Abstract
Background
Fatty filum terminale is a form of spinal dysraphism and a third of all patients develop symptoms such as sensory, motor, and urinary impairment. Early surgery at 6 months has the advantage that the bone density is still soft, and the patients are not ambulatory yet, promoting faster healing.
Method
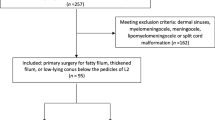
We present our minimal invasive surgical technique for FFT untethering.
Conclusion
Due to the low complication rate and the potentially high benefit of surgery, prophylactic untethering is recommended.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fatty filum terminale (FFT) potentially results in a tethered cord. Approximately, a third of all patients with a FFT present with skin stigmata in the lumbosacral area [1], and can become symptomatic presenting with sensory or motor deficits, urinary incontinence or urgency, back and leg pain, and scoliosis. The classical treatment of FFT is a one to two level laminectomy and microsurgical untethering of the FFT, ideally at 6–9 months of age [6]. We present our technique of FFT untethering through a minimal invasive interlaminar approach and a small durotomy.
Relevant surgical anatomy
The spinous process, which is often bifid in children < 6 years, lamina on each side of it, and facet joints are the bony landmarks. In small children, the disc space has approximately the same height as the vertebral body resulting in a larger interlaminar space, facilitating a minimal invasive approach. The filum terminale interna origins at the lower tip of the conus medullaris (CM) and continues to the end of the thecal sac [2]. Physiologically, the filum terminale has a high elasticity, which allows it to reduce elongation stress to the CM [2]. The increased fat content in a FFT reduces its elasticity, resulting in tension to the CM [9, 10]. The normal filum terminale diameter is 2 mm at the level L5/S1 and any larger diameter is considered pathological [5]. Typically, a FFT leads to a low-lying conus (under the level of L1) leading to a tethered cord syndrome. However, a normally positioned conus does not exclude the diagnosis of a FFT [10].
Description of surgical technique
Under general anesthesia, the patient is placed in prone position. Jelly rolls are positioned in a parallel fashion to the body from the mid clavicle to the iliac crest across the thorax to carefully pad all pressure points and relieve any abdominal pressure. Intraoperative neuromonitoring monitoring (IONM) with 14–16 muscles from L1 to S4 is recorded including anal sphincter electrodes for the bulbocavernosus reflex (Fig. 1). The level of incision is individually guided by the maximal point of fat within the filum. In infants, no routine fluoroscopy but anatomical landmarks are used to verify the level of incision. An approximately 3-cm-long midline incision is made (Fig. 2A). A subperiosteal dissection of the muscles on both sides exposing the laminae is conducted (Fig. 2B). The interspinous ligament is removed followed by a flavectomy. At times, very small portion of the laminae is resected (Fig. 2C). The interlaminar approach leads to a 1–1.5-cm dural exposure. Meticulous extradural hemostasis with coagulation, bone wax, and hemostatic agents (e.g., Floseal, Baxter International, Volketswil, Switzerland) is achieved. Using the surgical microscope, a midline durotomy of 0.8–1 cm is performed. The FFT is identified by its yellow appearance, and it is usually positioned in the midline (Fig. 2D). The FFT is dissected off the adjacent nerve roots and mobilized using a Rhoton microdissector. A small cotton patty is placed under the mobilized filum to keep it in place and create a barrier to the normal cauda equina nerve roots. Using a concentric bipolar stimulator probe with 0.2 milli Ampere (mA), the normal motor nerve roots are stimulated for quality control. Thereafter, the isolated FFT is stimulated with up to 10 mA while no motor response should be evoked (Fig. 2E). Bipolar diathermy is used to cauterize the FFT before transection. A small piece of FFT is sent for histopathological review for quality control. The cranial end is held in place with the bayonet forceps and its tip is thoroughly cauterized to avoid any bleeding (Fig. 2F). After its release, it often retracts rapidly cranially. The dura is closed in a watertight fashion using Ti-Cron™ (Medtronic, Minneapolis, MN, USA) 5–0 continuous suturing and fibrin sealant (TISSEEL, Baxter International, Volketswil, Switzerland) (Fig. 2G and H). Valsalva maneuver is performed to check for any CSF leak. The wound is closed in layers, using Vicryl 3–0 stitches for the fascia and Vicryl 4–0 stitches for the subcutaneous tissue. The skin is closed using an adhesive net and skin glue (Dermabond Prineo ®, Skin closure system, Ethicon Inc., Raritan, USA) (Fig. 2I, Video 1).
Surgical steps for fatty filum terminale untethering: A midline skin incision; B subperiosteal dissection of the muscle to expose the spinous process and lamina on both sides; C a small interlaminar approach is performed to visualize the dural sac; D dissection and careful mobilization of the fatty filum terminale; E electric stimulation of the fatty filum terminale before untethering; F dissected and cauterized cranial end of the fatty filum terminale; G watertight continuous dura closure with 4–0 PDS; H application of fibrin sealant (Tisseel, Baxter Inc.) to ensure dural closure; I skin closure of the small 3-cm-long incision with Dermabond Prineo® skin sealant system (Ethicon Inc., Raritan, NJ, USA)
Indications
Symptomatic patients diagnosed with FFT and regardless of the level of the CM should undergo surgery. No clear consensus exists for asymptomatic or oligosymptomatic patients with a FFT but normally placed CM or asymptomatic patients with an FFT and a low-lying CM [7, 8]. The advantage of prophylactic surgery (80% of all cases) is to avoid the development of neurologic deficits or scoliosis, which can occur in around 30% of the cases. The goal and reason of conducting the surgery must therefore be explained very thoroughly to the parents, for them to achieve an informed consent. Although controversial, we recommend surgery using IOM for quality control during surgery [4].
Surgery is ideally offered at the age of 6–9 months as it is early enough to avoid any neurologic damage, should they become symptomatic from the FFT, and has the advantage of a relatively soft bone, and less muscle tissue, facilitating surgery and recovery, allowing a minimal invasive approach, and reducing blood loss. Due to the low complication rate of around 2–4% and the potentially high benefit of surgery, we recommend prophylactic surgery to all of these children [3, 5].
Limitations
Our minimal invasive approach has the limitation of a very small bone window and durotomy which at times might lead to difficulty in detecting the FFT.
How to avoid complications
Even with IONM in place, careful dissection of the FFT from the cauda equina fibers needs to be ensured to avoid iatrogenic neurologic deficits. It is of paramount importance to ensure a watertight dura closure to prevent postoperative CSF leaks. This can either be achieved by continuous or interrupted suturing and possible addition of a sealant.
Specific perioperative considerations
In our institute, we run an interdisciplinary clinic including pediatric neurosurgeons, neurologist, and urologist to assess these patients together. All patients should receive an MRI of the whole neuroaxis to exclude other concurrent pathologies (Chiari malformation, hydrocephalus, scoliosis). The level of the conus is best assessed in T2-weighted sequences, while the FFT is best visualized in non-fat-suppressed T1-weighted sequences.
In our practice, all patients receive a urinary catheter, which is removed 1–2 days after surgery, to prevent urinary retention, especially when patients are treated with morphine. After surgery, patients are kept in a horizontal position for 48 h to avoid a CSF fistula. As of the third postoperative day, babies should be showered, while the Dermabond Prineo® is removed 14 days after surgery in our outpatient clinic.
Specific information for the patients about surgery and potential risks
The risk of possible neurological deficits despite the use of IONM or development CSF fistula is low (0–4%) [3, 5]. Re-tethering can occur in 2.7–8.6% of the cases and might indicate repeat surgery [5, 10]. The risk of wound infection is around 2–5% [3, 5]. In our experience, the overall risks and risk of postoperative CSF fistula are lower with a minimal invasive approach.
References
Cornips EMJ, Vereijken IMP, Beuls EAM et al (2012) Clinical characteristics and surgical outcome in 25 cases of childhood tight filum syndrome. Eur J Paediatr Neurol 16(2):103–117. https://doi.org/10.1016/j.ejpn.2011.07.002
De Vloo P, Monea AG, Sciot R, van Loon J, Van Calenbergh F (2016) The filum terminale: a cadaver study of anatomy, histology, and elastic properties. World Neurosurg 90:565-573.e1. https://doi.org/10.1016/j.wneu.2015.12.103
Ishisaka E, Usami K, Ogiwara H (2020) Surgical outcomes by sectioning a filum terminale in patients with terminal syringomyelia. Childs Nerv Syst 36(12):3035–3039. https://doi.org/10.1007/s00381-020-04615-5
Lalgudi Srinivasan H, Valdes-Barrera P, Agur A, Soleman J, Ekstein M, Korn A, Vendrov I, Roth J, Constantini S (2021) Filum terminale lipomas—the role of intraoperative neuromonitoring. Childs Nerv Syst 37(3):931–939. https://doi.org/10.1007/s00381-020-04856-4
Ostling LR, Bierbrauer KS, Kuntz C (2012) Outcome, reoperation, and complications in 99 consecutive children operated for tight or fatty filum. World Neurosurg. Published online 5
Samuels R, McGirt MJ, Attenello FJ, Garcés Ambrossi GL, Singh N, Solakoglu C, Weingart JD, Carson BS, Jallo GI (2009) Incidence of symptomatic retethering after surgical management of pediatric tethered cord syndrome with or without duraplasty. Childs Nerv Syst 25(9):1085–1089. https://doi.org/10.1007/s00381-009-0895-6
Steinbok P, Gupta N (2006) Occult tethered cord syndrome: a survey of practice patterns. J Neurosurg 104:5
Steinbok P, MacNeily AE, Hengel AR et al (2016) Filum section for urinary incontinence in children with occult tethered cord syndrome: a randomized, controlled pilot study. J Urol 195(4 Part 2):1183–1188. https://doi.org/10.1016/j.juro.2015.09.082
Yamada S, Yamada BS (2007) Pathophysiology of tethered cord syndrome and similar complex disorders. Neurosurg Focus 23:10
Yong RL Habrock-Bach T Vaughan M Kestle JR Steinbok P. Symptomatic retethering of the spinal cord after section of a tight filum terminale. :9
Funding
Open access funding provided by University of Basel.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
No approval from the ethics committee was sought as this is a technical description not including patient data or identifying information.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
-Prophylactic surgery is offered to the parents since the benefit overweighs the periprocedural risks.
-Surgery ideally performed between 6 and 9 months of age.
-Skin stigmata, neurological symptoms, and imaging (US and MRI) usually lead to the diagnosis.
-Study the MRI images carefully to assess the level of the FFT and if the bone is bifid to avoid incidental dural tears.
-Ensure sufficient padding of all pressure points in prone position.
-Subperiosteal dissection during muscle stripping to avoid excessive blood loss.
-Minimally invasive interlaminar approach without or only minimal laminotomy is sufficient.
-Test IONM and verify that no response is evoked before sectioning the FFT.
-Meticulous hemostasis of both ends of the fatty filum terminale to avoid intradural bleeding after cutting the FFT.
-Watertight dura closure and postoperative bedrest in horizontal position for 48 h to prevent CSF fistula.
This article is part of the Topical Collection on Pediatric Neurosurgery
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 83741 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Greuter, L., Licci, M., Terrier, A. et al. Minimal invasive interlaminar approach for untethering of fatty filum terminale in pediatric patients — how I do it. Acta Neurochir 164, 1481–1484 (2022). https://doi.org/10.1007/s00701-022-05204-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-022-05204-y