Abstract
Background
Gravitational shunt valves and most recently the adjustable proSA® gravitational valve have been designed to counteract overdrainage and thereby improving clinical outcome. So far, the applicability in a broader mix of hydrocephalus patients is unrevealed. The aim of this study was to evaluate the utility of gravitational valves in two different clinical settings.
Methods
This retrospective double-center cohort study was enabled by two different shunt management policies. At Rigshospitalet, patients with a complicated shunt history receiving a proGAV® and proSA® shunt system during surgical revision were included, and clinical outcome in the follow-up periods before and after was compared. At Aarhus University Hospital, a combination of a proGAV® and a fixed (SA®) or adjustable (proSA®) gravitational valve was used in all shunt procedures. Clinical outcome in a 2-year follow-up period was compared to a cohort receiving non-gravitational valves in the period before the transition to gravitational valves.
Results
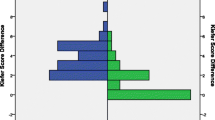
Twenty-two patients were included at Rigshospitalet. Mean follow-up time before and after proGAV® and proSA® implantation was 2.3 and 1.5 years, respectively. In each patient, roughly two surgical revisions (p 0.031) and two hospitalizations (p 0.009) were avoided each year after proGAV® and proSA® implantation. At Aarhus University Hospital, 90 patients with non-gravitational valves and 98 patients with gravitational valves were included. Changes in clinical outcome parameters and shunt survivals were either stable or statistically insignificant.
Conclusions
Gravitational valves are safe and useful in clinical practice and represent an equivalent alternative as a first-line shunt valve in a broad mix of patients, while proSA® valves should be considered for complex shunt patients.



Similar content being viewed by others
References
Allin DM, Czosnyka ZH, Czosnyka M, Richards HK, Pickard JD (2006) In vitro hydrodynamic properties of the Miethke ProGAV hydrocephalus shunt. Cerebrospinal Fluid Res 3:9. https://doi.org/10.1186/1743-8454-3-9
Baird LC, Mazzola CA, Auguste KI, Klimo P Jr, Flannery AM (2014) Pediatric hydrocephalus: systematic literature review and evidence-based guidelines. Part 5: effect of valve type on cerebrospinal fluid shunt efficacy. J Neurosurg Pediatr 14(Suppl 1):35–43. https://doi.org/10.3171/2014.7.peds14325
Czosnyka M, Czosnyka Z, Pickard JD (2012) Programmable shunt assistant tested in Cambridge shunt evaluation laboratory. Acta Neurochir Suppl 113:71–76. https://doi.org/10.1007/978-3-7091-0923-6_15
Czosnyka Z, Cieslicki K, Richards HK, Pickard JD, Czosnyka M (2014) Hydrocephalus shunts: principles, hardware, shunt testing. In: Rigamonti D (ed) Adult hydrocephalus. Cambridge University Press, Cambridge, pp 190–206. https://doi.org/10.1017/CBO9781139382816.018.
Czosnyka Z, Czosnyka M, Richards HK, Pickard JD (1998) Posture-related overdrainage: comparison of the performance of 10 hydrocephalus shunts in vitro. Neurosurgery 42:327–333 discussion 333-324
Fox JL, McCullough DC, Green RC (1973) Effect of cerebrospinal fluid shunts on intracranial pressure and on cerebrospinal fluid dynamics. 2. A new technique of pressure measurements: results and concepts. 3. A concept of hydrocephalus. J Neurol Neurosurg Psychiatry 36:302–312
Freimann FB, Schulz M, Haberl H, Thomale UW (2014) Feasibility of telemetric ICP-guided valve adjustments for complex shunt therapy. Child’s Nerv Syst: ChNS : Off J Int Soc Pediatr Neurosurg 30:689–697. https://doi.org/10.1007/s00381-013-2324-0
Freimann FB, Sprung C (2012) Shunting with gravitational valves—can adjustments end the era of revisions for overdrainage-related events?: clinical article. J Neurosurg 117:1197–1204. https://doi.org/10.3171/2012.8.jns1233
Kajimoto Y, Ohta T, Miyake H, Matsukawa M, Ogawa D, Nagao K, Kuroiwa T (2000) Posture-related changes in the pressure environment of the ventriculoperitoneal shunt system. J Neurosurg 93:614–617. https://doi.org/10.3171/jns.2000.93.4.0614
Kehler U, Kiefer M, Eymann R, Wagner W, Tschan CA, Langer N, Rohde V, Ludwig HC, Gliemroth J, Meier U, Lemcke J, Thomale UW, Fritsch M, Krauss JK, Mirzayan MJ, Schuhmann M, Huthmann A (2015) PROSAIKA: a prospective multicenter registry with the first programmable gravitational device for hydrocephalus shunting. Clin Neurol Neurosurg 137:132–136. https://doi.org/10.1016/j.clineuro.2015.07.002
Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F, Piatt J, Haines S, Schiff S, Cochrane D, Steinbok P, MacNeil N (2000) Long-term follow-up data from the shunt design trial. Pediatr Neurosurg 33:230–236. https://doi.org/10.1159/000055960
Khan RA, Narasimhan KL, Tewari MK, Saxena AK (2010) Role of shunts with antisiphon device in treatment of pediatric hydrocephalus. Clin Neurol Neurosurg 112:687–690. https://doi.org/10.1016/j.clineuro.2010.05.008
Kiefer M, Eymann R, Meier U (2002) Five years experience with gravitational shunts in chronic hydrocephalus of adults. Acta Neurochir 144:755–767; discussion 767. doi:https://doi.org/10.1007/s00701-002-0977-7
Kiefer M, Eymann R, Strowitzki M, Steudel WI (2005) Gravitational shunts in longstanding overt ventriculomegaly in adults. Neurosurgery 57:109–119 discussion 109-119
Kimura T, Schulz M, Shimoji K, Miyajima M, Arai H, Thomale UW (2016) In vitro performance of the fixed and adjustable gravity-assisted unit with and without motion-evidence of motion-induced flow. Acta Neurochir 158:2011–2018. https://doi.org/10.1007/s00701-016-2912-3
Kofoed Mansson P, Johansson S, Ziebell M, Juhler M (2017) Forty years of shunt surgery at Rigshospitalet, Denmark: a retrospective study comparing past and present rates and causes of revision and infection. BMJ Open 7:e013389. https://doi.org/10.1136/bmjopen-2016-013389
Kulkarni AV, Riva-Cambrin J, Butler J, Browd SR, Drake JM, Holubkov R, Kestle JR, Limbrick DD, Simon TD, Tamber MS, Wellons JC 3rd, Whitehead WE (2013) Outcomes of CSF shunting in children: comparison of hydrocephalus clinical research network cohort with historical controls: clinical article. J Neurosurg Pediatr 12:334–338. https://doi.org/10.3171/2013.7.peds12637
Lemcke J, Meier U (2010) Improved outcome in shunted iNPH with a combination of a Codman Hakim programmable valve and an Aesculap-Miethke ShuntAssistant. Central Eur Neurosurg 71:113–116. https://doi.org/10.1055/s-0029-1241179
Lemcke J, Meier U, Muller C, Fritsch MJ, Kehler U, Langer N, Kiefer M, Eymann R, Schuhmann MU, Speil A, Weber F, Remenez V, Rohde V, Ludwig HC, Stengel D (2013) Safety and efficacy of gravitational shunt valves in patients with idiopathic normal pressure hydrocephalus: a pragmatic, randomised, open label, multicentre trial (SVASONA). J Neurol Neurosurg Psychiatry 84:850–857. https://doi.org/10.1136/jnnp-2012-303936
Miyake H (2016) Shunt devices for the treatment of adult hydrocephalus: recent progress and characteristics. Neurol Med Chir 56:274–283. https://doi.org/10.2176/nmc.ra.2015-0282
Paulsen AH, Due-Tonnessen BJ, Lundar T (2017) Cerebrospinal fluid (CSF) shunting and ventriculocisternostomy (ETV) in 400 pediatric patients. Shifts in understanding, diagnostics, case-mix, and surgical management during half a century. Child’s Nerv Syst : ChNS : Off J Int Soc Pediatr Neurosurg 33:259–268. https://doi.org/10.1007/s00381-016-3281-1
Petersen LG, Petersen JC, Andresen M, Secher NH, Juhler M (2016) Postural influence on intracranial and cerebral perfusion pressure in ambulatory neurosurgical patients. American journal of physiology regulatory, integrative and comparative. Physiology 310:R100–R104. https://doi.org/10.1111/ane.12541 10.1152/ajpregu.00302.2015
Pollack IF, Albright AL, Adelson PD (1999) A randomized, controlled study of a programmable shunt valve versus a conventional valve for patients with hydrocephalus. Hakim-Medos Investigator Group Neurosurg 45:1399–1408 discussion 1408-1311
Rohde V, Haberl EJ, Ludwig H, Thomale UW (2009) First experiences with an adjustable gravitational valve in childhood hydrocephalus. J Neurosurg Pediatr 3:90–93. https://doi.org/10.3171/2008.11.peds08154
Sprung C, Schlosser HG, Lemcke J, Meier U, Messing-Junger M, Trost HA, Weber F, Schul C, Rohde V, Ludwig HC, Hopfner J, Sepehrnia A, Mirzayan MJ, Krauss JK (2010) The adjustable proGAV shunt: a prospective safety and reliability multicenter study. Neurosurgery 66:465–474. https://doi.org/10.1227/01.neu.0000365272.77634.6b
Stein SC, Guo W (2008) Have we made progress in preventing shunt failure? A critical analysis. J Neurosurg Pediatr 1:40–47. https://doi.org/10.3171/ped-08/01/040
Thomale UW, Gebert AF, Haberl H, Schulz M (2013) Shunt survival rates by using the adjustable differential pressure valve combined with a gravitational unit (proGAV) in pediatric neurosurgery. Child’s Nerv Syst: ChNS : Off J Int Soc Pediatr Neurosurg 29:425–431. https://doi.org/10.1007/s00381-012-1956-9
Tschan CA, Antes S, Huthmann A, Vulcu S, Oertel J, Wagner W (2014) Overcoming CSF overdrainage with the adjustable gravitational valve proSA. Acta Neurochir 156:767–776; discussion 776. https://doi.org/10.1007/s00701-013-1934-3
Weinzierl MR, Hans FJ, Stoffel M, Oertel MF, Korinth MC (2012) Experience with a gravitational valve in the management of symptomatic overdrainage in children with shunts. J Neurosurg Pediatr 9:468–472. https://doi.org/10.3171/2012.1.peds11110
Wong JM, Ziewacz JE, Ho AL, Panchmatia JR, Bader AM, Garton HJ, Laws ER, Gawande AA (2012) Patterns in neurosurgical adverse events: cerebrospinal fluid shunt surgery. Neurosurg Focus 33:E13. https://doi.org/10.3171/2012.7.focus12179
Zachenhofer I, Donat M, Roessler K (2012) The combination of a programmable valve and a subclavicular anti-gravity device in hydrocephalus patients at high risk for hygromas. Neurol Res 34:219–222. https://doi.org/10.1179/1743132811y.0000000079
Ziebell M, Wetterslev J, Tisell M, Gluud C, Juhler M (2013) Flow-regulated versus differential pressure-regulated shunt valves for adult patients with normal pressure hydrocephalus. The Cochrane database of systematic reviews:Cd009706. doi:https://doi.org/10.1002/14651858.CD009706.pub2
Funding
The Lundbeck Foundation provided financial support in the form of a scholarship for a total of 140.000 DKK to the first author.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Månsson, P.K., Hansen, T.S. & Juhler, M. The applicability of fixed and adjustable gravitational shunt valves in two different clinical settings. Acta Neurochir 160, 1415–1423 (2018). https://doi.org/10.1007/s00701-018-3568-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3568-y