Abstract
Background
A variety of surgical techniques can be used to achieve lumbar spinal fusion for management of degenerative conditions. Transforaminal lumbar interbody fusion (TLIF) is the most popular technique; however, midline lumbar interbody fusion (MIDLIF) is a valid alternative to the more traditional pedicle screw trajectory with potential advantages. The aim of this study is to evaluate the clinical outcomes from a cohort of patients submitted to MIDLIF in a single hospital during the surgical team’s initial learning period.
Methods
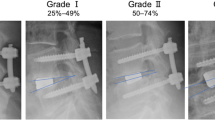
The first 30 consecutive patients who underwent single- or two-level MIDLIF surgery for lumbar degenerative disease were included in this retrospective study. Patients’ demographics, surgical data, length of hospitalisation, and perioperative complications were analysed. Preoperative and postoperative radiographic parameters were obtained. Validated questionnaires, Core Outcome Measure Index for the back, Euro-QoL 5-Dimensional Questionnaire, and Oswestry Disability Index, were used for clinical assessment.
Results
Mean surgery time was 278.53 ± 82.16 min and mean hospitalisation time was 6.17 ± 3.51 days. Six patients experienced complications, four of which being dural tears with no consequences, and two required reoperations during the mean follow-up of 25.23 ± 9.74 months. Preoperative and postoperative radiological parameters did not demonstrate significant differences. All clinical parameters significantly improved after surgery (p < 0.001). A complexity score was developed to more accurately compare the different procedures, and it strongly correlated with surgery duration (r = 0.719, p < 0.001). Furthermore, a moderate correlation was found between a developed Duration Index and the patient’s order number (r = − 0.539, p = 0.002).
Conclusions
In our initial experience, MIDLIF showed to be effective in significantly improving the patients’ functional status, pain scores, and quality of life. The technique seems safe, with an acceptably low complication rate. Hence, MIDLIF can be considered as a promising alternative to more traditional TLIF and PLIF techniques even at the beginning of the learning curve.

Similar content being viewed by others
References
Bielecki M, Kunert P, Prokopienko M, Nowak A, Czernicki T, Marchel A (2016) Midline lumbar fusion using cortical bone trajectory screws. Preliminary report. Videosurgery Miniinv 3:156–163
Bosacco SJ, Gardner MJ, Guille JT (2001) Evaluation and treatment of dural tears in lumbar spine surgery: a review. Clin Orthop Relat Res 389:238–247
Copay AG, Glassman SD, Subach BR, Berven S, Schuler TC, Carreon LY (2008) Minimum clinically important difference in lumbar spine surgery patients: a choice of methods using the Oswestry Disability Index, Medical Outcomes Study questionnaire Short Form 36, and Pain Scales. Spine J 8(6):968–974
Dabbous B, Brown D, Tsitlakidis A, Arzoglou V (2016) Clinical outcomes during the learning curve of MIDline Lumbar Fusion (MIDLF®) using the cortical bone trajectory. Acta Neurochir 158(7):1413–1420
Damasceno LHF, Rocha PAG, Barbosa ES, Barros CAM, Canto FT, Defino HLA, Mannion AF (2012) Cross-cultural adaptation and assessment of the reliability and validity of the Core Outcome Measures Index (COMI) for the Brazilian-Portuguese language. Eur Spine J 21(7):1273–1282
Elmekaty M, Kotani Y, El Mehy E, Robinson Y, El Tantawy A, Sekiguchi I, Fujita R (2018) Clinical and radiological comparison between three different minimally invasive surgical fusion techniques for single-level lumbar isthmic and degenerative spondylolisthesis: Minimally invasive surgical posterolateral fusion versus minimally invasive surgical transforaminal lumbar interbody fusion versus midline lumbar fusion. Asian Spine J 12(5):870–879
Fairbank JC, Pynsent PB (2000) The Oswestry Disability Index. Spine 25(22):2940–2952
Huang HM, Chen CH, Lee HC, Chuang HY, Chen DC, Chu YT, Cho DY (2018) Minimal invasive surgical technique in midline lumbar inter-body fusion: a technique note. J Clin Neurosci 55:103–108
Lan T, Hu SY, Zhang YT, Zheng YC, Zhang R, Shen Z, Yang XJ (2018) Comparison between posterior lumbar interbody fusion and transforaminal lumbar interbody fusion for the treatment of lumbar degenerative diseases: a systematic review and meta-analysis. World Neurosurg 112:86–93
Lee CS, Eoh W, Chung SS, Lee SH, Kim ES, Kim MK (2011) The impact of sagittal balance on clinical results after posterior interbody fusion for patients with degenerative spondylolisthesis: a pilot study. BMC Musculoskelet Disord 12(1)
Lee JC, Jang HD, Shin BJ (2012) Learning curve and clinical outcomes of minimally invasive transforaminal lumbar interbody fusion: Our experience in 86 consecutive cases. Spine 37(18):1548–1557
Maeng DH, Min JH, Lee SH, Jang JS, Kim JM, Han KM (2009) Can patients with sagittally well-compensated lumbar degenerative kyphosis benefit from surgical treatment for intractable back pain? Neurosurg 64(1):115–121
Mannion AF, Vila-Casademunt A, Domingo-Sàbat M, Wunderlin S, Pellisé F, Bago J et al (2016) The Core Outcome Measures Index (COMI) is a responsive instrument for assessing the outcome of treatment for adult spinal deformity. Eur Spine J 25(8):2638–2648
Miller JA, Derakhshan A, Lubelski D, Alvin MD, McGirt MJ, Benzel EC, Mroz TE (2015) The impact of pre-operative depression on quality of life outcomes after lumbar surgery. Spine J 15(1):58–64
Mizuno M, Kuraishi K, Umeda Y, Sano T, Tsuji M, Suzuki H (2014) Midline lumbar fusion with cortical bone trajectory screw. Neurol Med-Chir 54(9):716–721
Phillips JT (2017) Comparing mid lumbar interbody fusion (MIDLF) with traditional posterior lumbar interbody fusion (PLIF). Electronic Thesis And Dissertation Repository, 4541
Rodriguez A, Neal MT, Liu A, Somasundaram A, Hsu W, Branch CL (2014) Novel placement of cortical bone trajectory screws in previously instrumented pedicles for adjacent-segment lumbar disease using CT image-guided navigation. Neurosurg Focus 36(3):E9
Schnake KJ, Rappert D, Storzer B, Schreyer S, Hilber F, Mehren C (2018) Lumbale Spondylodese – Indikationen und Techniken. Der Orthop:50–58
Silva PS, Silva PA, Monteiro P, Vaz R, Pereira P (2013) Learning curve and complications of minimally invasive transforaminal lumbar interbody fusion. Neurosurg Focus 35(8):E7
Smith S, Weldring T (2013) Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Services Insights 61
Solberg T, Johnsen LG, Nygaard ØP, Grotle M (2013) Can we define success criteria for lumbar disc surgery? Estimates for a substantial amount of improvement in core outcome measures. Acta Orthop 84(2):196–201
The EuroQol Group (1990) EuroQol-a new facility for the measurement of health-related quality of life. Health Policy 16(3):199–208
Tuomainen I, Pakarinen M, Aalto T, Sinikallio S, Kröger H, Viinamäki H, Airaksinen O (2018) Depression is associated with the long-term outcome of lumbar spinal stenosis surgery: a 10-year follow-up study. Spine J 18(3):458–463
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
PP has an education and training and consultancy agreement with Medtronic Sofamor Danek, USA. FS, PSS, and RV certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (Comissão de Ética para a Saúde do Centro Hospitalar Universitário de São João) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Spine degenerative
Rights and permissions
About this article
Cite this article
Silva, F., Silva, P.S., Vaz, R. et al. Midline lumbar interbody fusion (MIDLIF) with cortical screws: initial experience and learning curve. Acta Neurochir 161, 2415–2420 (2019). https://doi.org/10.1007/s00701-019-04079-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04079-w