Abstract
Background
Abrupt increase of multidrug-resistant, extensively drug-resistant, and pandrug-resistant bacteria may complicate the course, management, and costs of neurocritical patients and is associated with high morbidity and mortality rates. No data exists regarding risk factors for colonization by gram-negative pathogens in neurocritical patients. The aim of the study was to identify risk factors associated with colonization by multidrug-resistant, extensively drug-resistant, and pandrug-resistant gram-negative bacteria in neurocritical patients.
Methods
We conducted a retrospective cohort study in a neurointensive care unit over a period of 3 years. We included adult neurocritical patients admitted for more than 48 h. We analyzed several factors including both anamnestic factors and admission diagnosis.
Results
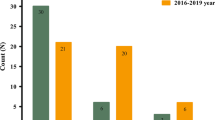
Four hundred twenty neurocritical patients were retrospectively enrolled. Seventy-three patients developed colonization by multidrug-resistant and 53 by extensively drug-resistant gram negative pathogens. Logistic regression identified intensive care unit length of stay (LOS) as the strongest predictor for both multidrug-resistant (AUC 0.877; 95% CI 0.841–0.913) and extensively drug-resistant (AUC 0.839 0.787–0.892) gram negative pathogens. In addition, external ventricular drainage and intracerebral pressure monitoring catheter were risk factors for XDR. Survival analysis revealed that MDR bacteria colonization happens earlier (log-rank test p = 0.017).
Conclusions
Optimization of healthcare strategies is required in order to reduce patients’ length of stay to prevent multi- and extensively-drug gram-negative colonizations. Indeed, an early external ventricular drainage and intracerebral pressure monitoring catheter removal is deemed necessary as soon as clinically appropriate.



Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- DM:
-
Diabetes mellitus
- EVD:
-
External ventricular drainage
- XDR:
-
Extensively drug resistant
- GCS:
-
Glasgow Coma Scale
- IMV:
-
Invasive mechanical ventilation
- ICP:
-
Intracerebral pressure
- ICU:
-
Intensive care units
- IQR:
-
Interquartile range
- LOS:
-
Length of stay
- MDR:
-
Multidrug resistant
- ORs:
-
Odds ratios
- PDR:
-
Pandrug resistant
References
Ang H, Sun X (2018) Risk factors for multidrug-resistant gram-negative bacteria infection in intensive care units: a meta-analysis. Int J Nurs Pract 24:e12644. https://doi.org/10.1111/ijn.12644
Barbier F, Andremont A, Wolff M, Bouadma L (2013) Hospital-acquired pneumonia and ventilator-associated pneumonia: recent advances in epidemiology and management. Curr Opin Pulm Med 19:216–228. https://doi.org/10.1097/MCP.0b013e32835f27be
Bouza E, Giannella M, Bunsow E et al (2012) Ventilator-associated pneumonia due to meticillin-resistant Staphylococcus aureus: risk factors and outcome in a large general hospital. J Hosp Infect 80:150–155. https://doi.org/10.1016/j.jhin.2011.11.013
Burillo A, Muñoz P, Bouza E (2019) Risk stratification for multidrug-resistant gram-negative infections in ICU patients. Curr Opin Infect Dis 32:626–637. https://doi.org/10.1097/QCO.0000000000000599
Fox J, Monette G (1992) Generalized collinearity diagnostics. Am Stat Assoc 87:178–183. https://doi.org/10.1080/01621459.1992.10475190
Geraldini F, De Cassai A, Correale C et al (2020) Predictors of deep-vein thrombosis in subarachnoid hemorrhage: a retrospective analysis. Acta Neurochir 162:2295–2301. https://doi.org/10.1007/s00701-020-04455-x
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332. https://doi.org/10.1016/j.ajic.2008.03.002
Liu P, Li X, Luo M et al (2018) Risk factors for carbapenem-resistant Klebsiella pneumoniae infection: a meta-analysis. Microb Drug Resist 24:190–198. https://doi.org/10.1186/s13756-020-0686-0
Magiorakos AP, Srinivasan A, Carey RB et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
Raymond B (2019) Five rules for resistance management in the antibiotic apocalypse, a road map for integrated microbial management. Evol Appl 12:1079–1091. https://doi.org/10.1111/eva.12808
Singer M, Deutschman CS, Seymour CW et al (2016) The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 315(8):801–810. https://doi.org/10.1001/jama.2016.0287
Topjian AA, Stuart A, Pabalan AA et al (2014) Risk factors associated with infections and need for permanent cerebrospinal fluid diversion in pediatric intensive care patients with externalized ventricular drains. Neurocrit Care 21:294–299. https://doi.org/10.1007/s12028-013-9946-7
Vasudevan A, Memon BI, Mukhopadhyay A, Li J, Tambyah PA (2015) The costs of nosocomial resistant gram negative intensive care unit infections among patients with the systemic inflammatory response syndrome- a propensity matched case control study. Antimicrob Resist Infect Control 4:3. https://doi.org/10.1186/s13756-015-0045-8
Wenzel RR, Thompson RL, Landry SM et al (1983) Hospital-acquired infections in intensive care unit patients: an overview with emphasis on epidemics. Infect Control 4:371–375. https://doi.org/10.1017/s0195941700059774
Wistrand-Yuen E, Knopp M, Hjort K, Koskiniemi S, Berg OG, Andersson DI (2018) Evolution of high-level resistance during low-level antibiotic exposure. Nat Commun 9:1599. https://doi.org/10.1038/s41467-018-04059-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. All persons gave their informed consent prior to their inclusion in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Infection
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Munari, M., Franzoi, F., Sergi, M. et al. Extensively drug-resistant and multidrug-resistant gram-negative pathogens in the neurocritical intensive care unit. Acta Neurochir 164, 859–865 (2022). https://doi.org/10.1007/s00701-020-04611-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04611-3