Abstract
Introduction
Intracranial infection is often associated with contiguous sinus infection, with Streptococcus intermedius being the most common pathogen. Microbiological assessment is possible via sinus or intracranial sampling. While a sinus approach is minimally invasive, it is not clear whether this yields definitive microbiological diagnosis leading to optimized antimicrobial therapy and avoidance of intracranial surgery.
Methods
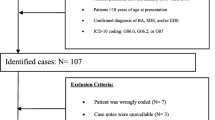
A retrospective review of a prospectively collected electronic departmental database identified patients between 2019 and 2022. Further demographic and microbiological information was obtained from electronic patient records and laboratory management systems.
Results
Thirty-one patients were identified with intracranial subdural and/or epidural empyema and concurrent sinus involvement during the 3-year study period. The median age of onset was 10 years with a slight male predominance (55%). All patients had intracranial sampling with 15 patients undergoing sinus sampling in addition. Only 1 patient (7%) demonstrated identical organism(s) grown from both samples. Streptococcus intermedius was the most common pathogen in intracranial samples. Thirteen patients (42%) had mixed organisms from their intracranial cultures and 57% of samples undergoing bacterial PCR identified additional organisms, predominantly anaerobes. Sinus samples had a significant addition of nasal flora and Staphylococcus aureus which was rarely grown from intracranial samples. Of concern, 7/14 (50%) of sinus samples did not identify the main intracranial pathogen diagnosed on intracranial culture and additional PCR. Literature review identified 21 studies where sinus drainage was used to treat intracranial empyemas, with only 6 authors reporting concurrent microbiology results. This confirmed our cohort to be the largest comparative study in the current literature. No center has observed a greater than 50% concordance in microbiological diagnoses.
Conclusion
Endoscopic sinus surgery may have therapeutic benefit, but it is not an appropriate approach for microbiological diagnosis in pediatric subdural empyemas. High rates of contaminating nasal flora can lead to misdiagnosis and inappropriate treatment. Routine addition of 16S rRNA PCR to intracranial samples is recommended.




Similar content being viewed by others
References
Blumfield E, Misra M (2011) Pott’s puffy tumor, intracranial, and orbital complications as the initial presentation of sinusitis in healthy adolescents, a case series. Emerg Radiol 18(3):203–210. https://doi.org/10.1007/s10140-010-0934-3
Wald ER, Applegate KE, Bordley C et al (2013) Clinical practice guideline for the diagnosis and management of acute bacterial sinusitis in children aged 1 to 18 years. Pediatrics 132(1):e262-280. https://doi.org/10.1542/peds.2013-1071
Fokkens WJ, Lund VJ, Hopkins C et al (2020) European position paper on rhinosinusitis and nasal polyps 2020. Rhinology 58(Suppl S29):1–464. https://doi.org/10.4193/Rhin20.600
Adibelli ZH, Songu M, Adibelli H (2011) Paranasal sinus development in children: a magnetic resonance imaging analysis. Am J Rhinol Allergy 25(1):30–35. https://doi.org/10.2500/ajra.2011.25.3552
Hakim HE, Malik AC, Aronyk K, Ledi E, Bhargava R (2006) The prevalence of intracranial complications in pediatric frontal sinusitis. Int J Pediatr Otorhinolaryngol 70(8):1383–1387. https://doi.org/10.1016/j.ijporl.2006.02.003
Muzumdar D, Jhawar S, Goel A (2011) Brain abscess: an overview. Int J Surg 9(2):136–144. https://doi.org/10.1016/j.ijsu.2010.11.005
McNeil JC, Dunn JJ, Kaplan SL, Vallejo JG (2020) Complications of otitis media and sinusitis caused by Streptococcus anginosus group organisms in children. Pediatr Infect Dis J 39(2):108–113. https://doi.org/10.1097/INF.0000000000002514
Tandon S, Beasley N, Swift AC (2009) Changing trends in intracranial abscesses secondary to ear and sinus disease. J Laryngol Otol 123(3):283–288. https://doi.org/10.1017/S002221510800234X
Patel NA, Garber D, Hu S, Kamat A (2016) Systematic review and case report: intracranial complications of pediatric sinusitis. Int J Pediatr Otorhinolaryngol 86:200–212. https://doi.org/10.1016/j.ijporl.2016.05.009
Bockova J, Rigamonti D (2000) Intracranial empyema. Pediatr Infect Dis J 19(8):735–737. https://doi.org/10.1097/00006454-200008000-00012
Brook I (2009) Microbiology and antimicrobial treatment of orbital and intracranial complications of sinusitis in children and their management. Int J Pediatr Otorhinolaryngol 73(9):1183–1186. https://doi.org/10.1016/j.ijporl.2009.01.020
Heilpern KL, Lorber B (1996) Focal intracranial infections. Infect Dis Clin North Am 10(4):879–898. https://doi.org/10.1016/s0891-5520(05)70331-7
Dill SR, Cobbs CG, McDonald CK (1995) Subdural empyema: analysis of 32 cases and review. Clin Infect Dis 20(2):372–386. https://doi.org/10.1093/clinids/20.2.372
Rasul FT, Chari A, Iqbal MO et al (2022) The case for early antibiotic commencement and source control in paediatric subdural empyema: a single-centre retrospective case series. Pediatr Neurosurg 57(1):28–34. https://doi.org/10.1159/000521038
Yogev R, Bar-Meir M (2004) Management of brain abscesses in children. Pediatr Infect Dis J 23(2):157–159. https://doi.org/10.1097/01.inf.0000110272.67271.a2
Younis RT, Lazar RH, Anand VK (2002) Intracranial complications of sinusitis: a 15-year review of 39 cases. Ear Nose Throat J 81(9):636–638, 640–642, 644
Maniglia AJ, Goodwin WJ, Arnold JE, Ganz E (1989) Intracranial abscesses secondary to nasal, sinus, and orbital infections in adults and children. Arch Otolaryngol Head Neck Surg 115(12):1424–1429. https://doi.org/10.1001/archotol.1989.01860360026011
Herrmann BW, Forsen JW Jr (2004) Simultaneous intracranial and orbital complications of acute rhinosinusitis in children. Int J Pediatr Otorhinolaryngol 68(5):619–625. https://doi.org/10.1016/j.ijporl.2003.12.010
Reynolds DJ, Kodsi SR, Rubin SE, Rodgers IR (2003) Intracranial infection associated with preseptal and orbital cellulitis in the pediatric patient. J AAPOS 7(6):413–417. https://doi.org/10.1016/j.jaapos.2003.09.013
Oxford LE, McClay J (2005) Complications of acute sinusitis in children. Otolaryngol Head Neck Surg 133(1):32–37. https://doi.org/10.1016/j.otohns.2005.03.020
Goodkin HP, Harper MB, Pomeroy SL (2004) Intracerebral abscess in children: historical trends at Children’s Hospital Boston. Pediatrics 113(6):1765–1770. https://doi.org/10.1542/peds.113.6.1765
Bair-Merritt MH, Shah SS, Zaoutis TE, Bell LM, Feudtner C (2005) Suppurative intracranial complications of sinusitis in previously healthy children. Pediatr Infect Dis J 24(4):384–386. https://doi.org/10.1097/01.inf.0000160589.40857.ad
Marques da Silva R, Caugant DA, Josefsen R, Tronstad L, Olsen I (2004) Characterization of Streptococcus constellatus strains recovered from a brain abscess and periodontal pockets in an immunocompromised patient. J Periodontol 75(12):1720–1723. https://doi.org/10.1902/jop.2004.75.12.1720
Young M, Putty M, Schaible K (2018) Spontaneous intraventricular tension pneumocephalus: case report and review of the literature. World Neurosurg 114:317–322. https://doi.org/10.1016/j.wneu.2018.03.076
Al Majid F, Aldrees A, Barry M, Binkhamis K, Allam A, Almohaya A (2020) Streptococcus anginosus group infections: management and outcome at a tertiary care hospital. J Infect Public Health 13(11):1749–1754. https://doi.org/10.1016/j.jiph.2020.07.017
Issa E, Salloum T, Tokajian S (2020) From normal flora to brain abscesses: a review of Streptococcus intermedius. Front Microbiol 11:826. https://doi.org/10.3389/fmicb.2020.00826
Kuczkowski J, Narozny W, Mikaszewski B, Stankiewicz C (2005) Suppurative complications of frontal sinusitis in children. Clin Pediatr (Phila) 44(8):675–682. https://doi.org/10.1177/000992280504400805
Ong YK, Tan HKK (2002) Suppurative intracranial complications of sinusitis in children. Int J Pediatr Otorhinolaryngol 66(1):49. https://doi.org/10.1016/s0165-5876(02)00209-4
Rosenfeld EA, Rowley AH (1994) Infectious intracranial complications of sinusitis, other than meningitis, in children: 12-year review. Clin Infect Dis 18(5):750–754. https://doi.org/10.1093/clinids/18.5.750
Johnson DL, Markle BM, Wiedermann BL, Hanahan L (1988) Treatment of intracranial abscesses associated with sinusitis in children and adolescents. J Pediatr 113(1 Pt 1):15–23. https://doi.org/10.1016/s0022-3476(88)80522-5
Wenig BL, Goldstein MN, Abramson AL (1983) Frontal sinusitis and its intracranial complications. Int J Pediatr Otorhinolaryngol 5(3):285–302. https://doi.org/10.1016/s0165-5876(83)80042-1. PMID: 6629657
Acknowledgements
We would like to acknowledge all of the children, parents, and health care workers who were involved in the care of the children in this cohort without whom the project would not have been possible.
Author information
Authors and Affiliations
Contributions
JH conceived the project with data extraction completed by MKS, JH, MM, and L-AB. The manuscript was written by MKS and JH with critical revisions by MKS, JH, MT, JH, KA, GJ, DT, OJ, ADHS, and MZT. The project was supervised by JH and ZT.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no financial nor non-financial competing interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kameda-Smith, M.M., Mendoza, M., Brown, LA. et al. Comparison of endoscopic sinus sampling versus intracranial sampling for microbiological diagnosis of intracranial infection in children: a case series and literature review. Childs Nerv Syst 39, 3561–3570 (2023). https://doi.org/10.1007/s00381-023-06038-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06038-4