Abstract
Background
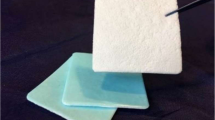
We analyze our experience of using TachoSil® (Takeda Austria GmbH: Linz, Austria) in microneurosurgical procedures as a hemostat and also as a sealant to patch dural defects.
Materials and methods
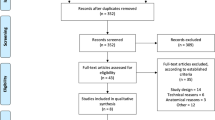
Beginning on January 1, 2012, we prospectively analyzed 100 consecutive surgeries where TachoSil was used. The patient group included 58 women (58 %) and 42 men (42 %); the mean age was 52 years (range, 3–85 years). Indications for surgery included removal of the tumor (53 cases; 53 %), clipping of the cerebral arterial aneurysm (31 cases; 31 %), and treatment of other pathologies, including AVM (four cases; 4 %), cavernomas (four cases; 4 %), spinal tumor, and traumatic subdural hematoma. Patients received postoperative care according to local neurosurgical department protocol, including a postoperative CT scan after each craniotomy. Primary assessment of the wound took place during the hospital stay as well as at discharge or transfer to a rehabilitation unit. Mean follow-up time was 4 months (range, 1–12 months).
Results
None of the patients developed postoperative hematoma after craniotomy or spinal procedure. At primary assessment during hospital stay, 93 patients (93 %) had had no wound-related problems over the normal course of healing. No case registered any liquor leak from the wound, and none of the patients showed any signs of allergic response related to TachoSil usage. At the last follow-up, 96 patients (96 %) experienced uneventful wound healing, and in four patients (4 %), superficial wound infection was successfully treated with oral antibiotics.
Conclusions
Our results indicate that TachoSil can serve in neurosurgical practice at no additional risks. TachoSil proved to be an effective hemostat, sealant, and adhesive in either cranial or spinal procedures.
Similar content being viewed by others
References
Barth M, Tuettenberg J, Thome C, Weiss C, Vajkoczy P, Schmiedek P (2008) Watertight dural closure: is it necessary? A prospective randomized trial in patients with supratentorial craniotomies. Neurosurgery 63:352–8, discussion 358
Berdajs D, Burki M, Michelis A, von Segesser LK (2010) Seal properties of TachoSil: in vitro hemodynamic measurements. Interact Cardiovasc Thorac Surg 10:910–913
Bock HC, Cohnen J, Keric N, Kantelhardt SR, Giese A (2011) Occlusion of surgical opening of the ventricular system with fibrinogen-coated collagen fleece: a case collection study. Acta Neurochir (Wien) 153:533–539
Boogaarts JD, Grotenhuis JA, Bartels RH, Beems T (2005) Use of a novel absorbable hydrogel for augmentation of dural repair: results of a preliminary clinical study. Neurosurgery 57:146–51, discussion 146–51
Cappabianca P, Cavallo LM, Valente V, Romano I, D’Enza AI, Esposito F, de Divitiis E (2004) Sellar repair with fibrin sealant and collagen fleece after endoscopic endonasal transsphenoidal surgery. Surg Neurol 62:227–33, discussion 233
Celiento M, Scioti G, Pratali S, Bortolotti U (2010) Repair of coronary artery perforation following angioplasty using TachoSil patches. Interact Cardiovasc Thorac Surg 10:328–330
Chauvet D, Tran V, Mutlu G, George B, Allain JM (2011) Study of dural suture watertightness: an in vitro comparison of different sealants. Acta Neurochir (Wien) 153:2465–2472
Dusick JR, Mattozo CA, Esposito F, Kelly DF (2006) BioGlue for prevention of postoperative cerebrospinal fluid leaks in transsphenoidal surgery: a case series. Surg Neurol 66:371–6, discussion 376
Fuglsang K, Dueholm M, Staehr-Hansen E, Petersen LK (2012) Uterine healing after therapeutic intrauterine administration of TachoSil (hemostatic fleece) in cesarean section with postpartum hemorrhage caused by placenta previa. J Pregnancy 2012:635683
Grau AE, Duran JA (2012) Treatment of a large corneal perforation with a multilayer of amniotic membrane and TachoSil. Cornea 31:98–100
Haas S (2006) The use of a surgical patch coated with human coagulation factors in surgical routine: a multicenter postauthorization surveillance. Clin Appl Thromb Hemost 12:445–450
Horowitz B, Busch M (2008) Estimating the pathogen safety of manufactured human plasma products: application to fibrin sealants and to thrombin. Transfusion 48:1739–1753
Hutter G, von Felten S, Sailer MH, Schulz M, Mariani L (2014) Risk factors for postoperative CSF leakage after elective craniotomy and the efficacy of fleece-bound tissue sealing against dural suturing alone: a randomized controlled trial. J Neurosurg 121:735–744
Kivelev J, Hernesniemi J (2013) Four-fold benefit of wound closure under high magnification. Surg Neurol Int 4:115-7806.118171, eCollection 2013
Kumar A, Maartens NF, Kaye AH (2003) Evaluation of the use of BioGlue in neurosurgical procedures. J Clin Neurosci 10:661–664
Lehecka M, Laakso A, Hernesniemi J (2011) Helsinki microneurosurgery basics and tricks. Aesculap AG, Germany
Maisano F, Kjaergard HK, Bauernschmitt R, Pavie A, Rabago G, Laskar M, Marstein JP, Falk V (2009) TachoSil surgical patch versus conventional haemostatic fleece material for control of bleeding in cardiovascular surgery: a randomised controlled trial. Eur J Cardiothorac Surg 36:708–714
Nistor RF, Chiari FM, Maier H, Hehl K (1997) The fixed combination of collagen with components of fibrin adhesive-a new hemostypic agent in skull base procedures. Skull Base Surg 7:23–30
Pilone V, Di Micco R, Monda A, Villamaina E, Forestieri P (2012) Use of Tachosil(R) in bariatric surgery: preliminary experience in control of bleeding after sleeve gastrectomy. Minerva Chir 67:241–248
Pocar M, Passolunghi D, Bregasi A, Donatelli F (2012) TachoSil for postinfarction ventricular free wall rupture. Interact Cardiovasc Thorac Surg 14:866–867
Reddy M, Schoggl A, Reddy B, Saringer W, Weigel G, Matula C (2002) A clinical study of a fibrinogen-based collagen fleece for dural repair in neurosurgery. Acta Neurochir (Wien) 144:265–9, discussion 269
Rickenbacher A, Breitenstein S, Lesurtel M, Frilling A (2009) Efficacy of TachoSil a fibrin-based haemostat in different fields of surgery–a systematic review. Expert Opin Biol Ther 9:897–907
Santulli P, Marcellin L, Touboul C, Ballester M, Darai E, Rouzier R (2011) Experience with TachoSil in obstetric and gynecologic surgery. Int J Gynaecol Obstet 113:112–115
Simo KA, Hanna EM, Imagawa DK, Iannitti DA (2012) Hemostatic agents in hepatobiliary and pancreas surgery: a review of the literature and critical evaluation of a novel carrier-bound fibrin sealant (TachoSil). ISRN Surg 2012:729086
Than KD, Baird CJ, Olivi A (2008) Polyethylene glycol hydrogel dural sealant may reduce incisional cerebrospinal fluid leak after posterior fossa surgery. Neurosurgery 63:ONS182-6, discussion ONS186-7
Toro A, Mannino M, Reale G, Di Carlo I (2011) TachoSil use in abdominal surgery: a review. J Blood Med 2:31–36
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
The authors’ experience with TachoSil matches that of our department. We too have used TachoSil extensively over the last 2 years in a similar range of operations, mainly for dural repair and as a cover for mastoid air cells. In addition, we have found it useful for sealing “weeping” arachnoid in transsphenoidal procedures. The surgical closure time is markedly reduced and the need for various patches is obviated. The authors also describe their experience with TachoSil for tumor bed hemostasis and how to avoid inadvertent detachment of the material, a technique that I am looking forward to trying. The safety profile of TachoSil appears to be sound, including the appropriate caveats of the authors. We must, however, remember that this series is anecdotal. Comparative studies to other dural closure techniques will be difficult and costly to organize due to the low incidence of CSF leakage in most supratentorial procedures. Infratentorial craniotomies that have a higher incidence of CSF complications may serve in a comparative evaluation of the utility of the product in the future. The high price of the product does limit its routine usage, though the company will soon be providing smaller patches at a lower price.
Zvi Harry Rappaport
Petah Tiqva, Israel
When I first saw the title of this article, I believed this was a topic that was covered extensively already. Rather surprisingly, I found that it is not. In the present article, the authors simply give us an account of their experience with the use of TachoSil, which appears to be of value for avoiding CSF leaks and in the closure of openings of the ventricular wall, etc. In my opinion, the most valuable information lies in the many practical tricks and tips they present in the Discussion section, e.g., on how to handle the pieces of sealant in the field.
Knut Wester
Oslo, Bergen
Rights and permissions
About this article
Cite this article
Kivelev, J., Göhre, F., Niemelä, M. et al. Experiences with TachoSil® in microneurosurgery. Acta Neurochir 157, 1353–1357 (2015). https://doi.org/10.1007/s00701-015-2473-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2473-x