Abstract
Background
Carotid rete mirabile (RM) is a meshwork of multiple, freely intercommunicating arterioles that reconstitute the absent or hypoplastic segments of the internal carotid artery (ICA). Carotid RM has been reported to be associated with cerebrovascular diseases. However, it is rarely associated with moyamoya-pattern collateral vessels in the posterior cerebral artery (PCA) region and aneurysm.
Case presentation
A 39-year-old woman was admitted complaining of sudden-onset headache, nausea, and vomiting. Further investigation revealed subarachnoid hemorrhage (SAH), carotid RM, a moyamoya collateral pattern in the PCA region, and a pseudoaneurysm in the moyamoya-like vessels. The patient was treated conservatively, recovered well and was discharged 1 week later. Follow-up angiography showed that the aneurysm had disappeared.
Conclusions
As shown by the present case, we believe that carotid RM could occur in combination with moyamoya-pattern collateral vessels in the PCA region; aneurysms can occur in the moyamoya-like vascular network. Congenital etiology may be the reason for these combinations. Based on our approach in this case, aneurysm located in moyamoya-like vessels can disappear spontaneously after conservative treatment.
Similar content being viewed by others
Background
Carotid rete mirabile (RM), which is often found in lower mammals such as pigs and sheep and rarely occurs in humans, is a meshwork of multiple, freely intercommunicating arterioles that reconstitute the absent or hypoplastic segments of the internal carotid artery (ICA) [1]. Carotid RM has been reported to be associated with cerebrovascular diseases [1, 2]. However, it is rarely associated with a moyamoya-like collateral pattern of cerebral arteries.
Moyamoya-pattern collateral vessels mainly occur in the middle cerebral artery (MCA) region, presenting with characteristic hypertrophy and proliferation of the small arteries; these vessels serve as collateral channels to bypass occlusions [3, 4]. Rarely, the posterior cerebral artery (PCA) is also involved in moyamoya-pattern collateral vessels [5]. Aneurysms can occur in moyamoya-pattern collateral vessels [6]. The natural history of aneurysms in moyamoya-pattern collateral vessels is uncertain.
Here, we report a rare case of a patient who presented with carotid RM, moyamoya-pattern collateral vessels in the PCA region and an aneurysm that was located in the collateral network. The aneurysm regressed after conservative treatment. The combination of carotid RM, moyamoya-pattern collateral vessels in the PCA region and aneurysm is discussed in the paper.
Case presentation
A 39-year-old woman was admitted complaining of sudden-onset headache, nausea, and vomiting for 1 day. She had a history of hypertension for 10 years and denied any history of diabetes, hyperlipidemia, autoimmune diseases, or other remarkable illnesses. She was alert and could correctly obey commands. Physical examination was unremarkable except for neck stiffness. Her blood glucose, electrolytes, blood cell counts, coagulation test, and antinuclear antibody series were within normal limits during laboratory investigations.
Head computed tomography (CT) showed a subarachnoid hemorrhage (SAH) concentrated in the perimesencephalic cistern (Fig. 1a). CT angiography (CTA) showed that the bilateral ICAs were absent in the skull base (Fig. 1b-c). The bilateral MCAs and anterior arteries were normal. An aneurysm was identified in the PCA region (Fig. 1d).
a: A head CT scan shows an SAH concentrated in the perimesencephalic cistern. b-c: CTA shows that the cavernous portion of the bilateral internal carotid arteries (ICAs) is absent (asterisks). The bilateral middle cerebral arteries and anterior arteries are normal. d: An aneurysm is identified in the PCA region. Abbreviations: CT: computed tomography, SAH: subarachnoid hemorrhage, CTA: CT angiography, ICA: internal carotid artery, PCA: posterior cerebral artery
Head digital subtraction angiography (DSA) showed that the bilateral internal maxillary arteries and ascending pharyngeal arteries were confluent with the cavernous portion of the ICAs at the skull base. And the bilateral ICAs above the cavernous portion of the ICAs, the MCAs, and the anterior cerebral arteries were normal (Fig. 2). The right vertebral artery (VA) was fine, while the left VA was well developed (Fig. 3a-b). Moyamoya-pattern collateral vessels could be seen in the bilateral PCAs region, the distal part of the PCA was composed of abnormally fine vessels, and an aneurysm was clearly identified in the left moyamoya-pattern collateral vessels (Fig. 3c-d).
a-b: Left common carotid artery DSA in AP and lateral views shows that the internal maxillary artery and ascending pharyngeal artery of the external carotid artery are confluent with the cavernous portion of the ICA at the skull base. And the ICA above the cavernous portion segment, middle cerebral artery, and anterior cerebral artery are normal in shape and direction. c-d: The findings of right common carotid artery DSA are similar to those of the left common carotid artery. Abbreviations: AP: anteroposterior, DSA: digital subtraction angiography, ICA: internal carotid artery
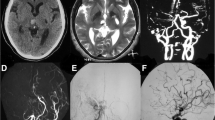
a-b: Right subclavian artery angiogram shows the right VA is slender. Left subclavian artery angiogram shows the left VA is well developed. c-d: Left VA angiogram in AP and lateral views shows that the left VA is extended tortuously to the basilar artery; the distal vessels of the bilateral PCAs are fine or even absent, and the capillaries around this area have compensatory hyperplasia. An aneurysm is clearly visible in the left moyamoya-pattern collateral vessels (arrows). Abbreviations: AP: anteroposterior, PCA: posterior cerebral artery, VA: vertebral artery
She was diagnosed as bilateral carotid RM, moyamoya-like vessels in the PCA region, intracranial pseudoaneurysm, and SAH. Management of the aneurysm was difficult, and wait and see management was adopted. The patient experienced an uneventful recovery and was discharged 1 week later. Follow-up CT performed 44 days later showed complete resolution of the SAH (Fig. 4a-b). Head DSA revealed that the pseudoaneurysm disappeared spontaneously while the moyamoya-pattern collateral vessels were unchanged, the distal part of the PCAs became finer and smaller, and the transdural compensation of the posterior meningeal artery was visible (Fig. 4c-d). The patient was in good condition during follow-up, she returned to her normal activities.
a-b: CT shows complete resolution of the SAH. c-d: Left VA angiogram in AP and lateral views reveals that the aneurysm have disappeared, the distal part of the PCAs become finer and smaller, and the transdural compensation of the posterior meningeal artery could be seen. Abbreviations: AP: anteroposterior; CT: computed tomography, SAH: subarachnoid hemorrhage, PCA: posterior cerebral artery, VA: vertebral artery
Discussion and conclusion
Carotid RM refers to a meshwork of multiple, freely intercommunicating fine arteries or arterioles that reconstitute the absent or hypoplastic segments of the ICA and is often found in lower mammals [1]. In rare cases, humans can also develop carotid RM. The diagnostic criteria for carotid RM include the following: 1) a hypoplastic ICA, 2) an arterial plexus between the maxillary artery and the cavernous portion of the ICA; 3) a dilated ophthalmic artery (OA); 4) a supraclinoid ICA that is not hypoplastic and is fed by the arterial plexus and the OA; 5) bilateral lesions; and 6) no abnormal vessels, such as moyamoya-like vessels, in the intradural circulation [7, 8]. The case reported in this paper met all of the carotid RM diagnostic criteria.
Carotid RM has been reported to be associated with many cerebrovascular diseases, such as intracranial aneurysm, arteriovenous malformation, pial arteriovenous fistula, carotid-cavernous fistula, and Galen aneurysmal malformation [1, 2, 9, 10]. However, carotid RM is rarely associated with a moyamoya-pattern collateral vessels of the posterior circulation. Moyamoya-pattern collateral vessels mainly occur in the MCA region [3, 4]. Rarely, the PCA could be also involved in moyamoya-pattern collateral vessels, as in our case [5].
The reasons that concomitant cerebrovascular diseases are associated with carotid RM are unclear. Currently, these combinations are thought to arise from congenital embryonic etiologies [11]. Therefore, congenital etiology may also be the reason that carotid RM was associated with a moyamoya-pattern collateral vessels of the PCA in our case.
Most patients with isolated moyamoya-pattern collateral vessels do not have severe perfusion impairment [3]. In our case, the moyamoya-pattern collateral vessels were visible in the bilateral PCAs region, and the transdural compensation from the posterior meningeal artery to the distal part of the PCA was also visible. Due to the sufficient collateral circulation, the CT scan did not show signs of ischemia in the territory of vertebrobasilar artery system (Figs. 1 and 4). The posterior meningeal artery transdural anastomosis observed in our case is rare, and the compensation pattern was the same as that seen in the middle meningeal artery in moyamoya disease [12, 13].
When moyamoya-pattern collateral vessels occur in the PCA region, the rich moyamoya-like vascular network may be associated with an unfavorable outcome because these expanded moyamoya-like vessels endure higher hemodynamic stress, which can easily result in aneurysm formation [14, 15]. These aneurysms can easily rupture. The complex anatomy increases the difficulty of treating aneurysms located in the moyamoya-like vascular network. Although successful treatment has been reported, the risk is very high [6, 16].
It is uncertain whether aneurysms in moyamoya-pattern collateral vessels should be treated due to a lack of understanding of their natural history. Kawaguchi et al. reported that these aneurysms of the moyamoya-like vascular network can disappear spontaneously after the initial bleeding episode [15]. Our previous study also found that pseudoaneurysms can disappear after conservative treatment [17]. Because of the uncertainty regarding the natural history of aneurysms in moyamoya-like vessels, we chose conservative treatment for our patient. The aneurysm had disappeared on follow-up DSA performed at 44 days later.
As shown by the present case, we believe that carotid RM can occur combined with moyamoya-pattern collateral vessels in the PCA region. And aneurysms can occur in the moyamoya-like vascular network. Furthermore, based on our approach in this case, aneurysms located in moyamoya-like vessels can also disappear spontaneously after conservative treatment.
Abbreviations
- CT:
-
Computed tomography
- CTA:
-
CT angiography
- DSA:
-
Digital subtraction angiography
- ICA:
-
Internal carotid artery
- MCA:
-
Middle cerebral artery
- OA:
-
Ophthalmic artery
- PCA:
-
Posterior cerebral artery
- RM:
-
Rete mirabile
- SAH:
-
Subarachnoid hemorrhage
- VA:
-
Vertebral artery
References
Xu K, Yu TC, Wang X, Yu JL. Bilateral carotid and vertebral rete mirabile associated with intracranial multiple hemorrhages: a case report and literature review. Int J Clin Exp Med. 2016;9:12153–62.
Mondel PK, Saraf R, Limaye US. Bilateral carotid and vertebral rete mirabile with vein of Galen aneurysmal malformation: an unreported association. J Neurointerv Surg. 2016;8:e1.
Derdeyn CP, Zipfel GJ, Zazulia AR, Davis PH, Prabhakaran S, Ivan CS, et al. Baseline hemodynamic impairment and future stroke risk in adult idiopathic Moyamoya phenomenon: results of a prospective natural history study. Stroke. 2017;48:894–9.
Rivera R, Sordo J, Badilla L, Bravo E, Riveros R, Giacaman P. Middle cerebral artery occlusion with moyamoya-like vessels and aneurysms. A report of two cases. Interv Neuroradiol. 2014;20:96–9.
Rahme R, Crevier L, Dubois J, Mercier C. Moyamoya-like vasculopathy and Seckel syndrome: just a coincidence? Childs Nerv Syst. 2010;26:983–6.
Lang M, Moore NZ, Witek AM, Kshettry VR, Bain MD. Microsurgical repair of ruptured aneurysms associated with moyamoya-pattern collateral vessels of the middle cerebral artery: a report of two cases. World Neurosurg. 2017;105:1042 e5–e10.
Verma A, Pendharkar H, Prasad C. Rete mirabile of the ICA: report of three cases. Interv Neuroradiol. 2018;24:586–90.
Itoyama Y, Kitano I, Ushio Y. Carotid and vertebral rete mirabile in man--case report. Neurol Med Chir (Tokyo). 1993;33:181–4.
Mondel PK, Saraf R, Limaye US. Rete mirabile associated with pial arteriovenous fistula: imaging features with literature review. BMJ Case Rep. 2017;2017. https://doi.org/10.1136/bcr-2016-012939.
Paschoal EH, Yamaki VN, Junior FM, Piske RL, Teixeira MJ, Bor-Seng-Shu E. Carotid rete mirabile associated with subarachnoid hemorrhage from intracranial aneurysm: a case report and systematic review. Interv Neuroradiol. 2015;21:55–60.
Mondel PK, Saraf R, Limaye US. Rete mirabile associated with pial arteriovenous fistula: imaging features with literature review. J Neurointerv Surg. 2017;9:e36.
Hou K, Guo Y, Xu B, Xu K, Yu J. Delayed establishment of collateral circulation from posterior meningeal artery after proximal occlusion of posterior inferior cerebellar artery: case report and literature review. World Neurosurg. 2018;115:334–7.
Yu J, Guo Y, Xu B, Xu K. Clinical importance of the middle meningeal artery: a review of the literature. Int J Med Sci. 2016;13:790–9.
Yeon JY, Kim JS, Hong SC. Incidental major artery aneurysms in patients with non-hemorrhagic moyamoya disease. Acta Neurochir. 2011;153:1263–70.
Kawaguchi S, Sakaki T, Morimoto T, Kakizaki T, Kamada K. Characteristics of intracranial aneurysms associated with moyamoya disease. A review of 111 cases. Acta Neurochir (Wien). 1996;138:1287–94.
Zhang L, Xu K, Zhang Y, Wang X, Yu J. Treatment strategies for aneurysms associated with moyamoya disease. Int J Med Sci. 2015;12:234–42.
Yu JL, Wang HL, Xu K, Li Y, Luo Q. Endovascular treatment of intracranial aneurysms associated with moyamoya disease or moyamoya syndrome. Interv Neuroradiol. 2010;16:240–8.
Acknowledgements
None.
Funding
None.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Conception and design: HC, KH. Acquisition of data: XW. Analysis and interpretation of data: KH, KX. Drafting of the article: KH, JY. Critical revision of the article: JY, KX. KH and HC contributed equally to this work and should be considered as co-first authors. All of the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of The First Hospital of Jilin University, and informed written consent was obtained from the patient.
Consent for publication
Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chen, H., Hou, K., Wang, X. et al. Spontaneous recession of a posterior cerebral artery aneurysm concurrent with carotid rete mirabile and moyamoya-pattern collateral vessels: a case report. BMC Neurol 19, 51 (2019). https://doi.org/10.1186/s12883-019-1277-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12883-019-1277-7