Abstract
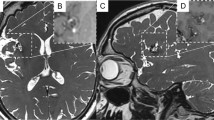
We report a case of a 50-year-old woman whose 0.5 mm middle cerebral artery (MCA) aneurysm was treated with gauze wrapping at an outside facility. She returned 9 months later with seizures and an inflammatory process in the region of the prior aneurysm. Surgical re-exploration at that time was aborted. Two years later, she presented with a gauzoma associated with local inflammatory response and severe narrowing of the MCA. A common carotid artery to MCA bypass was performed, followed by surgical removal of the gauze and inflammatory material. Over a 3-month period, she recovered with significant improvement in her preoperative neurological deficits.





Similar content being viewed by others
Abbreviations
- MCA:
-
middle cerebral artery
- PCommA:
-
left posterior communicating artery
- MRI:
-
magnetic resonance imaging
- STA:
-
superior temporal artery
- CCA:
-
common carotid artery
- CT:
-
computed tomography
- FLAIR:
-
fluid-attenuated inversion recovery
- ICA:
-
internal carotid artery
References
Andres RH, Guzman R, Weis J, Schroth G, Barth A (2007) Granuloma formation and occlusion of an unruptured aneurysm after wrapping. Acta Neurochir 149:953–958; discussion 958. https://doi.org/10.1007/s00701-007-1260-8
Beitzke M, Leber KA, Deutschmann H, Gattringer T, Poltrum B, Fazekas F (2013) Cerebrovascular complications and granuloma formation after wrapping or coating of intracranial aneurysms with cotton gauze and human fibrin adhesives: results from a single-center patient series over a 5-year period. J Neurosurg 119:1009–1014. https://doi.org/10.3171/2013.6.jns1373
Berger C, Hartmann M, Wildemann B (2003) Progressive visual loss due to a muslinoma—report of a case and review of the literature. Eur J Neurol 10:153–158
Bhatti MT, Holder CA, Newman NJ, Hudgins PA (2000) MR characteristics of muslin-induced optic neuropathy: report of two cases and review of the literature. AJNR Am J Neuroradiol 21:346–352
Bilginer B, Yavuz K, Agayev K, Akbay A, Ziyal IM (2007) Existence of cotton granuloma after removal of a parasagittal meningioma: clinical and radiological evaluation—a case report. Kobe J Med Sci 53:43–47
Brochert A, Reynolds T, Baker R (2003) MRI in a case of muslin-induced granuloma. Neuroradiology 45:82–84. https://doi.org/10.1007/s00234-002-0896-6
Carney PG, Oatey PE (1983) Muslin wrapping of aneurysms and delayed visual failure. A report of three cases. J Clin Neuro-Ophthalmo 3:91–96
Chambi I, Tasker RR, Gentili F, Lougheed WM, Smyth HS, Marshall J, Young I, Deck J, Shrubb J (1990) Gauze-induced granuloma ("gauzoma"): an uncommon complication of gauze reinforcement of berry aneurysms. J Neurosurg 72:163–170. https://doi.org/10.3171/jns.1990.72.2.0163
Deng X, Gao F, Zhang D, Zhang Y, Wang R, Wang S, Cao Y, Zhao Y, Pan Y, Liu X, Zhang Q, Zhao J (2017) Direct versus indirect bypasses for adult ischemic-type moyamoya disease: a propensity score-matched analysis. J Neurosurg:1–7. doi:https://doi.org/10.3171/2017.2.jns162405
Deshmukh VR, Kakarla UK, Figueiredo EG, Zabramski JM, Spetzler RF (2006) Long-term clinical and angiographic follow-up of unclippable wrapped intracranial aneurysms. Neurosurgery 58:434–442; discussion 434-442. https://doi.org/10.1227/01.neu.0000199158.02619.99
Felsberg GJ, Tien RD, Haplea S, Osumi AK (1993) Muslin-induced optic arachnoiditis (“gauzoma”): findings on CT and MR. J Comput Assist Tomogr 17:485–487
Fujimura M, Nishijima M, Umezawa K, Hayashi T, Mino Y, Sakuraba T, Midorikawa H (2003) Optochiasmal arachnoiditis following cotton wrapping of anterior communicating artery aneurysm treated by surgical removal of granuloma. J Clin Neurosci: Off J Neurosurg Soci Australasia 10:254–257
Goldsberry DH, Ross IB, Dhillon G, Corbett JJ (2004) Visual dysfunction caused by gauze wrapping of an intracranial aneurysm. J Neuro-Ophthalmol: Off J North Am Neuro-Ophthalmol Soc 24:42–45
Haisa T, Matsumiya K, Yoshimasu N, Kuribayashi N (1990) Foreign-body granuloma as a complication of wrapping and coating an intracranial aneurysm. Case report. J Neurosurg 72:292–294. https://doi.org/10.3171/jns.1990.72.2.0292
Kim YB, Hong CK, Chung J, Joo JY, Huh S-K (2014) Long-term clinical and angiographic outcomes of wrap-clipping strategies for unclippable cerebral aneurysms. Yonsei Med J 55:401–409. https://doi.org/10.3349/ymj.2014.55.2.401
Kirollos RW, Tyagi AK, Marks PV, van Hille PT (1997) Muslin induced granuloma following wrapping of intracranial aneurysms: the role of infection as an additional precipitating factor. Acta Neurochir 139:411–415. https://doi.org/10.1007/bf01808876
Kumar R, Nadarajah J, Kumar A, Gamanagatti S (2016) Misery of neurosurgeon: gauzoma causing foreign body granuloma-role of radiologist. Asian J Neurosurg 11:74–75. https://doi.org/10.4103/1793-5482.165797
Lee AG, Cech DA, Rose JE, Goodman JC, Haykal HA (1997) Recurrent visual loss due to muslin-induced optochiasmatic arachnoiditis. Neuro-Ophthalmology 18:199–204. https://doi.org/10.3109/01658109709014422
Marcus AO, Demakas JJ, Ross HA, Duick DS, Crowell RM (1986) Optochiasmatic arachnoiditis with treatment by surgical lysis of adhesions, corticosteroids, and cyclophosphamide: report of a case. Neurosurgery 19:101–103
McFadzean RM, Hadley DM, McIlwaine GG (1991) Optochiasmal arachnoiditis following muslin wrapping of ruptured anterior communicating artery aneurysms. J Neurosurg 75:393–396. https://doi.org/10.3171/jns.1991.75.3.0393
Onoue H, Abe T, Tashibu K, Suzuki T (1992) Two undesirable results of wrapping of an intracranial aneurysm. Neurosurg Rev 15:307–309
Perrini P, Montemurro N, Caniglia M, Lazzarotti G, Benedetto N (2015) Wrapping of intracranial aneurysms: single-center series and systematic review of the literature. Br J Neurosurg 29:785–791. https://doi.org/10.3109/02688697.2015.1071320
Prabhu SS, Keogh AJ, Parekh HC, Perera S (1994) Optochiasmal arachnoiditis induced by muslin wrapping of intracranial aneurysms. A report of two cases and a review of the literature. Br J Neurosurg 8:471–476
Repka MX, Miller NR, Penix JO, Trant JH 3rd (1984) Optic neuropathy from the use of intracranial muslin. J Clin Neuro-Ophthalmol 4:147–150
Sachs E Jr (1972) The fate of muscle and cotton wrapped about intracranial carotid arteries and aneurysms. A laboratory and clinico-pathological study. Acta neurochirurgica 26:121–137
Scott RM, Smith ER (2009) Moyamoya disease and Moyamoya syndrome. N Engl J Med 360:1226–1237. https://doi.org/10.1056/NEJMra0804622
Slater LA, Chandra RV, Holt M, Danks A, Chong W (2014) Long-term MRI findings of muslin-induced foreign body granulomas after aneurysm wrapping. A report of two cases and literature review. Interv Neuroradiol 20:67–73. https://doi.org/10.15274/inr-2014-10010
Subramanian PS, Miller NR, Renard V, Tamargo RJ (2005) Delayed progressive visual loss following wrapping of bilateral clinoidal aneurysms: recovery of vision and improvement in neuroimaging during corticosteroid treatment. Br J Ophthalmol 89:1666–1668. https://doi.org/10.1136/bjo.2005.078626
Taravati P, Lee AG, Bhatti MT, Lewis SB (2006) That's a wrap. Surv Ophthalmol 51:434–444. https://doi.org/10.1016/j.survophthal.2006.04.006
Tomsak RL (1985) Muslin optic neuropathy. J Neuroophthalmol 5:71
Yoon MA, Kim E, Kwon BJ, Kim JE, Kang HS, Park JH, Sohn CH, Kim JH, Lee DH (2010) Muslinoma and muslin-induced foreign body inflammatory reactions after surgical clipping and wrapping for intracranial aneurysms: imaging findings and clinical features. J Neurosurg 112:640–647. https://doi.org/10.3171/2009.7.jns081625
Funding
The United Hospital Foundation provided financial support in the form of grant funding. The sponsor had no role in the design of conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comments
This is an instructive case report, well-documented and presented, of a gauze ball that developed and became highly symptomatic around a miniscule unruptured MCA aneurysm. There are several educational points that we can take away.
1. The placement of extravascular foreign material is not always benign. In this case, a 6 mm PCoA UIA was clipped electively (I would agree with this), and a minuscule (0.5 mm) MCA blip was layered with gauze at the same operation. I freely admit that I have done this too, many years past. In light of current data, however, we must question whether anything at all should have been done at the MCA location, especially in consideration of the consequences to this patient, who developed seizures and hemiparesis and had three major craniotomies, all when she never had any SAH or clinical problem at all. Foreign material is just that we usually get away with it, but the strategy of prophylactic aneurysm wrapping is not benign, as we can see here.
2. The patient had an aggressive revascularization strategy based on vessel imaging. I understand that she had hemiparesis and that her STA was surgically absent. For my part, however, the clinical workup and the justification for saphenous vein bypass would have been strengthened by the acquisition of perfusion data, which is not presented here. This would improve the value of this case report as well.
It is, in sum, an interesting case and illustrates well that no good deed goes unpunished.
Christopher M. Loftus
Philadelphia, PA, USA
Rights and permissions
About this article
Cite this article
Nussbaum, E.S., Kallmes, K.M., Lowary, J. et al. Surgical treatment of a gauzoma with associated obliterative arteriopathy and review of the literature. Acta Neurochir 160, 1195–1202 (2018). https://doi.org/10.1007/s00701-017-3440-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-017-3440-5