Abstract
Purpose
Endoscopic endonasal skull base surgery (EESBS) is a clean-contaminated procedure. Guidelines regarding the antibiotic prophylaxis in EESBS have not been developed yet, and today, there are no universally accepted protocols. In this article, we investigated the efficacy of our new ultra-short antibiotic prophylaxis protocol for EESBS guided by the cultural results of preoperative microbiological nasal swabs.
Methods
We defined as “nasal swab-related antibiotic protocol” the administration of a first-generation cephalosporin (cefazolin 2 g) in patients whose nasal swabs revealed the presence of normal nasal flora or methicillin-sensitive Staphylococcus aureus (MSSA), and the administration of vancomycin 1 g intravenously in patients whose nasal swabs revealed the presence of methicillin-resistant Staphylococcus aureus (MRSA) or with reported cephalosporin/penicillin allergy. This case-control study included 120 patients who underwent EESBS. The case group included 60 cases who received the “nasal swab-related antibiotic protocol,” while the control group included 60 cases who received the “standard hospital antibiotic protocol” used in neurosurgery (cefazolin 2 g plus metronidazole 500 mg at induction, and 2 g of cefazolin repeated after 180 min).
Results
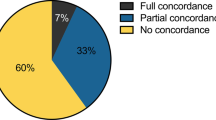
The preoperative microbiological nasal swabs showed normal nasal flora in 42 patients (70%), MSSA in 17 patients (28.3%), and MRSA in 1 patient (1.6%). During the study period, no cases of meningitis or sinusitis occurred in the case group (“nasal swab-related antibiotic protocol”), while two infections (3.3%, 1 sinusitis and 1 meningitis) were reported in the control group (“standard hospital antibiotic protocol”). Mean length of hospitalization was 6.5 days for the case group and 8.5 days in the control group. “Standard hospital antibiotic protocol” is less expensive (range, 2.88–5.42 euros) compared with our new “nasal swab-related antibiotic protocol” (range, 10.02–32.56 euros), but in line with other antibiotic prophylaxis protocols reported in literature.
Discussion
The low complication rates of our case series (0%) is comparable to complication rates reported in literature (1.6% for meningitis and 8% for sinusitis). Compared with other perioperative antibiotic regimens reported in literature, the “nasal swab-related antibiotic protocol” is cheap and at least equally effective. We discuss the rationale on which we based the choice of chemoprophylaxis, the timing, and the length of our regimen.
Conclusions
Our study confirmed the safety and efficacy of our easily applicable and low-cost antibiotic prophylaxis protocol.


Similar content being viewed by others
Abbreviations
- CSF:
-
Cerebrospinal fluid
- EESBS:
-
Endoscopic endonasal skull base surgery
- FSS:
-
Functional sinus surgery
- NSF:
-
Nasoseptal flap
- MDR:
-
Multidrug resistance
- MRI:
-
Magnetic resonance imaging
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MSSA:
-
Methicillin-sensitive Staphylococcus aureus
- SSIs:
-
Surgical site infections
References
Acquisto NM, Bodkin RP, Brown JE, Graman PS, Jones CMC, Li T, Hardy DJ, Dodds Ashley E (2018) MRSA nares swab is a more accurate predictor of MRSA wound infection compared with clinical risk factors in emergency department patients with skin and soft tissue infections. Emerg Med J 35(6):357–360
Balestrino A, Fiaschi P, Prior A, Criminelli Rossi D, Zona G (2020) Recurrent meningitis after cysto-sphenoidostomy surgery for craniopharyngioma healed with removal of the implanted catheter. J Neurosurg Sci. https://doi.org/10.23736/S0390-5616.18.04314-X
Bassis CM, Tang AL, Young VB, Pynnonen MA (2014) The nasal cavity microbiota of healthy adults. Microbiome 2(1):27
Beer R, Pfausler B, Schmutzhard E (2010) Infectious intracranial complications in the neuro-ICU patient population. Curr Opin Crit Care 16(2):117–122. https://doi.org/10.1097/MCC.0b013e328338cb5f
Borg A, Kirkman MA, Choi D (2016) Endoscopic endonasal anterior skull base surgery: a systematic review of complications during the past 65 years. World Neurosurg 95:383–391
Bratzler DW, Dellinger EP, Olsen KM et al (2013) Clinical practice guidelines for antimicrobial prophylaxis in surgery. Surg Infect 14(1):73–156
Brown SM, Anand VK, Tabaee A, Schwartz TH (2007) Role of perioperative antibiotics in endoscopic skull base surgery. Laryngoscope 117(9):1528–1532
Carrau RL, Snyderman C, Janecka IP, Sekhar L, Sen C, D’Amico F (1991) Antibiotic prophylaxis in cranial base surgery. Head Neck 13(4):311–317
Ceraudo M, Anania P, Prior A, Rossi DC, Zona G (2019) Modified endoscopic diving technique without the traditional irrigation system in endoscopic cranial base surgery: technical note. World Neurosurg 127:146–149
Cruse PJE, Foord R (1980) The epidemiology of wound infection: a 10-year prospective study of 62,939 wounds. Surg Clin N Am 60(1):27–40
David MZ, Daum RS (2017) Treatment of Staphylococcus aureus infections. In: Bagnoli F, Rappuoli R, Grandi G (eds) Staphylococcus aureus. Springer International Publishing, Cham, pp 325–383
Donath A, Sindwani R (2006) Frontal sinus cranialization using the pericranial flap: an added layer of protection. Laryngoscope 116(9):1585–1588
Drinka P, Niederman MS, El-Solh AA, Crnich CJ (2011) Assessment of risk factors for multi-drug resistant organisms to guide empiric antibiotic selection in long term care: a dilemma. J Am Med Dir Assoc 12(5):321–325
Fang CH, Hawn VS, Agarwal V, Moskowitz HS, Kshettry VR, McKean EL, Bellile E, Akbar NA, Abuzeid WM (2019) Antibiotic prophylaxis in anterior skull-base surgery: a survey of the North American Skull Base Society. Int Forum Allergy Rhinol 9(10):1196–1204
Fiaschi P, Prior A, Ceraudo M, Zona G, Criminelli Rossi D (2020) Use of 4K resolution in endoscopic endonasal neurosurgery. J Neurosurg Sci. https://doi.org/10.23736/S0390-5616.18.04329-1
Friedman JA, Ebersold MJ, Quast LM (2000) Persistent posttraumatic cerebrospinal fluid leakage. FOC 9(1):1–5
Gabriel PJ, Kohli G, Hsueh WD, Eloy JA, Liu JK (2020) Efficacy of simultaneous pericranial and nasoseptal “double flap” reconstruction of anterior skull base defects after combined transbasal and endoscopic endonasal approaches. Acta Neurochir 162(3):641–647
Gok A, Erkutlu I, Alptekin M, Kanlikama M (2004) Three-layer reconstruction with fascia lata and vascularized pericranium for anterior skull base defects. Acta Neurochir 146(1):53–57
Gritzfeld JF, Roberts P, Roche L, El Batrawy S, Gordon SB (2011) Comparison between nasopharyngeal swab and nasal wash, using culture and PCR, in the detection of potential respiratory pathogens. BMC Res Notes 4:122
Ivan ME, Bryan Iorgulescu J, El-Sayed I, McDermott MW, Parsa AT, Pletcher SD, Jahangiri A, Wagner J, Aghi MK (2015) Risk factors for postoperative cerebrospinal fluid leak and meningitis after expanded endoscopic endonasal surgery. J Clin Neurosci 22(1):48–54
Johans SJ, Burkett DJ, Swong KN, Patel CR, Germanwala AV (2018) Antibiotic prophylaxis and infection prevention for endoscopic endonasal skull base surgery: our protocol, results, and review of the literature. J Clin Neurosci 47:249–253
Kluytmans J, van Belkum A, Verbrugh H (1997) Nasal carriage of Staphylococcus aureus: epidemiology, underlying mechanisms, and associated risks. Clin Microbiol Rev 10(3):505–520
Kono Y, Prevedello DM, Snyderman CH, Gardner PA, Kassam AB, Carrau RL, Byers KE (2011) One thousand endoscopic skull base surgical procedures demystifying the infection potential: incidence and description of postoperative meningitis and brain abscesses. Infect Control Hosp Epidemiol 32(1):77–83
Little AS, White WL (2011) Prophylactic antibiotic trends in transsphenoidal surgery for pituitary lesions. Pituitary 14(2):99–104
Little AS, White WL (2011) Short-duration, single-agent antibiotic prophylaxis for meningitis in trans-sphenoidal surgery. Pituitary 14(4):335–339
Locatelli D, Balbi S, Veiceschi P (2020) The endoscopic diving technique in endonasal transsphenoidal surgery: how I do it. Acta Neurochir. https://doi.org/10.1007/s00701-020-04369-8
Milanese L, Zoli M, Sollini G, Martone C, Zenesini C, Sturiale C, Farneti P, Frank G, Pasquini E, Mazzatenta D (2017) Antibiotic prophylaxis in endoscopic endonasal pituitary and skull base surgery. World Neurosurg 106:912–918
Moldovan ID, Agbi C, Kilty S, Alkherayf F (2019) A systematic review of prophylactic antibiotic use in endoscopic endonasal transsphenoidal surgery for pituitary lesions. World Neurosurg 128:408–414
Naik BI, Roger C, Ikeda K, Todorovic MS, Wallis SC, Lipman J, Roberts JA (2017) Comparative total and unbound pharmacokinetics of cefazolin administered by bolus versus continuous infusion in patients undergoing major surgery: a randomized controlled trial. Br J Anaesth 118(6):876–882
Orlando R, Cappabianca P, Tosone G, Esposito F, Piazza M, de Divitiis E (2007) Retrospective analysis of a new antibiotic chemoprophylaxis regimen in 170 patients undergoing endoscopic endonasal transsphenoidal surgery. Surg Neurol 68(2):145–148
Pagliano P, Caggiano C, Ascione T, Solari D, Di Flumeri G, Cavallo LM, Tortora F, Cappabianca P (2017) Characteristics of meningitis following transsphenoidal endoscopic surgery: a case series and a systematic literature review. Infection 45(6):841–848
Patel PN, Jayawardena ADL, Walden RL, Penn EB, Francis DO (2018) Evidence-based use of perioperative antibiotics in otolaryngology. Otolaryngol Head Neck Surg 158(5):783–800
Rosen SAB, Getz AE, Kingdom T, Youssef AS, Ramakrishnan VR (2016) Systematic review of the effectiveness of perioperative prophylactic antibiotics for skull base surgeries. Am J Rhinol Allergy 30(2):e10–e16
Rudmik L, Soler ZM, Orlandi RR, Stewart MG, Bhattacharyya N, Kennedy DW, Smith TL (2011) Early postoperative care following endoscopic sinus surgery: an evidence-based review with recommendations. Int Forum Allergy Rhinol 1(6):417–430
Schenck LP, Surette MG, Bowdish DME (2016) Composition and immunological significance of the upper respiratory tract microbiota. FEBS Lett 590(21):3705–3720
Shibao S, Toda M, Tomita T, Ogawa K, Yoshida K (2014) Analysis of the bacterial flora in the nasal cavity and the sphenoid sinus mucosa in patients operated on with an endoscopic endonasal transsphenoidal approach. Neurol Med Chir(Tokyo) 54(12):1009–1013
Smith EJ, Stringer S (2014) Current perioperative practice patterns for minimizing surgical site infection during rhinologic procedures: perioperative practice patterns to minimize SSIs. Int Forum Allergy Rhinol 4(12):1002–1007
Somma T, Maraolo AE, Esposito F, Cavallo LM, Tosone G, Orlando R, Cappabianca P (2015) Efficacy of ultra-short single agent regimen antibiotic chemo-prophylaxis in reducing the risk of meningitis in patients undergoing endoscopic endonasal transsphenoidal surgery. Clin Neurol Neurosurg 139:206–209
Thorp BD, Sreenath SB, Ebert CS, M.P.H, Zanation AM (2014) Endoscopic skull base reconstruction: a review and clinical case series of 152 vascularized flaps used for surgical skull base defects in the setting of intraoperative cerebrospinal fluid leak. FOC 37(4):E4
Tseng W-P, Chen Y-C, Yang B-J, Chen S-Y, Lin J-J, Huang Y-H, Fu C-M, Chang S-C, Chen S-Y (2017) Predicting multidrug-resistant Gram-negative bacterial colonization and associated infection on hospital admission. Infect Control Hosp Epidemiol 38(10):1216–1225
Van de Beek D, Drake JM, Tunkel AR (2010) Nosocomial bacterial meningitis. N Engl J Med 362(2):146–154
Zanation AM, Carrau RL, Snyderman CH, Germanwala AV, Gardner PA, Prevedello DM, Kassam AB (2009) Nasoseptal flap reconstruction of high flow intraoperative cerebral spinal fluid leaks during endoscopic skull base surgery. Am J Rhinol Allergy 23(5):518–521
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This is a retrospective observational study. No ethical approval is required.
Informed consent
Informed patient consent is not required for the present paper. No data from which individual can be identified are present in the manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pituitaries
Rights and permissions
About this article
Cite this article
Ceraudo, M., Prior, A., Balestrino, A. et al. Ultra-short antibiotic prophylaxis guided by preoperative microbiological nasal swabs in endoscopic endonasal skull base surgery. Acta Neurochir 163, 369–382 (2021). https://doi.org/10.1007/s00701-020-04560-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-020-04560-x