read by senior radiologists and/or neuroradiologists and/or neurologists in a large number of the included studies [3, 12, 14, 15, 28, 40,41,42,43, 48, 49, 52, 60, 68, 71, 72, 76, 77, 81]. In one study, 2 neuropsychiatrists co-assessed the MRI scans with a neuroradiologist. Only one study [9] had no radiologist, neuroradiologist, or neurologist in the team reading the scans; their team included researchers with a doctor of medicine training in neuropsychology. T1-weighted image (T1WI) [25, 28], T2-weighted image (T2WI) and fluid-attenuated inversion recovery (FLAIR)[57] were the most commonly used MRI sequences, either alone or combined [3, 9, 10, 12, 14, 15, 26, 31, 40,41,42, 44, 48, 49, 52, 62, 65, 68, 71, 72, 76, 77, 81]. Other sequences that were used in a smaller number of published papers were gradient recalled echo T2WI (GRE T2WI) [12, 14, 48, 72, 77], proton density weighted imaging (PDWI) [48], perfusion weighted imaging (PWI) [48], diffusion tensor imaging (DTI) [48], time-of-flight (TOF) [48] angiography and T1/T2 spine echo (SE) [43]. Of the 35 included studies, 11 used a contrast agent [3, 14, 15, 26, 57, 62, 65, 68, 71, 77, 81], which improves the sensitivity of imaging [13].
Relationship between proportion of each vascular finding and age, derived from restricted cubic spline meta-regression models. Red dots show the findings of individual studies, with the size of the point relative to study sample size. Black lines are fitted estimates, while the shaded area is the 95% confidence interval of the fitted estimate
Relationship between proportion of each neoplastic finding and age, derived from restricted cubic spline meta-regression models. Purple dots show the findings of individual studies, with the size of the point relative to study sample size. Black lines are fitted estimates, while the shaded area is the 95% confidence interval of the fitted estimate
Relationship between proportion of each other finding and age, derived from restricted cubic spline meta-regression models. Green dots show the findings of individual studies, with the size of the point relative to study sample size. Black lines are fitted estimates, while the shaded area is the 95% confidence interval of the fitted estimate
There was also substantial variation in patient age, with studies focusing on children [15, 25, 40, 43, 49, 52, 60, 81], adults [3, 14, 28, 29, 31, 41, 62, 68, 77] or the elderly population [9, 10, 22, 26, 42, 44, 48, 57, 64, 65, 71, 72, 76]. This poses substantial analytic challenges. While meta-regression can approximate the relationship between age and prevalence, it is important to note that this approximation may be less valid in the context of rare findings. Ideally, future studies should consider pooling individual patient data to better characterise the relationship between findings and age. Most studies focused on healthy elderly [9, 10, 26, 42, 44, 48, 65, 72, 76], healthy adults [14, 29, 31, 41, 57, 62, 64, 68, 77] and healthy children [25, 40, 49, 60]. Three papers were on children who presented with headaches [43, 52, 81], while one was on adults with headaches [3]. Children with TBI [15], lead-exposed patients [2], patients with diabetes [71] and patients with early Alzheimer’s disease [12] were also the focus for some of the research done. While their inclusion may be considered confounding, excluding these studies in a sensitivity analysis did not substantially influence our results (Supplementary Figure II; Supplementary Table III). An element of selection bias is also possible in that populations were often self-selected volunteers or commercial screening populations, which may be reflective of socio-economic status or other social determinants of health.
Findings
Crude estimates for each category are shown in Fig. 3. Age-stratified estimates of the prevalence of findings per 1000 scans are shown in Table 3. Findings comprising the “other” category are shown in Table 4.
Vascular findings
Cavernomas were the most common vascular finding, observed in 111/34,777 participants (3.9/1000 scans, 95%CI 2.3–5.8), with a range of 0.00001/1000 scans (95%C 0–6) in 1-year-olds to 7/1000 scans (95%CI 0.3–20) in 80-year-olds (Fig. 4). There appeared to be a linear relationship between the proportion of vascular findings observed and increasing patient age (β = 0.002, p < 0.0001; Supplementary Table I). Substantial heterogeneity was observed in effect sizes for vascular findings (τ2 = 0.004, I2 = 94%) (Table 3), likely due to the substantial range of demographics of the included studies.
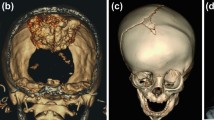
Neoplastic findings
Meningiomas were the most common neoplastic finding, observed in 246/38,076 participants (5.3/1000 scans, 95%CI 2.3–9.5), ranging from 0/1000 scans (95%CI 0–2) in 1-year-olds to 17/1000 scans (95%CI 4–37) in 80-year-olds (Fig. 5). There was a linear association with age (β = 0.002, p < 0.0001; Supplementary Table I). The rate of findings for aggregated neoplasms was 456/39,040 (11.9/1000 scans, 95%CI 7.5–17.2), ranging from 0.2/1000 scans (95%CI 0–10) in 1-year-olds to 34/1000 scans (95%CI 12–66) in 80-year-olds. Moderate heterogeneity was observed (τ2 = 0.003, I2 = 94%) (Table 3). The proportions of chiari malformations, pineal cysts and arachnoid cysts in relation to age are shown in Fig. 6.
Additional analyses
Results of multivariable regressions are shown in Supplementary Table II. A sensitivity analysis limited to healthy volunteers did not appear to alter the relationships between age and findings (Supplementary Figure II) and did not substantially alter our age-stratified estimates (Supplementary Table III). Using linear models appeared to alter the apparent relationship between age and effect size in some analyses, particularly for those appearing to have bimodal relationships in non-linear models (Supplementary Figure III). However, this did not substantially alter our pooled estimates (Supplementary Table IV). Adjusting linear models for gender did not appear to have a substantial effect on the observed relationships (Supplementary Figure IV) or pooled estimates (Supplementary Table V). Funnel plots did not show evidence of publication bias (Supplementary Figure V).
We found that the prevalence of neoplastic findings appeared to increase substantially in newer versus older studies, after adjustment for age (β = 0.004, p < 0.001) but not vascular findings (β = 0.00004, p = 0.98) (Fig. 7). Regression coefficients for all analyses are shown in Supplementary Table VI. The use of intravenous contrast did not appear to influence the age-adjusted proportion of neoplastic (13.2/1000 scans vs. 12.7/1000 scans, p = 0.92) or vascular findings (8.3/1000 scans vs. 8.8/1000 scans, p = 0.91) (Supplementary Table VII).
Relationship between proportion of findings and publication year, derived from multivariable meta-regression models additionally adjusted for age. Proportions on the y-axis relate to median age in the given analysis. Points show the findings of individual studies, with the size of the point relative to study sample size. Black lines are the fitted estimates, while the shaded area is the 95% confidence area of the fitted estimate
Summary of findings
GRADE judgements of certainty are provided in Table 3 for each analysis. We had predominantly low certainty, with estimates downgraded primarily for imprecision, indirectness and within-study bias.
Discussion
This meta-analysis identified a substantial prevalence of various incidental findings on brain MRI, which were most commonly meningiomas. Our analysis included predominantly healthy populations and thus may reasonably approximate the prevalence of these findings in the healthy population. In keeping with a previous analysis by Morris et al. [55], we identified a point prevalence of neoplastic findings of approximately 10 per 1000 scans, with a significant increase with older age. In their study [55], aneurysms were the most common vascular finding. We found a similar prevalence of aneurysms but a higher prevalence of cavernomas, which were the most common vascular finding in our study. Our analysis includes an additional 18 studies (21,218 patients) with a high prevalence of cavernomas in some large studies [9, 12, 42, 68, 76], which accounts for this discrepancy. The reason for this difference is unclear but is likely to be age-related given that we observed substantial correlation with age. This underscores the importance of interpreting crude prevalence with caution in the presence of a strong covariate. Like Morris et al. [55], we also identified a substantial correlation with age for most findings. However, we observed a bimodal relationship with age for arachnoid cysts and a decreasing incidence of Chiari malformations with age. Gliomas were insufficiently common to reliably determine any relationship with age, but an increasing incidence with age is well described in the population [80].
The clinical approach to incidental intracranial findings is uncertain. In particular, the management of common findings such as meningiomas, pituitary adenomas, cavernomas and aneurysms has been the subject of much debate. In the case of meningiomas, treatment for symptomatic presentations is clear in that maximal safe resection is typically the first-line option where feasible [23]. Conversely, the majority of asymptomatic, incidental meningiomas will not require surgical intervention, and the natural history of these lesions is uncertain [36, 37]. Studies have attempted to develop prognostic schema [36], but there are currently no well-validated tools. The management of incidental intracranial aneurysms is also subject to debate [4, 7, 17, 54, 79]. The incidence of aneurysms [74] appears to be significantly larger than that of aneurysmal subarachnoid haemorrhage (aSAH) [18]. Approximately two thirds of aneurysms in the population are < 5 mm in size [74] which, in most cases, appear to have a low risk of rupture [4, 7, 17]. Thus, even in the endovascular era, the risks of treatment may often outweigh the risk of rupture [79].
This then poses an important ethical question as to whether patients should be informed of incidental findings of questionable significance, especially when those findings are unlikely to require treatment [31]. Knowledge of these findings may cause substantial anxiety [21, 38], and thus this question is of particular importance in the context of imaging performed for research purposes in otherwise healthy individuals [31]. In addition, an increase in imaging utilisation [1] and fidelity may lead to a larger volume of incidental findings. Another consideration is a unprecedented level of access to radiology reports by patients [47, 53]. Arguably, explicit consent should be obtained with careful consideration of the implications of incidental findings, and clear thresholds at which findings are considered reportable should be determined [31]. This is particularly important when imaging studies are read by non-radiologists for research purposes [31]. In these situations, review by specialists should ideally be obtained before findings are disclosed to patients and/or further action is taken [31]. Inter-rater reliability should also be accounted for, given that disagreement may occur as to what warrants further evaluation. This is exemplified by incidental pituitary lesions—one study identified pituitary abnormalities in over 40% of patients, but with significant inter-rater variability [27]. The majority of small (≤ 1 cm) non-functioning adenomas will never enlarge [19], and thus, there is the question as to the approach to lesions with disagreement between evaluators. As such, clear guidelines and algorithms should arguably be enacted to facilitate consistent decision-making. These may also be of benefit when considering medico-legal implications[6], as decisions to forego treatment may be scrutinised in the event of preventable complications of a known, but untreated, pathology.
Incidental findings also carry economic implications [21]. It is important to note that there is no evidence of a concrete, patient-centred benefit to their identification. In a study of 5800 patients, Bos et al. [9] identified 143 meningiomas. Of these, 91 (63.6%) were referred for further assessment and only 15 (10.4%) required intervention [9]. In total, 188 of 549 findings (32%) required specialist referral and only 44 (8%) required further follow-up or intervention; one for every 131 scans performed [9]. Thus, it appears that approximately one third of incidental findings create additional workload in the form of specialist referral, but only a minority require further intervention or follow-up. This carries cost and anxiety for the patient, but may infrequently result in intervention, and thus the risk–benefit balance is uncertain. As an example, the utility of empiric screening for intracranial aneurysms has been highly debated given their commonality, the devastating outcomes of aSAH and the existence of an effective treatment [63]. However, even in a Japanese population known to be at particularly high-risk of aSAH [18], Yoshimoto et al. found that empiric screening is not cost-effective [82].
For patients, there are also implications for underwriting of personal insurance and bank loans. The presence of an intracranial finding may increase premium rates or even exclude the applicant entirely. For example, the presence of multiple cerebral aneurysms, suggesting a genetic component, or untreated aneurysms with high risk features may preclude underwriting [66]. This may seriously affect patients, especially younger individuals yet to obtain life insurance or mortgages. These consequences are often overlooked by patients and clinicians, but it is recommended they are explicitly discussed with patients undergoing imaging for screening or research purposes [8].
Limitations
There are several limitations to this study. Firstly, we observed substantial variation in methodological components of included studies, such as magnet strengths and sequences. This was reflected in substantial heterogeneity in many analyses, which limits the certainty of our findings. Perhaps more importantly, the reporting threshold for incidental findings was not standardised in our analysis and was often undefined or unclear in the included studies. As imaging fidelity improves, the size threshold for the visual detection of lesions is becoming smaller, and thus, it is possible and even likely that this threshold varied across the studies, which may bias estimates. Given the very strong relationship between mean age in the study and the prevalence of findings identified, raw proportions for each finding may be less informative. The enrolled populations in included studies also varied substantially, which may influence baseline risk for the various findings assessed and bias our estimates. We observed substantial heterogeneity in many cases, which limits our confidence. This analysis assesses predominantly outwardly healthy individuals and thus generalisability to hospital populations, in which most incidental findings are identified in practice, may be limited.
Conclusion
We identified a substantial prevalence of incidental findings on MRI brain in predominantly healthy volunteers. Meningiomas appear to be the most common of these, though their prevalence is highly age-dependent. The significance and optimal management of incidental findings is uncertain, and future studies should consider reporting their natural history and clinical course. Future reviews should consider obtaining individual patient data to better describe the relationship between age and prevalence.
Data availability
The datasets from which these results are generated are collated from the literature and available upon reasonable request to the corresponding author.
Statistical code
The statistical code used to generate these results is available upon reasonable request to the corresponding author.
References
Agarwal R, Bergey M, Sonnad S, Butowsky H, Bhargavan M, Bleshman MH (2010) Inpatient CT and MRI utilization: trends in the academic hospital setting. J Am Coll Radiol 7(12):949–955
Alphs HH, Schwartz BS, Stewart WF, Yousem DM (2006) Findings on brain MRI from research studies of occupational exposure to known neurotoxicants. AJR Am J Roentgenol 187(4):1043–1047
Alturkustani A, Bock Y, Bajunaid K, Lingawi S, Baeesa S (2020) Significant incidental brain magnetic resonance imaging findings in migraine headache patients: retrospective cross-sectional study. Clin Neurol Neurosurg. https://doi.org/10.1016/j.clineuro.2020.106019
Backes D, Rinkel GJE, Greving JP et al (2017) ELAPSS score for prediction of risk of growth of unruptured intracranial aneurysms. Neurology 88(17):1600–1606
Baumgart D, Egelhof T (2007) Preventive whole-body screening encompassing modern imaging using magnetic resonance tomography. Herz 32(5):387–394
Berlin L (2011) The incidentaloma: a medicolegal dilemma. Radiol Clin North Am 49(2):245–255
Bijlenga P, Gondar R, Schilling S, Morel S, Hirsch S, Cuony J, Corniola M-V, Perren F, Rüfenacht D, Schaller K (2017) PHASES score for the management of intracranial aneurysm. Stroke 48(8):2105–2112
Booth T, Jackson A, Wardlaw J, Taylor S, Waldman A (2010) Incidental findings found in “healthy” volunteers during imaging performed for research: current legal and ethical implications. Br J Radiol 83(990):456–465
Bos D, Poels MMF, Adams HHH et al (2016) Prevalence, clinical management, and natural course of incidental findings on brain MR images: the population-based Rotterdam scan study. Radiology 281(2):507–515
Boutet C, Vassal F, Celle S, Schneider FC, Barthélémy J-C, Laurent B, Barral F-G, Roche F (2017) Incidental findings on brain magnetic resonance imaging in the elderly:the PROOF study. Brain Imaging Behav 11(1):293–299
Boutet C, Vassal F, Celle S, Schneider FC, Barthelemy J-C, Laurent B, Barral F-G, Roche F (2017) Incidental findings on brain magnetic resonance imaging in the elderly:the PROOF study. Brain Imaging Behav 11(1):293–299
Brugulat-Serrat A, Rojas S, Bargalló N, Conesa G, Minguillón C, Fauria K, Gramunt N, Molinuevo JL, Gispert JD (2017) Incidental findings on brain MRI of cognitively normal first-degree descendants of patients with Alzheimer’s disease: A cross-sectional analysis from the ALFA (Alzheimer and Families) project. BMJ Open. https://doi.org/10.1136/bmjopen-2016-013215
Cai X, Zhu Q, Zeng Y, Zeng Q, Chen X, Zhan Y (2019) Manganese oxide nanoparticles as MRI contrast agents in tumor multimodal imaging and therapy. Int J Nanomedicine 14:8321
Cieszanowski A, Maj E, Kulisiewicz P, Grudzinski IP, Jakoniuk-Glodala K, Chlipala-Nitek I, Kaczynski B, Rowinski O (2014) Non-contrast-enhanced whole-body magnetic resonance imaging in the general population: the incidence of abnormal findings in patients 50 years old and younger compared to older subjects. PLoS ONE 9(9):e107840
Cohrs G, Huhndorf M, Niemczyk N, Volz LJ, Bernsmeier A, Singhal A, Larsen N, Synowitz M, Knerlich-Lukoschus F (2018) MRI in mild pediatric traumatic brain injury: diagnostic overkill or useful tool? Child’s Nerv Syst 34(7):1345–1352
Dangouloff-Ros V, Roux C-J, Boulouis G, Levy R, Nicolas N, Lozach C, Grevent D, Brunelle F, Boddaert N, Naggara O (2019) Incidental brain MRI findings in children: a systematic review and meta-analysis. Am J Neuroradiol 40(11):1818–1823
Detmer FJ, Hadad S, Chung BJ et al (2019) Extending statistical learning for aneurysm rupture assessment to Finnish and Japanese populations using morphology, hemodynamics, and patient characteristics. Neurosurg Focus. https://doi.org/10.3171/2019.4.FOCUS19145
Etminan N, Chang HS, Hackenberg K, De Rooij NK, Vergouwen MDI, Rinkel GJE, Algra A (2019) Worldwide incidence of aneurysmal subarachnoid hemorrhage according to region, time period, blood pressure, and smoking prevalence in the population: a systematic review and meta-analysis. JAMA Neurol 76(5):588–597
Fernández-Balsells MM, Murad MH, Barwise A et al (2011) Natural history of nonfunctioning pituitary adenomas and incidentalomas: a systematic review and metaanalysis. J Clin Endocrinol Metab 96(4):905–912
Freda P, Katznelson L, Molitch M (2011) Patient guide to pituitary incidentaloma assessment and treatment. J Clin Endocrinol Metab 96(4):35A-36A
Ganguli I, Simpkin AL, Lupo C, Weissman A, Mainor AJ, Orav EJ, Rosenthal MB, Colla CH, Sequist TD (2019) Cascades of care after incidental findings in a US national survey of physicians. JAMA Netw Open. https://doi.org/10.1001/JAMANETWORKOPEN.2019.13325
Glasmacher SA, Thomas HS, Stirland L, Wilkinson T, Lumsden J, Langlands G, Waddell B, Holloway G, Thompson G, Pal S (2020) Incidental findings identified on head MRI for investigation of cognitive impairment: a retrospective review. Dement Geriatr Cogn Disord 48(3–4):123–130
Goldbrunner R, Stavrinou P, Jenkinson MD et al (2021) EANO guideline on the diagnosis and management of meningiomas. Neuro Oncol 23(11):1821–1834
Gunning-Dixon FM, Brickman AM, Cheng JC, Alexopoulos GS (2009) Aging of cerebral white matter: a review of MRI findings. Int J Geriatr Psychiatry 24(2):109–117
Gur RE, Kaltman D, Melhem ER, Ruparel K, Prabhakaran K, Riley M, Yodh E, Hakonarson H, Satterthwaite T, Gur RC (2013) Incidental findings in youths volunteering for brain MRI research. AJNR Am J Neuroradiol 34(10):2021–2025
Haberg AK, Hammer TA, Kvistad KA, Rydland J, Muller TB, Eikenes L, Garseth M, Stovner LJ (2016) Incidental intracranial findings and their clinical impact; the HUNT MRI study in a general population of 1006 participants between 50–66 years. PLoS ONE 11(3):e0151080
Hall WA, Luciano MG, Doppman JL, Patronas NJ, Oldfield EH (1994) Pituitary magnetic resonance imaging in normal human volunteers: occult adenomas in the general population. Ann Intern Med 120(10):817–820
Hanna KF, Sayles HR, O’Neill J, White ML, Wilson TW, Swindells S (2020) Incidental findings on brain MRI in people with HIV infection. Sci Rep 10(1):9474
Hartwigsen G, Siebner HR, Deuschl G, Jansen O, Ulmer S (2010) Incidental findings are frequent in young healthy individuals undergoing magnetic resonance imaging in brain research imaging studies: a prospective single-center study. J Comput Assist Tomogr 34(4):596–600
Hitzeman N, Cotton E (2014) Incidentalomas: initial management. Am Fam Physician 90(11):784–789
Hoggard N, Darwent G, Capener D, Wilkinson ID, Griffiths PD (2009) The high incidence and bioethics of findings on magnetic resonance brain imaging of normal volunteers for neuroscience research. J Med Ethics 35(3):194–199
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Baker P, Smith E, Buchbinder R (2012) Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 65(9):934–939
Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ (2014) In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol 67(8):897–903
Illes J, Desmond JE, Huang LF, Raffin TA, Atlas SW (2002) Ethical and practical considerations in managing incidental findings in functional magnetic resonance imaging. Brain Cogn 50(3):358–365
Illes J, Rosen AC, Huang L, Goldstein RA, Raffin TA, Swan G, Atlas SW (2004) Ethical consideration of incidental findings on adult brain MRI in research. Neurology 62(6):888–890
Islim AI, Kolamunnage-Dona R, Mohan M, Moon RDC, Crofton A, Haylock BJ, Rathi N, Brodbelt AR, Mills SJ, Jenkinson MD (2020) A prognostic model to personalize monitoring regimes for patients with incidental asymptomatic meningiomas. Neuro Oncol 22(2):278–289
Islim AI, Mohan M, Moon RDC, Rathi N, Kolamunnage-Dona R, Crofton A, Haylock BJ, Mills SJ, Brodbelt AR, Jenkinson MD (2020) Treatment outcomes of incidental intracranial meningiomas: results from the IMPACT cohort. World Neurosurg 138:e725–e735
Jagadeesh H, Bernstein M (2014) Patients’ anxiety around incidental brain tumors: a qualitative study. Acta Neurochir (Wien) 156(2):375–381
Jansen PR, Dremmen M, van den Berg A et al (2017) Incidental findings on brain imaging in the general pediatric population. N Engl J Med 377(16):1593–1595
Kaiser D, Leach J, Vannest J, Schapiro M, Holland S, Consortium CMRI of N (CMIND) A (2015) Unanticipated findings in pediatric neuroimaging research: prevalence of abnormalities and process for reporting and clinical follow-up. Brain Imaging Behav 9(1):32–42
Katzman GL, Dagher AP, Patronas NJ (1999) Incidental findings on brain magnetic resonance imaging from 1000 asymptomatic volunteers. JAMA 282(1):36–39
Keuss SE, Parker TD, Lane CA et al (2019) Incidental findings on brain imaging and blood tests: results from the first phase of Insight 46, a prospective observational substudy of the 1946 British birth cohort. BMJ Open 9(7):e029502
Kim BS, Illes J, Kaplan RT, Reiss A, Atlas SW (2002) Incidental findings on pediatric MR images of the brain. AJNR Am J Neuroradiol 23(10):1674–1677
Koncz R, Mohan A, Dawes L, Thalamuthu A, Wright M, Ames D, Lee T, Trollor J, Wen W, Sachdev P (2018) Incidental findings on cerebral MRI in twins: the Older Australian Twins Study. Brain Imaging Behav 12(3):860–869
Kumar R, Sachdev PS, Price JL, Rosenman S, Christensen H (2008) Incidental brain MRI abnormalities in 60- to 64-year-old community-dwelling individuals: data from the Personality and Total Health Through Life study. Acta Neuropsychiatr 20(2):87–90
Kumra S, Ashtari M, Anderson B, Cervellione KL, Kan LI (2006) Ethical and practical considerations in the management of incidental findings in pediatric MRI studies. J Am Acad Child Adolesc Psychiatry 45(8):1000–1006
Lee CI, Langlotz CP, Elmore JG (2016) Implications of direct patient online access to radiology reports through patient web portals. J Am Coll Radiol 13(12):1608–1614
Li S, Fang F, Cui M et al (2019) Incidental findings on brain MRI among Chinese at the age of 55–65 years: the Taizhou Imaging Study. Sci Rep 9(1):464
Li Y, Thompson WK, Reuter C et al (2021) Rates of incidental findings in brain magnetic resonance imaging in children. JAMA Neurol 78(5):578–587
Lin L, Xu C (2020) Arcsine-based transformations for meta-analysis of proportions: pros, cons, and alternatives. Heal Sci Reports. https://doi.org/10.1002/hsr2.178
Lubman DI, Velakoulis D, McGorry PD, Smith DJ, Brewer W, Stuart G, Desmond P, Tress B, Pantelis C (2002) Incidental radiological findings on brain magnetic resonance imaging in first-episode psychosis and chronic schizophrenia. Acta Psychiatr Scand 106(5):331–336
Mar S, Kelly JE, Isbell S, Aung WY, Lenox J, Prensky A (2013) Prevalence of white matter lesions and stroke in children with migraine. Neurology 81(16):1387–1391
Miles RC, Hippe DS, Elmore JG, Wang CL, Payne TH, Lee CI (2016) Patient access to online radiology reports: frequency and sociodemographic characteristics associated with use. Acad Radiol 23(9):1162–1169
Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, Holman R (2002) International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 360(9342):1267–1274
Morris Z, Whiteley WN, Longstreth WTJ et al (2009) Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ 339:b3016
O’Sullivan JW, Muntinga T, Grigg S, Ioannidis JPA (2018) Prevalence and outcomes of incidental imaging findings: umbrella review. BMJ. https://doi.org/10.1136/bmj.k2387
Onizuka M, Suyama K, Shibayama A, Hiura T, Horie N, Miyazaki H (2001) Asymptomatic brain tumor detected at brain check-up. Neurol Med Chir (Tokyo) 41(9):431–435
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan-a web and mobile app for systematic reviews. Syst Rev. https://doi.org/10.1186/s13643-016-0384-4
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Potchen MJ, Kampondeni SD, Mallewa M, Taylor TE, Birbeck GL (2013) Brain imaging in normal kids: a community-based MRI study in Malawian children. Trop Med Int Health 18(4):398–402
R Core Team (2020) R: a language and environment for statistical computing
Reneman L, de Win MML, Booij J, van den Brink W, den Heeten GJ, Freling N, Majoie CBLM (2012) Incidental head and neck findings on MRI in young healthy volunteers: prevalence and clinical implications. AJNR Am J Neuroradiol 33(10):1971–1974
Rinkel GJE, Ruigrok YM (2021) Preventive screening for intracranial aneurysms. Int J Stroke. https://doi.org/10.1177/17474930211024584
Rocque BG, Baskaya MK, Kuo JS (2008) Incidental findings on brain MRI. N Engl J Med 358(8):853–855
Sandeman EM, Hernandez MDCV, Morris Z et al (2013) Incidental findings on brain MR imaging in older community-dwelling subjects are common but serious medical consequences are rare: a cohort study. PLoS ONE 8(8):e71467
Scharf E, Pelkowski S, Sahin B (2017) Unruptured intracranial aneurysms and life insurance underwriting. Neurol Clin Pract 7(3):274–277
Seki A, Uchiyama H, Fukushi T, Sakura O, Tatsuya K (2010) Incidental findings of brain magnetic resonance imaging study in a pediatric cohort in Japan and recommendation for a model management protocol. J Epidemiol 20(Supplement_II):S498–S504
Serag D, Ragab E (2020) Prevalence of incidentally discovered findings on brain MRI in adult Egyptian population. Egypt J Radiol Nucl Med. https://doi.org/10.1186/s43055-020-00187-1 LK - http://jq6am9xs3s.search.serialssolutions.com/?sid=EMBASE&issn=20904762&id=doi:10.1186%2Fs43055-020-00187-1&atitle=Prevalence+of+incidentally+discovered+findings+on+brain+MRI+in+adult+Egyptian+population&stitle=Egypt.+J.+Radiol.+Nucl.+Med.&title=Egyptian+Journal+of+Radiology+and+Nuclear+Medicine&volume=51&issue=1&spage=&epage=&aulast=Serag&aufirst=Dena&auinit=D.&aufull=Serag+D.&coden=&isbn=&pages=-&date=2020&auinit1=D&auinitm=
Sullivan EV, Lane B, Kwon D et al (2017) Structural brain anomalies in healthy adolescents in the NCANDA cohort: relation to neuropsychological test performance, sex, and ethnicity. Brain Imaging Behav 11(5):1302–1315
Tsushima Y, Taketomi-Takahashi A, Endo K (2005) Prevalence of abnormal findings on brain magnetic resonance (MR) examinations in adult participants of brain docking. BMC Neurol 2005 51 5(1):1–6
Vázquez-Justes D, Sanahuja J, Diez J, Rubinat E, Begué R, Salas C, Vicandi C, Gil MI, Purroy F, Mauricio D (2020) Incidental findings on brain MRI in a cohort of diabetic patients. J Neuroradiol 47(5):343–348
Vernooij MW, Ikram MA, Tanghe HL, Vincent AJPE, Hofman A, Krestin GP, Niessen WJ, Breteler MMB, van der Lugt A (2007) Incidental findings on brain MRI in the general population. N Engl J Med 357(18):1821–1828
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor. J Stat Softw 36(3):1–48
Vlak MHM, Algra A, Brandenburg R, Rinkel GJE (2011) Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol 10(7):626–636
Wahlund L, Agartz I, Saaf J, Wetterberg L, Marions O (1989) Magnetic resonance tomography in psychiatry–clear benefits for health care services. Lakartidningen 86(46):3991–3994
Wang L, Lin H, Peng Y et al (2021) Incidental brain magnetic resonance imaging findings and the cognitive and motor performance in the elderly: the Shanghai Changfeng Study. Front Neurosci. https://doi.org/10.3389/fnins.2021.631087
Weber F, Knopf H (2006) Incidental findings in magnetic resonance imaging of the brains of healthy young men. J Neurol Sci 240(1–2):81–84
Westgate MJ (2019) revtools: an R package to support article screening for evidence synthesis. Res Synth Methods 10(4):606–614
Wiebers DO (2003) Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 362(9378):103–110
Wrensch M, Minn Y, Chew T, Bondy M, Berger MS (2002) Epidemiology of primary brain tumors: current concepts and review of theliterature. Neuro Oncol 4(4):278–299
Yılmaz Ü, Çeleğen M, Yılmaz TS, Gürçınar M, Ünalp A (2014) Childhood headaches and brain magnetic resonance imaging findings. Eur J Paediatr Neurol 18(2):163–170
Yoshimoto Y, Wakai S (1999) Cost-effectiveness analysis of screening for asymptomatic, unruptured intracranial aneurysms: a mathematical model. Stroke 30(8):1621–1627
Yue NC, Longstreth WT, Elster AD, Jungreis CA, O’Leary DH, Poirier VC (1997) Clinically serious abnormalities found incidentally at MR imaging of the brain: data from the Cardiovascular Health Study. 202(1):41–46. https://doi.org/10.1148/radiology20218988190
Funding
Open Access funding provided by the IReL Consortium
Author information
Authors and Affiliations
Contributions
Concept and design: MA, JH, MJ.
Screening and data collation: DES, MA, MAB, EDWT, JH.
Statistical analysis: JH.
Interpretation of data: DES, MA, MAB, EDWT, JH, MJ.
Writing: DES, MA, MAB, EDWT, JH, MJ.
Review and revision of manuscript: DES, MA, MAB, EDWT, JH, MJ.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neurosurgery general.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sunny, D.E., Amoo, M., Al Breiki, M. et al. Prevalence of incidental intracranial findings on magnetic resonance imaging: a systematic review and meta-analysis. Acta Neurochir 164, 2751–2765 (2022). https://doi.org/10.1007/s00701-022-05225-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05225-7